CHAPTER 44 Thoracic Disc Disease
Historical Background
In 1838, Key1 wrote the first report of a thoracic herniated disc causing spinal cord compression. Middleton and Teacher2 reported the second case 73 years later. The first reported surgical treatment of a thoracic herniated disc was in 1922 by Adson, who performed a laminectomy and disc removal.3 In their classic 1934 monograph on ruptured intervertebral discs, Mixter and Barr4 described four cases of thoracic disc herniation; two of three patients treated surgically via laminectomy were rendered paraplegic, emphasizing the challenge in the management of the disease. In the ensuing years, many reports helped define the disease and document that treatment by laminectomy was unpredictable and very risky.3,5–16
The costotransversectomy approach was introduced by Menard17 in 1900. Capener18 later modified the procedure for use in the treatment of Pott disease. At Alexander’s suggestion, Hulme19 was the first to use this approach in the management of a herniated thoracic disc. Hulme19 reported his experience with six patients treated by costotransversectomy and showed that it was a safer, more effective approach than laminectomy. In a later literature review of 49 surgical cases using costotransversectomy, Arce and Dohrmann20 noted 82% of patients improved, the condition was unchanged in 14% of patients, and only 4% of patients experienced worsening of their condition.
Hodgson and Stock21 popularized the anterior approach to the spine for the treatment of Pott disease. In 1958, Crafoord and colleagues22 reported the first transthoracic procedure on the spine for a herniated disc. They performed a fenestration, or windowing of the disc without any attempt at disc removal or cord decompression. The one patient described in their article did well. Simultaneous reports by Perot and Munro23 and Ransohoff and colleagues24 in 1969 established transthoracic spinal cord decompression as a viable alternative to costotransversectomy. The posterolateral approach to the thoracic disc space was described by Carson and colleagues25 in 1971 and was modified by Patterson and Arbit26 in 1978.
All the surgical approaches have undergone minor modifications, including the application of microsurgical techniques.27–29 Developments in the use of video-assisted thoracoscopic surgery (VATS) have provided an additional option in surgical treatment of a symptomatic thoracic herniated disc.30–33 Each technique has advantages and disadvantages, and all but laminectomy are currently acceptable.
The diagnostic use of MRI has had a profound influence on the treatment of thoracic disc herniation.34–42 At most centers, MRI has replaced myelography as the standard for the diagnosis of this condition. Because MRI is rapid, noninvasive, and increasingly available, its use is likely to decrease delay in diagnosis and lead to earlier treatment and perhaps improved prognosis. A new challenge is likely to be avoiding overdiagnosis and unnecessary operations on asymptomatic lesions.41,43
Epidemiology
The true incidence of thoracic herniated discs is unknown; many cases are unrecognized, or patients are asymptomatic. Most patients are in the 4th through 6th decades of life (Fig. 44–1).3,6,44,45 In a review of 288 cases reported in the literature, Arce and Dohrmann44 noted a slight male preponderance (1.5:1), although most series show an approximately even sex distribution.5,11,46,47 Cases have been reported in patients ranging in age from 11 to 75 years.25,48,49
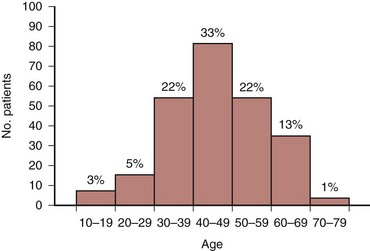
FIGURE 44–1 Distribution of 280 cases of thoracic disc herniation according to age.
(From Arce CA, Dohrmann GJ: Herniated thoracic disks. Neurol Clin 3:383-392, 1985.)
