Fig. 16.1
Lateral radiograph demonstrating flexion instability with a CR TKR
1.
The most common cause of flexion instability in CR TKR is due to an excessive flexion gap by either undersizing the femoral component or an excessive posterior tibial slope. Others include an iatrogenic PCL injury, or acquired PCL insufficiency due to aggressive postoperative rehabilitation.
The surgical technique greatly influences the stability of the knee. Recreation of posterior condylar offset (PCO) is an important aspect of flexion gap balancing [8]. Over-resection of posterior femoral condyles with undersizing the femoral component in anteroposterior dimension can result in laxity in flexion. This is easily diagnosed by comparing the PCO in preoperative and postoperative lateral radiographs. The reduced PCO also produces a relative PCL laxity and paradoxical anterior femoral roll back [8]. This can easily be appreciated in lateral projection radiographs at 30° and 90°. This situation is corrected with upsizing the femoral component and use of posterior augments.
Recreation of posterior condylar offset (PCO) is an important aspect of flexion gap balancing.
Excessive tibial slope is also responsible for a flexion-extension gap mismatch (Fig. 16.2). The lax flexion space puts excessive forces on PCL, stretching and resulting in PCL insufficiency. This is usually treated by revision to a posterior-stabilised TKR and accurate flexion and extension gap matching.
Iatrogenic damage to PCL during a CR TKR is a known cause of flexion instability. This can occur during tibial preparation by overzealous tibial resection [2]. The PCL can also be damaged during aggressive physical therapy to achieve range of motion and flexion in a knee in which the flexion space is left tight and overstuffed. Some patients are able to recall an episode of feeling a snap during physical therapy and immediate improvement in motion. Lastly, PCL insufficiency can occur due to continuation of the disease process in inflammatory joint arthritis [2] or in long-lasting cases due to age-related attenuation [5]. The initial treatment is usually nonoperative with conversion to revision surgery in patients with persistent symptoms. Conversion to posterior-stabilised TKR with careful attention to flexion-extension gap balancing results in consistently good results [2].
PCL insufficiency can occur during tibial preparation or during aggressive physical therapy to achieve range of motion and flexion in a knee where the flexion space is left tight and overstuffed.
16.1.2 Flexion Instability in Posterior Stabilised (PS) TKR
Presence of a spine-cam mechanism in PS TKR, although prevents posterior translation of the tibia on the femur, certainly does not prevent flexion instability if enough attention was not drawn towards achieving equal flexion-extension gaps (Fig. 16.3). Patients with PS TKR can also have subtle flexion instability presenting with pain, especially while negotiating stairs, a sense of instability, recurrent joint effusions and periarticular tenderness [3]. The diagnosis of flexion instability requires a high level of suspicion and is based predominantly on clinical assessment. Diagnosis of flexion instability as cause of residual pain after PS TKR requires high index of suspicion. All patients with TKR should also be examined in 90° of flexion with an anterior to posterior translation force while the patient is dangling his legs at the side of the table. Occasionally, a visible sag is seen at the tibiofemoral articulation while doing this examination (Fig. 16.4). The diagnostic features of flexion instability are summarised in Table 16.1.



Fig. 16.3
Lateral radiograph demonstrating flexion instability with a PS TKR

Fig. 16.4
A visible sag at tibiofemoral articulation in flexion instability
Table 16.1
Diagnostic features of flexion instability
Symptoms |
Diffuse knee pain |
Recurrent effusions |
Difficulty negotiating the stairs and difficulty in getting up from sitting position |
Signs |
Excessive anteroposterior laxity in 90° flexion |
Condylar liftoff with varus and valgus stress at 90° flexion |
Stable in extension |
Knee effusion and multiple tender points around the tendon insertion points |
Radiographic findings |
Undersized femoral component |
Anterior placement of femoral component |
Loss of posterior condylar offset |
Excessive tibial slope |
Paradoxical anterior tibial translation in a PCL retaining implant in lateral projection comparing from 30° to 90° |
In suspicion of instability, all patients after TKR should be examined in 90° of flexion with an anterior to posterior translation force while the patient is dangling his legs at the side of the table.
