Fig. 4.1
Different landmarks used to determine tibial rotation (ATA anatomical tibial angle, STA sagittal tubercle axis, PCA posterior condylar axis)
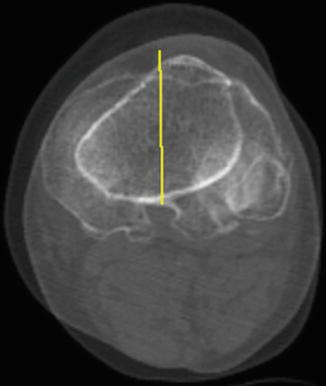
Fig. 4.2
Akagi’s line: a line connecting the middle of the posterior cruciate ligament and the medial edge of the patellar tendon attachment (fusion of 2 CT scan slides)
It has also been reported that alignment of the tibial TKR component along the femoral epicondylar axis more reliably results in proper rotational positioning of the tibial component with respect to the patellar ligament [9, 20].
In the absence of precise and easily identifiable tibial anatomical landmarks, the self-adjustment method uses the posterior border of the femoral condyles. This method aligns the tibial baseplate performing several cycles of knee flexion/extension movements (Fig. 4.3). Such method, which has been criticized by Nagamine et al. [21] and Ikeuchi et al. [22], should be used only in case of reliable rotational alignment of the femoral component. As a “dependent” method, it relies on the femoral and tibial bone cuts performed in the frontal plane. When considering the surgical transepicondylar axis of Berger et al. [23] as rotational axis of the knee and femoral implant rotational alignment to be parallel, this axis can be taken as a reliable reference for rotational alignment of the tibial component.
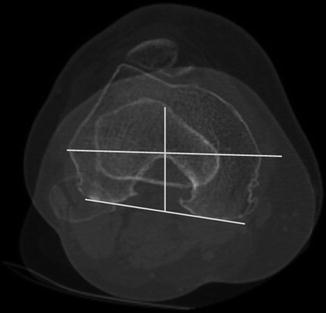
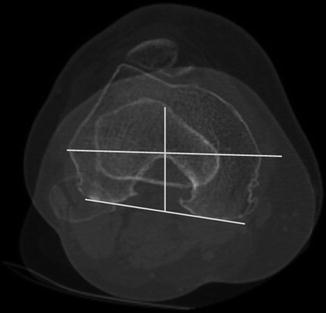
Fig. 4.3
Preoperative CT scan: tibial axis related to the femoral transepicondylar axis and the posterior femoral condyles
The self-adjustment method can be reliable and reproducible since it provides an accurate femur-tibia parallelism with the posterior bicondylar axis of the femoral prosthesis [24]. However, this is only true when the femoral TKR is well positioned.
Important landmarks for tibial component positioning are between the medial and two lateral thirds of the anterior tibial tubercle, medial border of patellar tendon, right angle to the anteroposterior axis drawn between the posterior cruciate ligament insertion and medial border of patellar tendon (Akagi’s method), relative to the anterior tibial marginal line (Page’s method), femoral epicondylar axis, self-adjustment method, and medial-lateral axis of the resected tibial surface.
4.3 Tibial Component Placement in Varus and Valgus Knees
The rotation of the tibia has a high interindividual variability [9, 20, 24]. Berhouet et al. did a prospective nonrandomized study between March 2008 and December 2009 [24]. A CT scan was performed in 95 knees (87 patients) three months after primary TKR due to osteoarthritis of the knee. Ninety-four knees were included in this study. Two subgroups were made: a genu varum subgroup, which was operated using a medial parapatellar approach, and a genu valgum subgroup, which was operated using a lateral parapatellar approach.
Knowing the influence of the surgical approach on rotational alignment of the tibial TKR [25], and in order to simplify the study groups, all cases of genu varum operated on through the lateral approach (e.g., patellar subluxation or hardware removal) and all cases of genu valgum operated on through the medial approach were excluded from this study. We also excluded all cases of revision surgery of unicondylar or TKR. The NexGen LPS Flex (Zimmer) fixed-bearing and symmetrical knee prosthesis was implanted. The following CT scan measurements were done (Fig. 4.4):
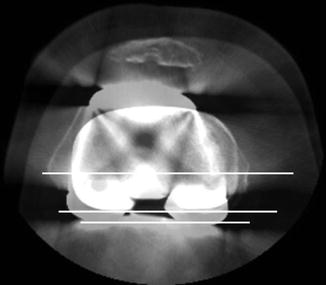
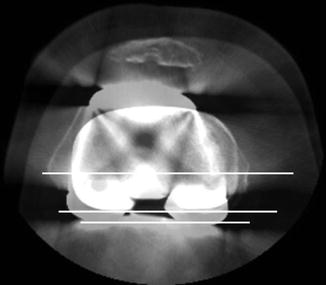
Fig. 4.4
Postoperative CT scan: method of measurement of the prosthetic posterior condylar angle (PCA TKR) between the anatomic transepicondylar axis (TEA) and the posterior bicondylar axis of the femoral prosthesis (PBCf TKR), the angle between the anatomic transepicondylar axis (TEA) and the posterior marginal axis of the tibial prosthesis (PMAt TKR), the angle between the posterior bicondylar axis of the femoral prosthesis (PBCf TKR) and the posterior marginal axis of the tibial prosthesis (PMAt TKR)
The prosthetic posterior condylar angle (PCA TKR), that is, the angle between the anatomic transepicondylar axis (TEA) and the posterior bicondylar axis of the femoral component (PBCf TKR).
