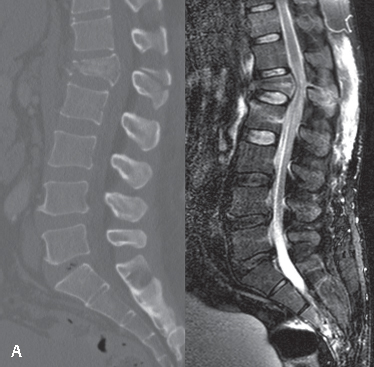
13 Flexion-distraction injuries in the thoracolumbar spine are classically referred to as “seat belt injuries” or Chance fractures. They comprise 5–15% of thoracolumbar fractures. The most common mechanism is a motor vehicle accident in which a lap belt acts as an axis of rotation anterior to the spinal column, causing failure of the spinal column in tension. If the center of rotation involves the anterior portion of the spinal column, it may fail either in compression or in tension. Upwards of 50–60% of patients will suffer concomitant abdominal visceral injuries, which require a high level of suspicion and judicious management by trauma personnel. Fractures with the aforementioned mechanism involving the bony spinal elements with the axis of rotation anterior to the spine have been given the eponym “Chance fractures” after G. Q. Chance, the first physician to report on this particular pattern of injury.1 Specifically, Chance noted that in several cases the vertebral body was relatively incompressible and, as he stated, “something has to give way,” referring to the posterior bony structures. A traditional Chance fracture involves a horizontal splitting of the vertebra that begins with the spinous process or lamina and extends anteriorly through the pedicles and vertebral body. Several classification schemes have been proposed. However, inter- and intra-observer reliability, as well as prognostic value, have been lacking in most cases. In 2005, the Spine Trauma Study Group introduced the Thoracolumbar Injury Classification and Severity Score (TLICS) in an attempt to address the shortcomings of previous methods of classification.2 Injury morphology, neurologic status, and posterior ligamentous complex integrity were all taken into account, and operative versus nonoperative management was proposed based on the severity of injury. Of relevance to flexion-distraction injuries, in this system, distraction injuries receive the maximal amount of points (4/4) in the morphology category and disruption of the posterior ligamentous complex receives 3/3, again, the maximal amount of points, in its category. Surgical treatment is recommended for a point total greater than 4. Recent evidence suggests that this system can reliably be used to predict surgical management.3 Other classification systems that are more specific to flexion-distraction injuries have been described. Denis divided these injuries into four types: (A) one-level injury, primarily bony; (B) one-level injury, primarily soft tissue (i.e., ligamentous and disk); (C) two-level injury, primarily bony, through the posterior vertebral body; and (D) two-level injury, primarily soft tissue, through the posterior vertebral body. A classification system based on the posterior starting point and symmetry of the fracture was described by Gumley et al.4 There were three types. Type I fractures start in the spinous process and are symmetrical. Type II fractures start at the base of the spinous process and are symmetrical. Type III fractures are asymmetrical, and the fracture plane is not parallel to the endplates. Gertzbien and Court-Brown expanded upon Gumley’s classification to incorporate the exit point of the fracture and the degree to which the vertebral body was involved.4 In this scheme, fractures were first classified as I, II, or III based on Gumley’s system, and then further classified into subgroups A through E: (A) fracture exits through disk, (B) fracture exits through anterior vertebral body wall, (C1) superior endplate involved, (C2) inferior endplate involved, (D) anterior vertebral body compression, (E) burst component. Flexion-distraction injuries most commonly occur during motor vehicle accidents or falls. It is important to elucidate whether the patient was wearing a seat belt and whether it was a simple lap belt or a belt including a shoulder harness. These injuries are classically associated with lap belt use, though today many injuries occur as a result of other mechanisms, including fall from height. Evaluation by a trauma team is paramount when flexion-distraction injury is suspected to rule out concomitant intraabdominal injury. Classically, with enough force, abdominal wall contusions, known as the “seatbelt sign,” will be noted on inspection, which are predictive of intraabdominal injury. However, recent data suggest that the rate of intraabdominal injury with Chance fractures may previously have been overreported. Tyroch et al. reported only 26/79 (33%) of patients with Chance fracture as having intraabdominal injury. A detailed neurologic exam must be performed by an orthopedic and/or neurosurgical physician. This entails a full motor and sensory exam, reflexes, rectal exam (including tone, sensation, and volition), and upper motor neuron signs such as clonus, Babinski reflex, and Hoffmann sign. Close attention should be paid to posterior spinal “step-off” and/or increased space between spinous processes. Likewise, palpation at the site of