Historically, only 0.15% to 4% of all symptomatic protrusions of an intervertebral disc are in the thoracic spine.3,5,6,12,44,50–52 Surgically, thoracic disc excision accounts for 0.2% to 1.8% of all operations performed on symptomatic herniated discs.5,29,39,44,53–56 In 1950, Love and Kiefer47 reported on 17 cases seen over 26 years. Logue12 reported a thoracic herniated disc in 11 of 250 discectomies (4%). Otani and colleagues51 later reported symptomatic thoracic disc herniation in 15 of 857 discectomies (1.8%) over a 15-year period. In a cadaveric study, Haley and Perry57 showed that 11% of unselected autopsies revealed protruded thoracic discs; 2 of 99 specimens in their series had discs protruding 4 to 7 mm into the canal. The prevalence of herniated thoracic discs with an associated neurologic deficit has been estimated to be 1 per 1 million population.25,42,47,52,58
Improvements in imaging techniques have resulted in an increased detection of thoracic abnormalities and, concurrently, of herniated thoracic discs. Ryan and colleagues59 reviewed 270 patients undergoing computed tomography (CT) of the thorax for suspected malignancy and found 4 (1.5%) who had asymptomatic calcified herniated thoracic discs. In a retrospective review of combined CT and myelography in 360 patients, Awwad and colleagues60 found 54 herniations of a thoracic disc in 40 patients (11%) who were asymptomatic. In their study, 88% of the asymptomatic thoracic discs showed some deformity of the spinal cord; there was no single feature or combination of features clearly separating asymptomatic from symptomatic thoracic herniated discs.
The advent of MRI and its inherent sensitivity has increased further the reported incidence of thoracic disc herniations. Williams and colleagues41 retrospectively reviewed 48 patients who underwent MRI for oncologic evaluation and reported a thoracic herniated disc in 7 (15%). Ross and colleagues39 diagnosed 20 cases (16 confirmed) by MRI in a 2-year period compared with the initial report of Love and Kiefer47 in 1949 of 17 cases seen over a 26-year period. Wood and colleagues42 reported 66 of 90 asymptomatic individuals (73%) had positive anatomic findings at one or more thoracic levels; findings included herniation of a disc in 33 subjects (37%), bulging of a disc in 48 (53%), an annular tear in 52 (58%), and deformation of the spinal cord in 26 (29%). Wood and colleagues42 reported no association between age and the prevalence of disc herniation. Compared with the MRI findings of 18 patients treated operatively for thoracic disc herniations in their study, the overall prevalence of these findings in the group that had thoracic pain was not significantly different from the asymptomatic population.
Williams and colleagues41 suggested that thoracic disc herniation may be common enough to be considered a normal variant on MRI. More recently, Niemelainen and colleagues61 reported that degenerative thoracic MRI changes were less common than previously reported. In a cross-sectional study of men 35 to 70 years old from the Finnish Twin Cohort study, only 9.2% of subjects had posterior disc bulging. Anterior disc bulging was much more common, found in 45.2%. The presence of anterior disc bulging was positively correlated with age (r = 0.15 to 0.23, P < .005). Moderate to severe disc height narrowing ranged from 5.4% to 9.5% by level in the thoracic spine.
Etiology
Most authors favor degenerative processes as the major cause of thoracic disc herniation.3,20,57 This theory is supported by the higher incidence of herniation in the thoracolumbar spine, where greater degenerative changes occur.34,40,62 In a review of MRI findings and their relationship to thoracic and lumbar disc degeneration in a cohort of 232 subjects, Videman and colleagues40 noted that moderate and severe osteophytes were most common at the T11-12 level (20.7% of subjects); upper endplate irregularities were most common at levels T8-12, typically in the middle of the endplates in the thoracolumbar spine compared with more peripheral endplate changes in the lumbar spine. These results were later supported by Niemelainen and colleagues,61 who reported moderate to severe disc height narrowing in 21.4% of subjects.
The role of trauma as a cause of herniated thoracic discs is controversial. A history of trauma can be elicited in 14% to 63% of patients.35,45 The mean prevalence in 10 random series was 34%. In some patients, the causal relationship is undeniable; in others, trauma may have been an aggravating factor or purely coincidental. The degree of reported trauma responsible for herniation ranges from minor twisting strains and chiropractic manipulation to major falls or motor vehicle accidents.63
Several authors35,54,64 have suggested an association between Scheuermann disease and herniated thoracic discs. The primary pathogenic process of the disease or secondary disc degeneration may be the factors promoting herniation. Wood and colleagues42 noted that endplate changes consistent with Scheuermann disease were more prevalent in their symptomatic patient group than in the asymptomatic population.
