11
Mycobacterial Tenosynovitis
John C. P. Floyd and Waldo E. Floyd III
History and Clinical Presentation
A 66-year-old man employed as a machinist was referred for further evaluation of limited range of motion and swelling in his left hand and distal forearm, which had been progressive over the past 8 months. The patient had been impaled over the volar aspect of the volar forearm by a saltwater catfish fin 18 months previously. The patient’s surgical and medical history was otherwise negative.
Physical Examination
The patient had limited range of motion in the thumb and small finger and a 4 × 5 cm cystic mass over the volar aspect of the wrist and distal forearm (Fig. 11–1). Over the volar aspect of the thumb, there was marked swelling about the flexor tendon sheath. To a lesser degree, the small finger was also swollen over the flexor sheath and rested in slight flexion at the interphalangeal joints. There was limitation of composite digital flexion, but all flexor tendons were intact. Neurovascular examination of the hand was normal. No evidence of axillary or epitrochlear node involvement was present.
Diagnostic Studies
Anteroposterior and lateral radiographs of the left hand were positive for soft tissue swelling. No evidence of osseous involvement was present. A magnetic resonance imaging scan demonstrated a 4 × 5 × 3 cm mass volar to the pronator quadratus without evidence of bone involvement (Fig. 11–2). The mass was homogeneous and had a signal intensity consistent with soft tissue.
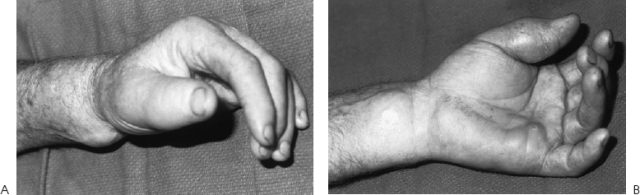
Figure 11–1. (A) Progressive hand and wrist swelling. (B) Eighteen months following a penetrating volar wrist injury by a saltwater catfish. (With permission from Floyd WE III, Foulkes GD. Tuberculous, mycotic, and granulomatous disease. In: Peimer CA, ed. Surgery of the Hand and Upper Extremity, 1st ed. New York: McGraw-Hill; 1996.)
PEARLS
- High index of suspicion
- Obtain a thorough history of possible exposure
- Surgical debridement is key to affecting a cure
- Obtain infectious disease consultation
PITFALLS
- For species-specific diagnosis, culture is necessary.
- Treatment should be modified to the specific species.
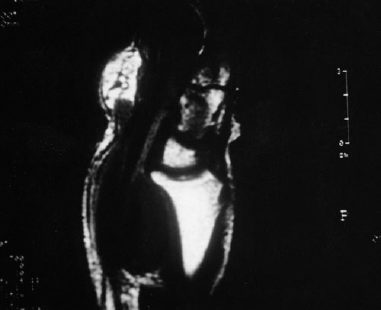
Figure 11–2. Magnetic resonance imaging scan demonstrating a solid soft tissue mass volar to the pronator quadratus. (With permission from Floyd WE III, Foulkes GD. Tuberculous, mycotic, and granulomatous disease. In: Peimer CA, ed. Surgery of the Hand and Upper Extremity, 1st ed. New York: McGraw-Hill; 1996.)
Differential Diagnosis
Neoplasm
Fungal infection
Mycobacterial infection
Bacterial infection
Diagnosis
Microbacterial Infection
The diagnosis was a horseshoe abscess of noncaseating granulomatous disease secondary to mycobacteria other than tuberculosis (MOTT). Cultures were positive for Mycobacterium avium-intracellulare complex.
A major cause of granulomatous infections is mycobacteria. Two of the earliest identified mycobacteria were Mycobacterium tuberculosis and Mycobacterium leprae. Tuberculosis remains the most common pathologic organism of this genus. Hansen’s disease or M. leprae has long been recognized as a separate species, but leprosy is far less common in most parts of the United States than some of the more newly recognized species. “Atypical mycobacteria” has traditionally meant a mycobacterium that is neither tuberculosis nor leprosy. An increased understanding of all nontuberculosis infections has led to the introduction of the term mycobacteria other than tuberculosis (MOTT).
Timpe and Runyon first showed MOTT to be pathogenic in humans in 1954. The Runyon classification system has been used to delineate species on the basis of pigment production or growth rate in culture. Runyon groups I, III, and IV have been identified as pathogenic in humans.
Mycobacteria may be identified immediately with acid-fast stain, but most often, as in this case, MOTT is not seen. Current microbiologic methods may take 8 to 10 weeks to identify the slow-growing MOTT. In vitro sensitivities may not be available for at least another week.
Because the hand is the major manipulator of the environment, the hand is more likely to be inoculated with saprophytic bacteria. Infection occurs by either cutaneous or deep (noncutaneous) pathways. Cutaneous infections are far more common. Abrasions on the extremities involving an aquatic environment (swimming pools, aquaria, fishing) are the prototypical cases. These infections can spread proximally with multiple abscesses resembling sporotrichosis. Deep infections in the adult patient present as a spectrum of disease progressing from tenosynovitis to septic arthritis. All species of MOTT can be acquired from prior trauma except Mycobacterium kansasii, which usually shows no clear mode of inoculation. Mycobacterium marinum is the most common cause of MOTT infections of the upper extremity followed in frequency by M. kansasii. Symptoms appear slowly and are only occasionally characterized by typical inflammatory criteria. A thorough remote and recent history is essential in raising suspicion of a MOTT infection, because MOTT infections are indolent and may present long after inoculation.
Surgical Management
A zigzag incision was made over the volar aspect of the wrist. The median nerve was identified and carefully protected. A large mass was present about the flexor tendons. The mass was opened and contained multiple rice bodies (Fig. 11–3). A frozen section biopsy demonstrated the presence of granulomatous disease.