Similar to CR TKR, certain aspects of surgical technique may predispose to development of flexion instability in PS TKR [9]. These include poor restoration of posterior condylar offset (PCO) resulting from over-resection of the posterior condyles due to either undersizing or anteriorizing the femoral component (Fig. 16.5), femoral component malrotation which could lead to asymmetric flexion gaps [10] and increase in posterior tibial slope (Fig. 16.2). Appropriate gap balancing by establishing stability of the flexion space without affecting extension is of paramount importance at revision surgery for flexion instability. Surgical options include the elevation of joint line with distal femoral resection and the use of a thicker tibial component or upsizing femoral component with the use of posterior augments to increase the PCO or complete revision to address all issues (Fig. 16.6a, b). Isolated tibial polyethylene insert exchange has been reported to be of limited utility in the management of flexion instability compared to complete revision [3]. It is our goal, as has been described before, to have a stable flexion gap with an anterior tibial translation of less than 5 mm. The polyethylene tibial post in a PS knee is not designed to withstand all the stresses experienced with instability. A broken polyethylene post with polyethylene debris-related synovitis can also be a cause for pain and flexion instability in PS TKR [11]. In this case, revision arthroplasty is required to balance the gaps and reduce the stresses on the tibial post. Occasionally, the flexion instability is manifested with a frank dislocation and severe pain. Most of these cases were reported in earlier published isolated case reports [12–14]. Most current conventional posterior-stabilised TKRs have increased the so-called jump-distance, and a frank dislocation is a rarity.

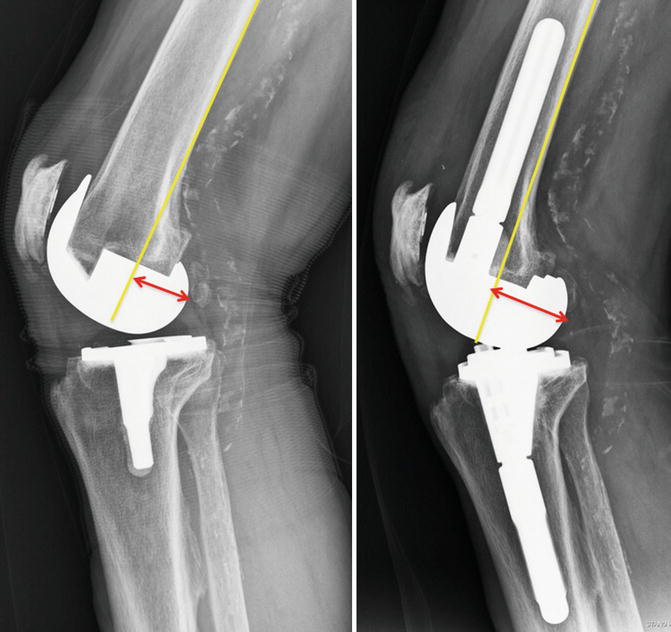

Fig. 16.5
Lateral radiograph demonstrating flexion instability with a PS TKR due to reduced posterior condylar offset
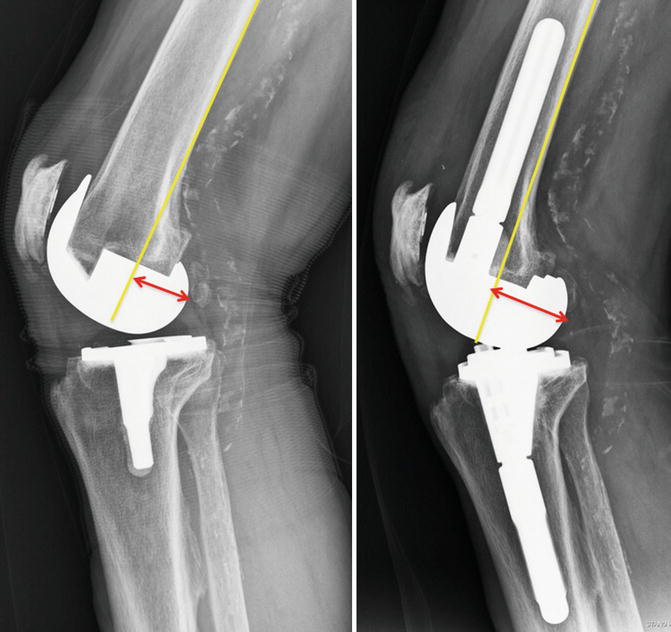
Fig. 16.6
(a) Poor restoration of posterior condylar offset in primary TKR. (b) Accurate restoration of posterior condylar offset with posterior augments in revision TKR restoring flexion gap
16.2 Extension Instability
Extension instability is the most common form of instability in TKR resulting in pain and swelling and patients complaining ‘not enough confidence in my knee after surgery’. Extension instability can be symmetric and asymmetric.
