Fig. 52.1
Joint line elevation after revision TKR for infected primary TKR. Joint line elevation occurred as a consequence of attempting to match the extension space with the intraoperatively noted loose flexion space. The surgeon tried to achieve this by proximalising the femoral component, as is obvious from the position of the joint line in reference to the patella, fibular styloid, and epicondyles
Changes in femoropatellar contact area and kinematics after joint line elevation of 4–8 mm have been reported in biomechanical studies, which may partially explain the symptoms [19].
Joint elevation automatically causes patella baja. However, patella baja also occurs when there is a shortening of the patella ligament such as in arthrofibrosis (Fig. 52.2a, b). The Insall-Salvati Index helps to distinguish between the two etiologies of patellofemoral malposition.
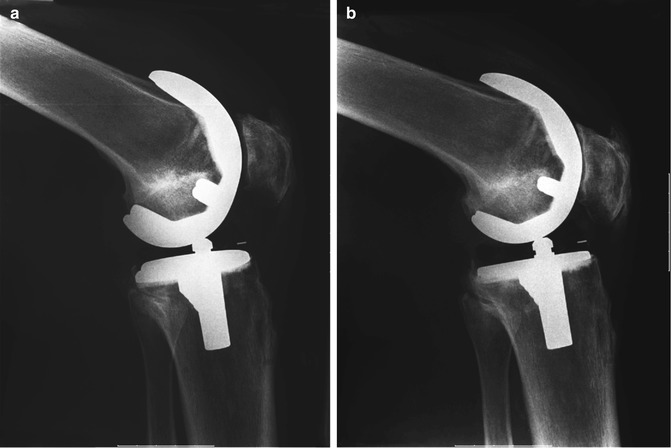
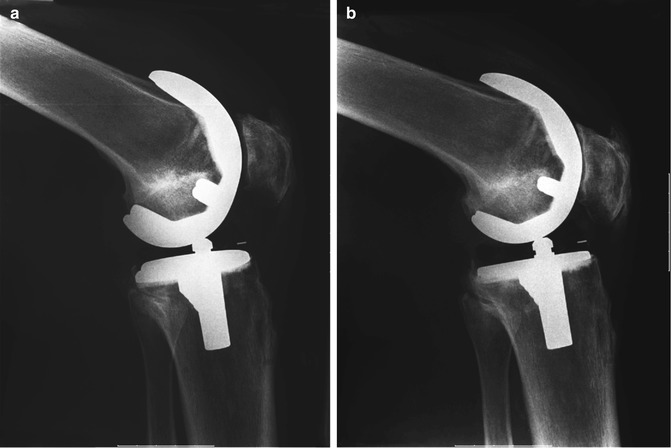
Fig. 52.2
Patella baja caused by shortening of the patella ligament due to arthrofibrosis. Showing a case one (a) and five (b) years after surgery
52.1 Cause for Joint Line Elevation in Revision TKR
In revision TKR, there is a tendency for the surgeon to proximalise the joint line [1–3]. There have been several reasons identified (Table 52.1).
Table 52.1
Common causes of joint line elevation in revision TKR
Underestimation of distal femoral bone loss |
Increasing the extension space to accommodate for an increased flexion gap due to |
Undersizing of femoral component to accommodate posterior bone loss |
Capsuloligamentous damage to the mediolateral soft tissues effective in flexion |
Anteriorisation of the femoral component due to the use of straight stems |
Typical reasons for joint line elevation in revision TKR are distal femoral bone loss, undersizing of femoral component and generally larger flexion than extension space in revision surgery.
First of all, there is always inevitable distal femoral bone loss, even after gentle removal of the primary femoral component (Fig. 52.3). This will automatically cause proximalisation of the femoral component.
Fig. 52.3
Femoral and tibial component removal after cemented TKR. Significant bone of the medial and lateral condyle is still attached to the femoral component. It is essential to underline the femoral component with a thin sawblade or chisel in order to avoid any bone loss
Secondly, the surgeon has the tendency to undersize the femoral component in revision TKR. This is a consequence of the fact that, after extraction of the primary femoral component, the surgeon will also be faced with posterior bone loss and will have a tendency to choose a smaller femoral component size in order to obtain direct seating of the component against the remaining bone (Fig. 52.4). In order to achieve stability both in flexion and extension, the use of a thicker tibial insert will subsequently be needed, leading to elevation of the joint line.