Pathogenesis
The pathogenesis of neurologic compromise secondary to herniated thoracic discs is believed to be a combination of direct neural compression and vascular insufficiency.2,3,6,12,26 Middleton and Teacher2 suggested this in a case reported in 1911. Severe back pain developed while this patient was lifting a heavy object. Approximately 20 hours later, he felt a sudden severe pain shoot from his chest to his feet and he became almost completely paraplegic. The patient died 16 days later of urosepsis. The autopsy revealed a herniated thoracic disc opposite a section of cord that was compressed, degenerated, and hemorrhagic. A thrombosed vessel was found in the section of cord showing the most hemorrhage.
Several anatomic features make the thoracic cord vulnerable to manipulation and trauma.26 The thoracic spinal canal is small, and most of its available space is occupied by the cord. The blood supply to the cord is tenuous in this region, especially in the “critical zone” of T4-9.65 In addition, thoracic disc protrusions are more common centrally than laterally, are often calcified, and may adhere to or penetrate the dura.*
The theory of direct compression causing neural compromise is supported by the report by Logue12 of a patient who died after a 14-month course of progressive paraplegia. The autopsy showed extreme distortion of the cord, but the anterior spinal artery and vein were patent and showed no evidence of damage. Kahn68 suggested that, in addition to direct anterior compression by the herniated disc, the dentate ligaments may resist posterior displacement of the cord, leading to traction and distortion of neural structures.
Vascular insufficiency has been the explanation for unusual cases, such as cases with transitory paresis and instances in which the segmental level of involvement was higher than expected from the location of the herniated disc.3,6 Significant neural deficits may be caused by herniations that appear too small to cause significant compression. This theory also helps explain patients who show no improvement after complete decompression and patients who had an abrupt onset of paraplegia in the presence of a chronic calcified disc. The theory is supported by patients in whom the disc herniation has been shown to cause anterior spinal artery thrombosis.12
Doppman and Girton69 performed an angiographic study on the effect of laminectomy in the presence of acute anterior epidural masses. They found that when decompression restored normal arteriovenous hemodynamics, the animals were neurologically intact despite significant cord distortion. When either the artery or the vein remained obstructed, however, the animals remained paraplegic.
Clinical Presentation
In symptomatic cases, the condition is dynamic and can progress.9 Tovi and Strang16 outlined the usual chronologic progression, which begins with thoracic pain followed by sensory disturbances, weakness, and finally bowel and bladder dysfunction. Arce and Dohrmann20 confirmed this pattern in their review of the literature: Of 179 patients who described their initial symptoms, 57% described pain, 24% described sensory disturbance, 17% described motor weakness, and 2% described bladder dysfunction (Table 44–1). By the time of presentation, 90% of the patients had signs and symptoms of cord compression, 61% had motor and sensory complaints, and 30% had bowel or bladder dysfunction (Table 44–2). The duration of symptoms before presentation ranged from hours to 16 years in one series.3 In a report of 55 patients initially treated conservatively, Brown and colleagues70 reported anterior bandlike chest pain as the most common early symptom in 67% of patients; lower extremity complaints were present in 20% of patients and ranged from paresthesia (4%) to frank muscle weakness (16%). Additional symptoms included intrascapular pain (8%) and epigastric pain (4%).
TABLE 44–1 Initial Symptoms of Protruded Thoracic Disc
| Symptom | No. Patients (%) |
|---|---|
| Pain | 102 (57) |
| Sensory | 42 (24) |
| Motor | 31 (17) |
| Bladder | 4 (2) |
From Arce CA, Dohrmann GJ: Herniated thoracic disks. Neurol Clin 3:383-392, 1985.
TABLE 44–2 Presenting Features of Thoracic Disc Herniation
| Feature | No. Patients (%) |
|---|---|
| Motor and sensory signs and symptoms | 131 (61) |
| Brown-Séquard syndrome | 18 (9) |
| Sensory signs and symptoms only | 33 (15) |
| Motor signs and symptoms only | 13 (6) |
| Radicular pain only | 20 (9) |
| Bladder or sphincter features | 65 (30) |
From Arce CA, Dohrmann GJ: Herniated thoracic disks. Neurol Clin 3:383-392, 1985.
