1
Thermal, Chemical, and
Electrical Burns
Ziv M. Peled and Jonathan S. Schreiber
History and Clinical Presentation
A 77-year-old man undergoing chemotherapy for lung cancer was seen in consultation by the plastic surgery service after suffering a burn injury to the dorsum of his right hand. A previous intravenous (IV) site had infiltrated in the man’s right hand and this was removed. A different site was begun in another location for administration of mitomycin C. The chemotherapeutic agent extravasated at the site of the first IV line in the right hand, resulting in a chemical burn.
PEARLS
- There are multiple ways to treat burns of the hand, depending on the degree of the burn and associated injuries. Several principles should always be kept in mind and are critical to a successful outcome. These are early debridement and edema/infection control, early wound coverage, and early mobilization. Adherence to these simple principles will likely prevent or minimize common postburn complications such as flexion contractures and boutonniere deformities.
- When completing the dissection of a distally based flap, the surgeon should examine the flap for evidence of venous congestion. If venous congestion is noted, a venous anastomosis should be performed to achieve adequate flap drainage. This technique, although infrequently necessary, can improve flap viability.
PITFALLS
- Evaluation of a burn wound is challenging because the thickness of burn is often difficult to determine initially.
Physical Examination
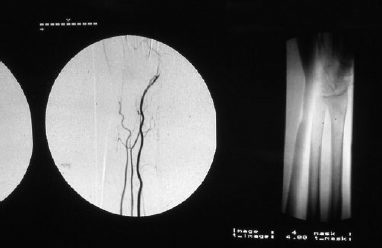
On initial examination the involved skin and subcutaneous tissue were cellulitic with a small area of necrosis. Initial debridement was performed in the office and revealed that the wound extended to the level of the deep subcutaneous tissue. The extensor tendons were noted to be covered by soft tissue and paratenon. Normal saline dressings were used to promote granulation tissue for possible future split-thickness skin grafting. Despite meticulous wound care, the overlying soft tissue became necrotic and required further debridement with resultant broad exposure of the extensor communis tendons. Minimal granulation tissue formation was noted. The patient was subsequently admitted to the local university hospital for workup and definitive treatment.
Differential Diagnosis
Thermal burns
Chemical burns
Electrical burns
Diagnosis
Chemical Burn
The patient had a chemical burn caused by extravasation of mitomycin C. Tissue necrosis and sloughing is known to occur with extravasation of several types of chemotherapeutic agents and is well described with the use of mitomycin C. This tissue reaction has been known to occur at sites distant from the injection site.
Alternative Methods of Management
The primary goal in the treatment of all hand injuries is to restore optimal function. There are multiple ways to treat burns of the hand, depending on the thickness and extent of the burn and associated injuries. Several principles should always be kept in mind. Early debridement, edema/infection control, early wound coverage, and early mobilization are critical to a successful outcome. Adherence to these simple principles will likely prevent or minimize the most difficult postburn complications such as flexion contractures and boutonniere deformities.
A variety of flaps have been described for coverage of hand wounds after burn injury (Table 1–1). Each technique has its unique advantages and disadvantages. Local flaps such as the homodigital flap have been successfully used to treat defects of the hand. The benefits of this technique include a one-stage procedure and the use of skin with similar thickness, appearance, and elasticity. The limitation of this flap is the limited area of skin for coverage and the ability to cover only very distal hand injuries. A more traditional technique is the use of a two-stage groin flap. This flap has the advantage of ample suitable skin for coverage, but the resultant immobilization of the involved hand makes this option less appealing in most patients. Recently, neurocutaneous ulnar nerve/artery flaps have been described. Aside from similar skin characteristics, these flaps have the reported advantage of preserved cutaneous sensation in the flap. Unfortunately, these flaps require a more involved dissection and there is limited experience with them. Another option is the distally based radial or ulnar forearm flap. These flaps can cover large defects, provide skin with characteristics similar to the recipient site, do not require staged procedures or immobilization, and do not require extensive dissection or, in many cases, vascular anastomoses. Another option is a free flap. Radial forearm free flaps from the opposite arm and temporoparietal free flaps with split-thickness skin graft (STSG) have both been described. The need for a vascular anastomosis and the risk of flaploss are the major disadvantages. The decision or method of reconstruction can be thought of as a “reconstructive ladder.” Each wound needs to be evaluated carefully and the decision for coverage is determined by many factors. The extent and site of the wound as well as associated injuries help to determine the method of coverage.
| Type | Example |
| Local flap | Homodigital flap, advancement flap |
| Distant flap | Groin flap |
| Distally based fasciocutaneous flaps | Radial or ulnar forearm flap |
| Neurocutaneous flaps | Ulnar artery/nerve flap |