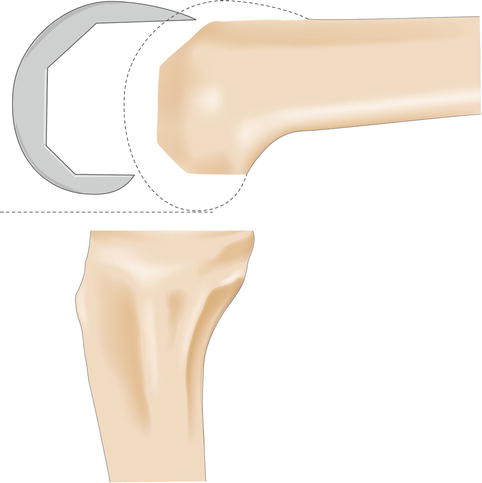
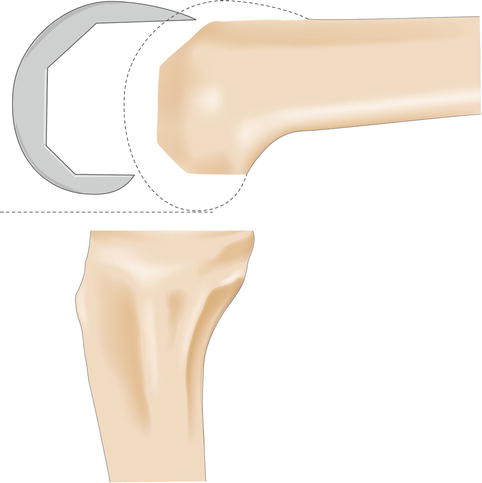
Fig. 52.4
After removal of the primary components, the surgeon has a natural tendency to undersize the femoral component in order to achieve direct bone contact. This leads to an increased flexion space, which could steer the surgeon toward proximalising the femur in order to balance the flexion and extension gaps. Consequently, joint line elevation will occur
The third reason is that in revision TKR, the surgeon will commonly be confronted with a relatively larger flexion space after component removal and joint debridement, compared to the extension space. This occurs because, in the revision situation, the capsulo-ligamentous structures that are effective in extension are usually much better preserved than those that control the knee in flexion. The surgeon may therefore decide to fill up the flexion space by using a thicker insert and compensatorily increase the extension space by proximalising the femoral component in order to obtain a balanced flexion and extension gap. This will result in an elevation of the joint line.
The use of a non-offset diaphyseal femoral fixation stem may further increase this tendency toward the creation of an excessive flexion gap, because non-offset stems tend to position the femoral component anteriorly (Fig. 52.5). Again, in such a circumstance, a stable and functional joint can only be obtained if the surgeon is prepared to use a thick polyethylene insert and accept an elevated joint line.
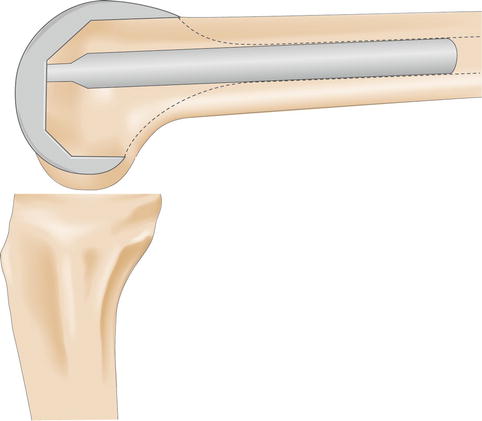
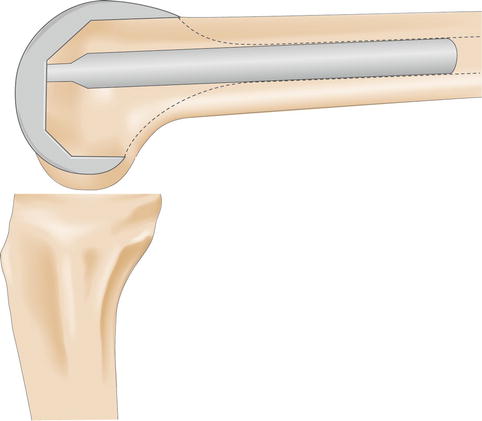
Fig. 52.5
A straight diaphyseal stem provokes anterior seating of the femoral component, and this again leads to an increased flexion space. Also, in this situation, the surgeon can choose to proximalise the femur to balance the flexion and extension gaps. This will again lead to joint line elevation
Finally, revision TKR always inevitably comes with some damage and stretching of the capsule-ligamentous soft tissue sleeve around the knee. The surgeon will therefore be confronted with the necessity to fill up the joint by lengthening the leg. This can be done by adding material to the proximal tibia, the distal femur, or both. The authors of this chapter believe that such build-up should be divided over both the femur and tibia in order to maintain as much as possible the isometric nature of the mediolateral soft tissues as well as the patellar height in reference to the tibiofemoral joint line. This means that joint line elevation will always occur to some extent, at least when measured from the tibia. Likewise, however, when measured from a femoral reference (e.g. the hip centre or adductor tubercle), the same situation can be considered joint line distalisation.
The last aspect is generally forgotten in the discussion of joint line elevation during revision TKR. It puts the issue in a somewhat different perspective and, in fact, demonstrates that some joint line elevation as commonly defined (i.e. from a tibial or distal reference) is unavoidable and probably even desirable after revision TKR.
52.2 Consequences of Joint Line Elevation
Today, it is not fully clear what the clinical and biomechanical consequences of joint line elevation are. Certainly there are some theoretical concerns. Optimal knee joint function obviously requires a delicate balance between the osseous anatomy and the surrounding soft tissues, which is dramatically distorted in case of joint line elevation [3, 11, 12, 14]. Impingement of the inferior pole of the patella against the tibial insert has been observed, as well as patella baja and impingement of the patellar tendon against the anterior surface of the tibial component, causing pain, structural tendon damage, and limited knee flexion [11, 15, 16].
Joint line elevation of 10 mm and 15 mm leads to patellofemoral contact force of 60 and 90 % body weight, respectively [10]. That may partially explain postoperative pain and limited knee function.
Biomechanical studies showed midflexion instability when the femoral component was shifted proximally and anteriorly of 5 mm [9]. In contrast, distalisation and a more posterior position of the femoral component caused midflexion tightness. The isolated elevation of the joint line does not seem to increase midflexion laxity as shown in a computer model [13].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