Thoracic pain can be midline, unilateral, or bilateral, depending on the location of the herniation. In some cases, there may be no pain. Coughing and sneezing may aggravate pain, as with herniated discs in the cervical and lumbar regions. With herniation of the T1 disc, the pain may be in the neck and upper extremity and simulate a cervical disc problem, causing upper extremity numbness, intrinsic muscle weakness, and Horner syndrome.5,26,71
When the herniation is in the mid-thoracic spine, radiation of pain into the chest or abdomen can simulate cardiac or abdominal disease, clouding an already complex clinical picture. In the four cases reported by Epstein,7 one patient underwent an unnecessary thoracotomy for excision of a pericardial cyst, hysterectomy and salpingo-oophorectomy were performed in another patient, and a third patient almost underwent an abdominal exploration for endometriosis before the true cause of her symptoms was identified. Pain from a lower thoracic disc herniation may radiate to the groin or flank and simulate ureteral calculi or renal disease.62,72,73 Abdominal wall paresis and abdominal hernia have also been presenting signs for thoracic disc herniations.74,75 Herniated discs at the lowest thoracic levels can impinge on the cauda equina and on the distal spinal cord causing lower extremity pain or weakness and mimic a herniated lumbar disc.76,77 On physical examination, flexion of the neck may induce back or root pain with lesions below the mid-thoracic level.25 A thorough neurologic examination is mandatory, and the examiner should pay close attention to long tract signs and other evidence of myelopathy.
Some investigators believe that the occurrence of pronounced sensory changes with relatively minor motor deficits is highly suggestive of a herniated thoracic disc.25,78 Sensory disturbances, motor weakness, sphincter dysfunction, and gait abnormalities should direct the examiner’s attention to the nervous system as the source of the problem.
Level and Classification of Herniation
Three fourths of cases occur between T8 and L1; the peak is at T11-12, where 26% to 50% of herniations occur (Fig. 44–2).20,40 Herniations are uncommon in the upper thoracic spine.20,26,71 Haley and Perry57 found a similar distribution in their cadaveric study of 99 spines and theorized that the increased incidence in the thoracolumbar area is due to the greater degree of motion in this region. The reason that the incidence at T11-12 is greater than that at T12-L1 (9%) may be the facet orientation. Malmivaara and colleagues79 believed that the coronally oriented facets in the upper thoracolumbar region have less torsional resistance than the sagittally oriented facets at T12-L1, so the T11-12 disc is exposed to greater stress and has a high likelihood of degeneration.
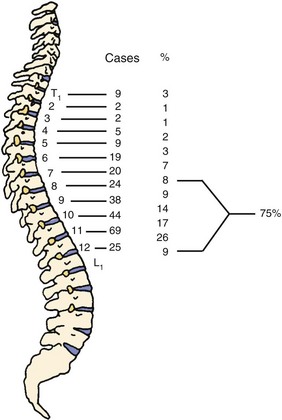
FIGURE 44–2 Levels of thoracic disc protrusion in 280 cases.
(From Arce CA, Dohrmann GJ: Herniated thoracic disks. Neurol Clin 3:383-392, 1985.)
Herniated thoracic discs can be classified by location or by symptoms. Most authors describe the location of the herniation as central, centrolateral, or lateral, and roughly 70% of the cases are either central or centrolateral.20,60 In a comparison of characteristics on CT myelography of asymptomatic and symptomatic herniated thoracic discs, Awwad and colleagues60 reported that 90% of herniations were central or parasagittal versus lateral in asymptomatic patients, whereas 80% were central or parasagittal in symptomatic patients. No identifiable radiographic features could reliably classify a herniated disc as symptomatic or asymptomatic. Abbott and Retter5 classified cases by symptoms and reported that lateral protrusions cause root compression and that patients have radicular pain and minimal or no signs of cord compression. Patients with central disc herniation in the upper and middle thoracic spine can have myelopathy. Protrusions at T11 and T12 compress the conus and cauda equina and may cause pain referred to the lower limbs and sphincter disturbance.