injury will often elicit pain. In the setting of spinal shock (temporary loss of reflexes caudal to the level of spinal cord injury), the bulbospongiosus reflex is useful in determining what phase of shock the patient is in. Ditunno et al. proposed four phases.5 The gold standard system with which spinal cord injuries are assessed and classified is that of the American Spinal Injury Association (ASIA). ASIA guidelines for examination and classification are strongly recommended for any suspected injury to the spine. Evaluation begins with an assessment of the bony anatomy, either using plain-film radiography or computed tomography (CT). On plain film, interspinous widening may be seen on both the anteroposterior (AP) and lateral views. Additionally, the lateral view may show some degree of segmental kyphosis. Any translation at the level of the injury on the AP or lateral views should be noted. Any translation is representative of significant instability. If a high level of suspicion exists for a flexion-distraction injury based on plain film, mechanism of injury, or physical exam, a CT scan should be obtained to delineate the pattern of bony anatomy disruption further. Magnetic resonance imaging (MRI) is also typically obtained, especially if there is any evidence on physical examination of a neurologic deficit. The MRI is particularly sensitive in identifying compression of the neural elements and defining the integrity of the soft-tissue structures (i.e., intervertebral disk, facet capsules, interspinous and supraspinous ligaments, ligamentum flavum, and the thoracodorsal fascia). However, recent evidence suggests that in assessing the posterior ligamentous complex of the spine, specificity and positive predictive value are at times poor, ranging from 56% to 67% and 42% to 82%, respectively.6,7 Hence, MRIs may be “over-read” and unnecessary surgery may occur. Injury morphology and neurologic status must be considered when devising a surgical plan. Nonoperative treatment is usually reserved for neurologically intact, primarily bony, flexion-distraction injuries with less than 15° of kyphosis. In these cases, patients may be treated with a simple extension-type cast or orthosis with 85% good to fair results expected.8 Patients should be followed a minimum of 3 months with radiographs obtained at each interval visit to assess maintenance of sagittal alignment. For injuries presenting with greater than 15° of kyphosis, neurologic deficit, or disruption of the posterior ligamentous complex, surgical stabilization is recommended.8 The goal of surgery is to restore the posterior tension band. This can be usually be achieved with a posterior-only approach. The standard approach has been the stabilization of two levels above and two levels below the level of injury with a pedicle screw/rod construct; however, short-segment fixation can be used in flexion-distraction injuries in which there is minimal comminution and/or collapse of the anterior spinal column.9 Injuries that involve significant comminution of the vertebral body have a flexion component with probable disruption of the posterior ligamentous complex. These injuries typically require both long-segment posterior stabilization and anterior corpectomy and fusion with use of a structural bone graft or interbody cage for anterior support. It is vital to review the preoperative imaging studies prior to surgery to determine whether or not there are intervertebral disk or retropulsed vertebral body bone fragments that need to be decompressed at the time of surgery, either from a posterior, transpedicular approach or a combined anterior/posterior approach. Surgical treatment yields satisfactory results in most cases. Finkelstein et al. reported that 88% of patients in which a short construct, spanning one motion segment, was used achieved minimal disability at minimum 20 months’ follow-up.10 In 2005, Tezer et al. reported on 48 patients treated surgically for thoracolumbar burst fractures associated with a flexion-distraction injury of the posterior elements. At mean follow-up of 70 months there was no loss of correction, a satisfactory reduction, and good stabilization with solid fusion achieved in all cases.11 Complications associated with the injury itself include epidural hematoma, neurologic injury, and kyphotic deformity. The most common complication associated with nonoperative management is progression of kyphosis. Complications of surgery include infection, instrumentation failure, pseudarthrosis, loss of correction, neurologic injury, and/or mortality. Fig. 13.1A Sagittal CT and MRI of L1 flexion-distraction injury at initial presentation. This injury was treated nonoperatively.
Thoracolumbar Flexion-Distraction Injuries
![]() Classification
Classification
![]() Workup
Workup
History
Physical Examination
Spinal Imaging
![]() Treatment
Treatment
![]() Outcomes
Outcomes
![]() Complications
Complications
![]() Case Examples
Case Examples
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






