The Role of Arthroscopy in Treating Developmental Dysplasia of the Hip
Jeffrey A. Krempec
John C. Clohisy
Introduction
Developmental dysplasia of the hip (DDH) with associated structural instability is a common cause of prearthritic and arthritic hip disease (1). The pathomorphology of DDH is quite variable and can involve both the acetabulum and the proximal femur. Patients frequently present with prearthritic hip symptoms related to structural instability and acetabular rim overload in adolescence or young adulthood (2). In DDH, intrinsically normal intra-articular soft tissue structures are exposed to loading forces that physically exceed their tolerance level, resulting in progressive damage to the hip joint. Structural instability and anterolateral migration of the femoral head leads to chronic shear stresses at the acetabular margin initially resulting in labral hypertrophy with subsequent tearing of the labrum off the acetabular rim and/or an acetabular rim fracture. The adjacent acetabular rim articular cartilage also undergoes degeneration (3).
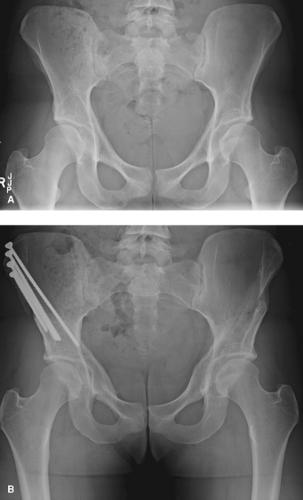
Treatment goals in the symptomatic patient are alleviation of pain, return to function, and prevention or delay of secondary osteoarthritic changes. Treatment for DDH is typically directed at correcting the underlying anatomical deformity, restoring femoral head coverage, and eliminating instability. Multiple pelvic osteotomies with long-term follow-up have been described. The Bernese periacetabular osteotomy (PAO) has gained popularity and supportive evidence over the past decade, with general good to excellent results in the majority of patients (4,5,6,7,8,9). Hip arthroscopy is a useful tool to address periarticular hip pathology. Labral tears and impingement morphology of the acetabulum and femur can be successfully addressed. However, there is limited evidence to guide the use of hip arthroscopy in the setting of DDH and structural instability. We propose that the vast majority of cases with definite DDH are best treated with correction of the underlying structural deformity via acetabular, femoral, or combined osteotomies. Recent studies indicate that isolated hip arthroscopy in the setting of DDH is one of the most common reasons for joint preservation failure (10,11) (Fig. 38.1). Nevertheless, there is a large spectrum of DDH severity, and borderline cases with questionable structural instability are challenging to diagnose and treat. As such, the optimal treatment of borderline dysplasia remains controversial. In such cases, isolated hip arthroscopy can be considered. This chapter examines the use of arthroscopy in DDH, the available evidence, and provides several case examples of hip arthroscopy utilized in the setting of DDH. We will focus on hip arthroscopy as an adjunct to osteotomy procedures and as an isolated procedure in selected cases of borderline dysplasia. The clinical presentation and diagnostic evaluation of DDH have been discussed in previous chapters of this book.
Definition of Dysplasia and Associated Structural Abnormalities
We utilize multiple clinical and radiographic parameters to define a hip as dysplastic, borderline dysplastic, or normal. Additionally, not every case of borderline dysplasia is associated with structural instability, and this delineation is important for selecting patients as candidates for hip arthroscopy. Each individual hip is critically evaluated by history, examination, radiographs, and advanced imaging to decide upon a treatment course. In diagnosing structural instability, we consider multiple factors including patient sex, clinical signs and symptoms, acetabular and femoral deformity, soft tissue integrity (laxity), and activity profile. Specific radiographic parameters include lateral center edge angle of Wiberg (LCEA), acetabular inclination (Tönnis angle), and anterior center edge angle of Lequesne (ACEA). The LCEA is calculated using the anteroposterior radiograph according to the technique described by Wiberg (12). Previously defined cutoff values for LCEA are used with measurements less than 20 degrees considered acetabular dysplasia, measurements between 20 and 25 degrees considered borderline acetabular dysplasia, and measurements greater than 25 degrees considered normal (13). Acetabular inclination (Tönnis angle) represents the horizontal orientation of the weight-bearing zone (sourcil) of the acetabulum and is defined by the angle created by the line connecting the inferior and lateral aspects of the acetabular sourcil and the transverse pelvic axis (14). Angles from 0 to 10 degrees are considered normal, angles 10 to 13 degrees are considered
borderline acetabular dysplasia, and angles greater than 13 degrees are consistent with acetabular dysplasia (15). The ACEA is calculated from the false-profile radiograph in the method of Lequesne and de Seze (15,16). We utilize angles less than 16 degrees as definite dysplasia, angles 16 to 20 degrees as borderline dysplasia, and angles greater than 20 degrees as normal. There is controversy regarding the normal values for the ACEA (17,18,19). Table 38.1 summarizes these parameters. It is important to note that the radiographic parameters of hip morphology must be interpreted in the context of all contributing disease characteristics.
borderline acetabular dysplasia, and angles greater than 13 degrees are consistent with acetabular dysplasia (15). The ACEA is calculated from the false-profile radiograph in the method of Lequesne and de Seze (15,16). We utilize angles less than 16 degrees as definite dysplasia, angles 16 to 20 degrees as borderline dysplasia, and angles greater than 20 degrees as normal. There is controversy regarding the normal values for the ACEA (17,18,19). Table 38.1 summarizes these parameters. It is important to note that the radiographic parameters of hip morphology must be interpreted in the context of all contributing disease characteristics.
Table 38.1 General Guidelines for Radiographic Parameters of Acetabular Dysplasiaa | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
The pathomorphology of DDH is commonly more remarkable on the acetabular side, yet the femur is often abnormal as well. The femoral head has variable size and shape, the neck can have excessive anteversion, the neck-shaft angle can be increased creating coxa valga, the greater trochanter may be displaced posteriorly, and a stenotic femoral canal can be present (20,21,22). Various combinations of femoral and acetabular deformities often produce structural instability which we believe are better treated with anatomical correction through acetabular and/or femoral osteotomy. Additionally, dysplastic hips are associated with a high percentage of aspherical femoral head deformities that after acetabular reorientation may produce secondary femoroacetabular impingement (FAI). In one retrospective study, patients having undergone PAO for DDH had a 72% incidence of a radiographically aspherical femoral head and 75% incidence of radiographically decreased head–neck offset, factors known to predispose to FAI (23




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree