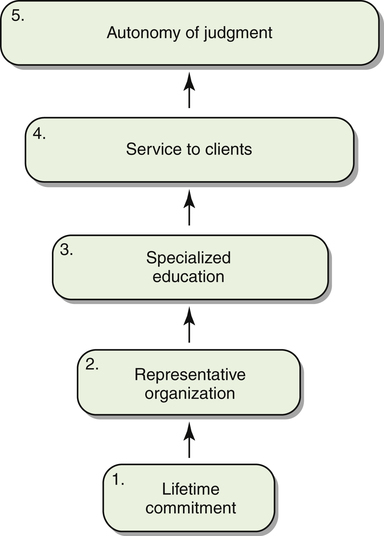
After reading this chapter, the reader will be able to: Part of the confusion regarding the definition of physical therapy results from the variety of legal definitions seen from state to state. Each state has the right to define the profession of physical therapy and regulate its practice. Such definitions are commonly included in legislation known as practice acts, which pertain to specific professions (practice acts are further described in Chapter 5). To limit the variety of definitions, the Board of Directors of the American Physical Therapy Association (APTA) created the Physical Therapist Scope of Practice (Box 1-1), which was originally titled Model Definition of Physical Therapy for State Practice Acts.2 This definition identifies several activities inherent in the practice of physical therapy. It uses language and terminology based on the Guide to Physical Therapist Practice (“the Guide”),3 a pivotal document describing the approach of the physical therapist (PT) to patient care. One of the fundamental concepts of the Guide is the five elements of the patient/client management model, and these are incorporated into the definition. (These are briefly described here. For more details on the elements of the model see Chapter 2.) First and foremost, physical therapy begins with an examination to determine the nature and status of the condition. An evaluation is then conducted to interpret the findings and establish a diagnosis and prognosis that includes a plan of care. Interventions are then administered and modified in accordance with the patient’s responses. Interventions focus on musculoskeletal, neuromuscular, cardiovascular and pulmonary, and integumentary disorders. Other important activities in the role of the PT include consultation, education, and research. These may be separate from, but ultimately contribute to, effective practice. The definition of physical therapy also reflects the areas of prevention; health promotion, wellness, and fitness; and consultation, all of which occur across the life span. Traditionally, PTs have provided care to patients—individuals who have disorders that require interventions to improve their function. Client is the term used to refer to an individual who seeks the services of a PT to maintain health or a business that hires a PT for consultation.3 These areas of involvement have become more significant in the recent development of the profession. In addition to identifying the activities of a PT, the definition states that physical therapy is “provided by or under the direction and supervision of a physical therapist.” This qualification is further stipulated in a section of another policy (adopted by the House of Delegates, the highest policymaking body of the APTA) specifying that PTs and physical therapist assistants (PTAs) working under the direction of a PT are the only individuals who provide physical therapy (Box 1-2).4 The definition of physical therapy provides a broad description of the scope of practice of physical therapy. A companion document addresses physical therapy as a profession (Box 1-3).5 This position was adopted by the House of Delegates of the APTA in 1983 and was subsequently revised to incorporate Guide language. Although the position states, “Physical therapy is a health profession…,” it does not offer a spectrum of characteristic evidence to support this statement. Perhaps one reason is the difficulty in conclusively defining a profession. Swisher and Page6 presented a comprehensive review of the variety of descriptions of a profession. They addressed definitions based on a description of characteristics, stages of evolution, or power, but they focused on three qualities commonly held in high regard: autonomy, ethical standards, and accountability. Distinct applications of these qualities were made to physical therapy. Moore7 also included autonomy in a description of a profession and positioned it at the peak of a hierarchy of characteristics (Figure 1-1). This description is particularly applicable to physical therapy. The first characteristic, a lifetime commitment requiring an individual’s dedication to the profession, is formidable yet admirable. PTs and PTAs do not commonly leave this profession. The second characteristic, a representative organization, provides standards, regulations, structure, and a vehicle for communication. In physical therapy this characteristic is fulfilled by the APTA. The third characteristic, specialized education, ensures competency to practice. For example, evaluative criteria for accreditation stipulate that the degree for professional-level PT education programs must be at the postbaccalaureate level and that the degree for PTA education programs is the associate degree.8,9 The fourth characteristic, service to clients, is obvious in physical therapy and provides a direct benefit to society. In this context the term “patients” would also apply. The final feature, autonomy of judgment, applies regardless of whether the therapist practices in a jurisdiction where a physician’s referral is required by law. Independent and accurate judgment is inherent in every evaluation, plan of care, and discharge plan conducted by the PT. This last criterion is frequently used to distinguish a professional from a technician (an individual who requires supervision). As a profession, physical therapy is guided by the criteria listed in Figure 1-1. Such was not always the case, and evolution of the profession has entailed significant change and varying degrees of recognition from other professions. The next section provides a brief overview of the history of physical therapy. Granger10 described how physical measures were used in ancient civilizations to relieve pain and improve function. Massage was used by the Chinese in 3000 bc, described by Hippocrates in 460 bc, modified by the Romans, and accepted as a scientific procedure in the early 1800s. Techniques of muscle reeducation developed from this evolution. Hydrotherapy was practiced by the Greeks and Romans through the use of baths and river worship. The development of electrotherapy began in the 1600s with the introduction of electricity and electrical devices. It is unfortunate that the impetus to develop physical therapy in this country was the response to widespread suffering; at the same time, such an origin demonstrates the direct humanitarian motivation that serves as the foundation of physical therapy. First came the epidemics of polio (poliomyelitis or infantile paralysis) in 1894, 1914, and 1916, which left tens of thousands of children paralyzed and in need of “physical therapy.” Then at the outbreak of World War I, the Surgeon General of the United States sent a group of physicians to England and France to learn about physical therapy techniques for the better management of those wounded in war. As a result, the Division of Special Hospitals and Physical Reconstruction was created in 1917.11 This division was responsible for training and managing reconstruction aides (exclusively women) who would provide physical reconstruction to those injured in war. These women were the forerunners of the profession and practice of physical therapy in the United States (Figure 1-2).
The Profession of Physical Therapy
Definition and Development
 Describe the characteristics of a profession
Describe the characteristics of a profession
 Describe a brief history of the profession of physical therapy in the United States and the major factors that influenced its growth and development
Describe a brief history of the profession of physical therapy in the United States and the major factors that influenced its growth and development
Definition
Physical Therapy as a Profession
Historical Development
Origins of Physical Therapy
Impact of World War I and Polio
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Profession of Physical Therapy: Definition and Development