Extension instability is the most common form of instability in TKR resulting in pain and swelling and patients complaining ‘not enough confidence in my knee after surgery’.
16.2.1 Symmetric Extension Instability
Symmetric extension instability results from inadequate filling of extension space by thickness of the components. Excessive resection from the proximal tibia and or distal femur can result into this situation. When there is too much proximal tibial resection, it affects extension and flexion space equally, and the TKR is loose in both extension and flexion, creating global instability. Revising the tibial component with a thicker polyethylene insert during revision surgery may treat this instability. The long-term concern regarding poor tibial fixation when excess tibial bone is removed still exists [15]; however, we recommend not revising the tibial component entirely, if intraoperative assessment shows a well-fixed component.
Over-resection of the distal femur can also lead to extension instability, and this poses a more difficult problem to treat. The knee is loose in extension and stable in 90° of flexion. Treating this problem with a thicker polyethylene insert can result in excessive tightening of the flexion space and elevation of joint line, which in turn alters the patellar kinematics [15–18]. This does not solve the problem. A definitive solution in these situations is revising the femoral component and using distal femoral augments to avoid joint line elevation [15–17] and avoid tightening the flexion space.
Symmetric extension instability results from inadequate filling of extension space by thickness of the components. It could be the consequence of excessive resection from the proximal tibia and/or distal femur.
16.2.2 Asymmetric Extension Instability
While symmetric extension instability is due to over-resection of the bone, asymmetric extension instability is usually due to poor attention at the soft tissue balance. Deformities in coronal plane in the knee cause contracture of the ligaments on the concave side and overstretching and lengthening of the ligaments on the convex side. TKR is a soft tissue operation as much as it involves accurate bone cuts. Asymmetric instability can be noted on a standing anterior-posterior (AP) radiograph with either medial or lateral joint space opening.
Asymmetric instability is more common in the valgus knee where under-correction of the deformity is more common. Under-correction leaves the lateral collateral ligament (LCL) and the lateral joint capsule tight, and eventually the valgus deformity recurs, leaving the knee unstable in extension with medial instability [15–17]. Soft tissue release for the fixed valgus deformity was originally described by Insall et al. [19, 20] who describe sequential release of lateral structures starting with LCL and continuing on to the popliteus tendon and eventually lateral head of gastrocnemius. Insall et al. proposed that iliotibial band should not be released except in severe external rotation deformities. Because of potential overrelease of the lateral side as described by Mihalko and Krackow [21], along with reports of TKR dislocations with patients with extensive release, Insall modified his technique and popularised the ‘pie crust’ or multiple fenestration technique. Clarke et al. reported our experience with this technique [22], and midterm results showed no clinical failures, cases of postoperative instability and no cases of radiographic loosening. The technique involves completion of accurate distal femoral and proximal tibial bone cuts and with the knee distracted in extension. The tight lateral structures are then assessed and released using a multiple puncture technique. First, at the level of the tibial bone cut, a no. 15 surgical blade was used to make a transverse incision through the arcuate ligament (posterolateral capsule), lateral to the popliteus tendon, at the posterolateral corner of the knee. Next, multiple horizontal stab incisions were made through the iliotibial band (ITB) and lateral capsule until medial-lateral soft tissue balance was achieved. The popliteus tendon is protected at all times as this is an important structure to provide stability in flexion. The flexion and extension space is then assessed by spacer block, and gap balance is assessed. The pie crusting technique can be repeated until equal gaps are created. If flexion and extension gaps are equal but the extension gap is tight to accommodate a minimal thickness spacer of 10 mm, an additional distal femoral cut is made to address this problem. We recommend no greater than 5 mm penetration of the lateral structures during this technique to avoid damage to peroneal nerve [23].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