Few cases of intradural herniation of thoracic discs have been reported, suggesting that the incidence is low.3,8,16,26,80–84 Love and Schorn3 reported a series of 61 cases in which 7 (11%) showed disc erosion through the anterior dura. In a review of the literature, Epstein and colleagues81 noted that 5% of all intradural disc herniations were found in the thoracic spine. Similar to the cervical spine, the low incidence was attributed to the lack of significant dural adhesions of the thoracic dura to the posterior longitudinal ligament and anulus fibrosus. Patients with intradural thoracic disc herniations tended to present with a higher incidence of Brown-Séquard syndromes and paraplegia.44 In most cases, the presence of an intradural thoracic disc herniation is not identified preoperatively. CT myelography seems to have a higher sensitivity to detect this than MRI even with the addition of gadolinium.80
The exact incidence of multilevel herniations is unknown.5,14,35,85 Arseni and Nash6 reviewed the literature in 1960 and found multiple herniations in only 4 of 106 cases reported. A report by Bohlman and Zdeblick35 suggested, however, that the incidence may be much higher than previously recognized. Of their 19 patients, 3 (16%) had herniations at two levels. The sensitivity of MRI may be partially responsible for this increased frequency.37,39 Ross and colleagues39 reported that 3 of 13 patients (23%) whose herniation was diagnosed by MRI had multilevel involvement; Wood and colleagues42 reported multiple disc herniations in 39% of asymptomatic volunteers that were diagnosed by MRI. These rates are similar to the findings in the autopsy study by Haley and Perry,57 in which two of seven patients had more than one protruded disc.
Van Landingham64 suggested an association between Scheuermann disease and multilevel herniation. Wood and colleagues42 noted that endplate changes consistent with Scheuermann disease were more prevalent in the group with thoracic pain and disc herniation than in the asymptomatic population. Conversely, Lesoin and colleagues54 reported six cases of single-level herniations only in patients with Scheuermann disease, suggesting a lack of significant association with multiple herniations.
Natural History
There are few long-term reports of untreated adults with herniated thoracic discs. In 1992, Brown and colleagues70 reported a 2-year follow-up on 55 patients found to have thoracic disc herniation on MRI and concurrent pain; 11 (20%) initially had lower extremity complaints. Initial treatment in 54 patients included bed rest; nonsteroidal anti-inflammatory drugs; and controlled physical therapy involving hyperextension strengthening, postural training, and body mechanics education. Ultimately, 15 patients (27%) underwent operation. Of the remaining 40 patients treated nonoperatively, 31 (78%) returned to their prior level of activity. Nine of the 11 patients presenting with lower extremity complaints of pain or weakness underwent operation; 55% of herniated discs in the operative group were at or below T9. In contrast, 48% of the discs in the nonoperative group were at T6-9.
In patients with lower extremity complaints, the natural history of the disorder is typically one of progression, and nearly all patients eventually undergo operation for progressive neurologic deficit or unremitting pain.3,11 The most characteristic chronologic progression of symptoms is pain followed by sensory disturbance, weakness, and bowel and bladder dysfunction.16 The course can be extremely variable, however, and it is unknown whether neurologic signs or symptoms ever would have developed in patients operated on for pain alone. Some patients might have improved spontaneously if not subjected to surgical treatment. Haro and colleagues86 reported on two patients with acute onset of symptomatic thoracic disc herniation with signs of myelopathy that resolved without surgery. Both patients had lower extremity signs of myelopathy, but neither developed bladder dysfunction or progressive motor weakness. Treatment with steroids and prostaglandin E1 led to resolution of symptoms and resorption of thoracic disc herniation on follow-up MRI scans.
Arseni and Nash6 described two general patterns for the time course of symptoms. The first, which occurs in younger patients with a history of trauma, is backache that can be followed by a rapidly evolving myelopathy. In the second pattern, which typically occurs in patients past middle age who have degenerative disc disease without any significant trauma, signs and symptoms of cord compression develop slowly and progressively. Tovi and Strang16 found that when the first symptom to develop was unilateral, the course tended to be one of slow progression with periods of stabilization and occasional slight remission. Rapid, irreversible progression generally was noted in cases with a bilateral onset.