The angle between the TEA and the posterior marginal axis of the tibial prosthesis (PMAt TKR). It corresponded to the rotation given to the tibial component with respect to the native femur.
The angle between the posterior marginal axis of the tibial prosthesis (PMAt TKR) and the posterior marginal axis of the tibial bone (native PMAt), obtained by superimposing the CT view passing through the tibial baseplate and the tibial CT view passing just below the metallic tibial baseplate. The objective was to evaluate the tibial component positioning in the transverse plane with respect to the native tibia.
The angle between the posterior bicondylar axis of the femoral prosthesis (PBCf TKR) and the posterior marginal axis of the tibial prosthesis (PMAt TKR). This angle was obtained by superimposing the two views passing through the posterior bicondylar axis on one hand and through the tibial baseplate on the other hand.
For all measurements, the intra-observer variability was not significantly different (variation coefficient between the two series less than 6 %).
Results according to HKA axis are summarized in Table 4.1.
Table 4.1
Influence of the surgical approach on rotational alignment of the tibial
n | Mean HKA angle | Mean distal epiphyseal femoral torsion (PBCf) | Prosthetic posterior bicondylar axis (PBCf TKR): target = 3° of external rotation | Tibial baseplate placement (relative to femoral component) | Tibial baseplate placement (relative to native tibia) | |
|---|---|---|---|---|---|---|
Varus knees | 50 | 172.2° (162.5–179) | 4.9° (2–7) | 3.14° ± 1.91 (range 0–17.5°) | 0.7° ± 4.45 of external rotation (range 9.5–9.2) | 6.1° ± 5.85 of external rotation (range 4.6–22.5°) |
Valgus knees | 45 | 182.3° (181–198) | 6.1° (2–10). | 4.72° ± 2.7 (range 0–11°) | 0.9° ± 4.53 of external rotation (range 10.8–9.5°) | 12.52° ± 8.6 of external rotation (range 10–28.9°) |
Using the self-adjustment technique, with the posterior condylar angles as a rotational reference for the tibial baseplate, both varus and valgus knees are well corrected (Figs. 4.4 and 4.5).
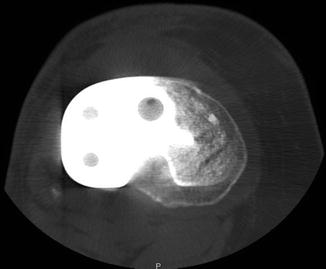
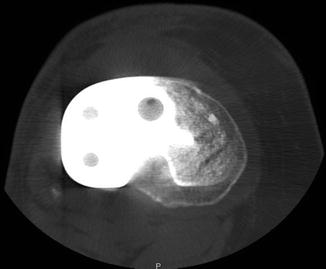
Fig. 4.5
Same patient. By the use of a symmetrical tibial component, which is properly externally rotated, there is a lack of coverage of the posterior part of the medial tibial plateau
4.4 Mobile-Bearing Components: A Solution for Tibial Malrotation?
In theory, a mobile-bearing tibial component improves the rotational placement of the tibia under the femur, when compared to a fixed-bearing component (FB). More precisely, it is said to be more forgiving in terms of rotational malalignment.
Comparative studies of the two designs (fixed-versus mobile-bearing TKR) in the same patient failed to demonstrate a difference in range of motion, knee preference, knee scores, survivorship, and patellofemoral complications [26–29]. Several authors have demonstrated that the tibial insert of a mobile-bearing TKR stops moving when flexed more than 90°. It then functions similarly as a fixed-bearing TKR design [30]. In flexion, kinematic studies have found an identical paradoxical anterior tibial displacement of both designs [31]. Fluoroscopic studies have shown that both designs have kinematic profiles similar to a native knee [32]. Range of motion is often used as a measure of kinematics. Fixed- and mobile-bearing TKR have shown a tendency toward a greater arc of flexion. However, this finding has not been reproduced or evidenced by RCTs or meta-analyses [33–36]. In summary, the use of a mobile-bearing component does not avoid malpositioning and complications due to malrotation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