Calcification of the disc in children is considered to be a painful but self-limited process, with eventual resolution of the pain and resorption of the calcified deposit. It generally occurs in the cervical spine. About half of cases are preceded by a history of trauma (30%) or upper respiratory tract infection.87,88 The natural history of herniated calcified thoracic discs in children was reviewed by Nicolau and colleagues.89 The course was similar to cases without herniation; the patients improved spontaneously, and the calcified fragment resorbed. The progression is not always benign, however. Two cases in children have been reported in which myelopathy developed from cord compression and required operation.13,67
Disc calcification in adults differs from that in children. The thoracolumbar spine is the most frequent site of calcification, and the condition is generally asymptomatic unless herniation of the disc occurs.87 The deposits may accelerate degeneration by interfering in the biomechanics and nutrition of the disc.87,90 Disc calcification is found on routine radiographs in 4% to 6% of patients without disc herniation compared with up to 70% of patients with disc prolapse.12,87 The natural history of disc herniation in adults has not been conclusively shown to be altered by disc calcification.
Differential Diagnosis
Love and Schorn3 reported that before myelography the correct diagnosis was made in 13 of 61 patients and was considered in the differential diagnosis in only 7 others; even after myelography, the correct diagnosis was made preoperatively in only 56% of patients. With greater awareness of the diagnosis and improved imaging techniques now available, the correct diagnosis should be made before operation in almost all cases.
The differential diagnosis of back pain includes spinal tumors and infections, ankylosing spondylitis, fractures, intercostal neuralgia, herpes zoster, and cervical and lumbar herniated discs. Diseases of the thoracic and abdominal viscera may have a similar presentation. Neurosis is another possibility. The differential diagnosis of myelopathy includes demyelinating and degenerative processes of the central nervous system, such as multiple sclerosis and amyotrophic lateral sclerosis.91,92 Intraspinal tumors, brain tumors, and cerebrovascular accidents also should be considered.20,63
In patients who have a neurologic deficit and radiographic evidence of Scheuermann disease, the differential diagnosis includes an extradural cyst or compression from an angular kyphosis.54,93 In the series by Lesoin and colleagues,54 the mean age of the patients who had a herniated thoracic disc in association with Scheuermann disease was 44 years, similar to the population without Scheuermann disease. This is in contrast to a mean age of 17 years in three patients in whom neurologic compromise developed secondary to bony cord compression at the apex of the kyphosis.93
Diagnostic Evaluation
Spine Radiographs
Plain radiographs of the spine generally are diagnostic only if they show disc calcification. The calcified disc is not always the one that is herniated, but the association at least suggests the diagnosis.3,94 A calcified disc in the canal is pathognomonic of disc herniation.12,27,28,94 Baker and colleagues94 identified two radiographic patterns of calcification (Fig. 44–3). One consisted of extensive calcification posteriorly in the interspace and bulging into the canal. The other pattern, which is subtle and often overlooked initially, is a small nidus just posterior to the narrowed interspace. Studies35,59 of adult lumbar discs have shown that the deposits may be calcium pyrophosphate dihydrate or calcium hydroxyapatite. The clinical significance of the different radiographic patterns or chemical compositions has not been determined.
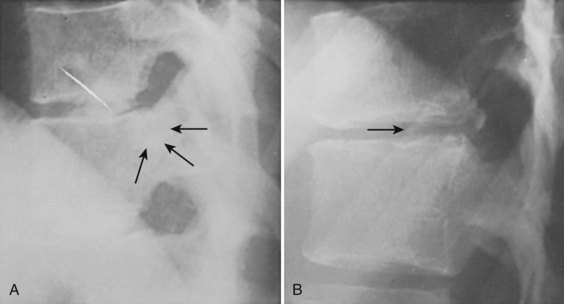
FIGURE 44–3 Plain radiographs can be used to diagnose herniated discs only when calcification is seen within spinal canal. A, Large calcified disc within canal (arrows) is nearly obscured by overlying ribs (see Figs. 44-7 and 44-8 for CT and MRI scans from same patient). B, Tiny nidus of calcium is visible in canal posterior to narrowed 11th interspace (arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








