Chapter 5 The pressure pain test
INTRODUCTION
In his tireless work on the nature of the auricular representation of the body Paul Nogier used a variety of methods to obtain what he called the ‘reactional information’ of every subject. Both evoked pain in the pinna at palpation and the application of cold and heat were repeatedly used for diagnostic purposes. For example he used the cold test, applying a rod of cold copper on the anthelix to localize any vertebral blockage. In this case he often found a reduced cold sensation on the representation of the vertebrae concerned which disappeared as soon as the blockage had been corrected with manipulation.
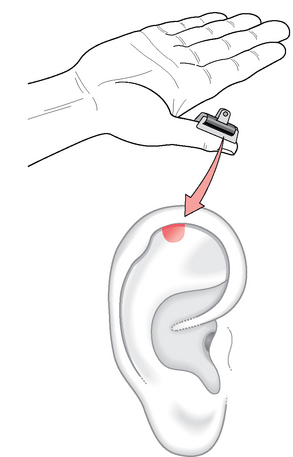
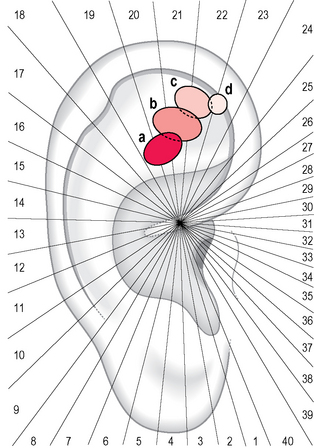
Nogier nevertheless realized that the most readily available technique for determining the reactivity of auricular reflex points was palpation and pressure pain test (PPT) applied to specific areas of the auricle. He wished, however, to approach this topic scientifically, so with his collaborator Bourdiol set up an experiment which is easy to realize and reproduce and which is now part of the history of ear acupuncture1 (Fig. 5.1). The procedure was as follows:
This experiment by Nogier and Bourdiol was repeated by Alimi2 applying functional magnetic resonance imaging (fMRI). The aim of the study was to examine the hypothesis that there are specific neurophysiological connections between ear acupoints and the central nervous system (CNS). A dynamometric clamp was calibrated at 2 kg/cm2 to induce a nociceptive stimulation of the thumb. To identify the auricular reflex points, instead of the pressure-probe an electronic microvoltmeter (Pointoselect DT+, manufactured by Schwa-medico) was used, selecting the points which had a variation of more than 3 SDs from the basic value of the auricular potential for every subject. Five paradigm stimulations were performed and real time fMRI brain signals were recorded in 10 healthy volunteers:
The results of Alimi’s experiment were that for 9 out of 10 subjects the stimulation of the needles produced a significant MRI signal, superimposed on that obtained by tactile stimulation of the thumb, on the presumed somatotopic projection of the thumb in the S1 somesthesic area. In three subjects recordings were obtained bilaterally; two of them showed the same phenomenon during tactile stimulation of the thumb.
We tried to repeat Alimi’s work reintroducing Bourdiol’s procedure: the auricular area representing the thumb was tested repeatedly 2 hours before fMRI with the pressure-probe to ensure its insensitivity.3 By immediately afterwards applying a dynamometric clamp calibrated at 2 kg/cm2, we identified the most tender point in the thumb area and marked it with ink. The subjects were right-handed healthy volunteers and we chose the left non-dominant thumb for the experiment. The following six recording sequences were carried out:
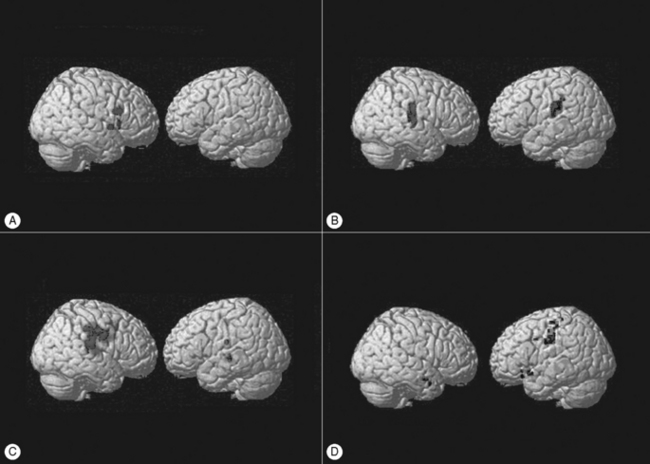
Figure 5.2A shows the activation of motor region M1 on the contralateral (right) side during sequence 2; Figure 5.2B shows the activation of the primary somatosensory cortex S1, during sequence 3, on the contralateral but also on the ipsilateral (left) side. The acupressure stimulation of the left auricular thumb point in sequence 4 as well as the mechanical stimulation of the inserted needle in sequence 6 demonstrate that the information is processed in several areas: the right somatosensory S1–S2 and frontal–prefrontal supplementary motor area cortices are activated during acupressure, whereas the ipsilateral primary somatosensory and motor areas are more focally activated during sequence 6.
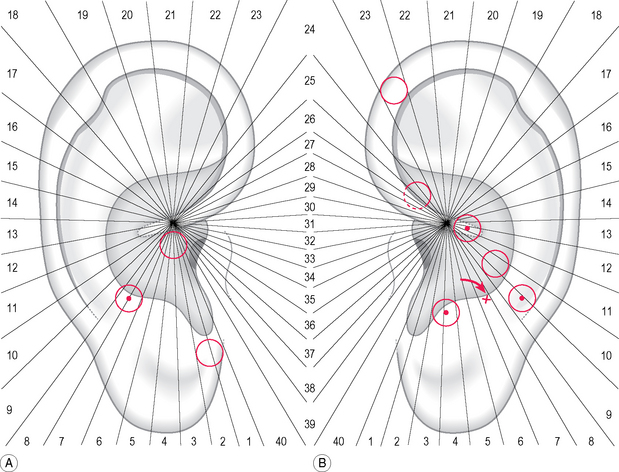
A 37-year-old female patient came for examination because she had been suffering with persistent headache of the frontal and nuchal region for a week. She was in her 20th week of pregnancy and did not wish to take any painkillers. She had never suffered from migraine before nor had any member of her family. The palpation of her auricles evidenced in total nine tender areas, three on the right (A) and six on the left (B)(Fig. 5.3). Four of these areas hid a tender point: three of them were directly related to her pain syndrome; the fourth, on the left stomach area, was included into treatment because she had suffered frequently with dyspepsia, both before and during pregnancy. Her pain score was 7 on the verbal numeric scale (VNS) at the beginning, and dropped to 4 after treatment, but a further point was needed (see arrow) for the pain to disappear.
WHAT IS THE SIGNIFICANCE OF A PAINFUL POINT ON THE EAR?
This question is not easy to answer since there are several confounding factors which may influence the tenderness of the auricle. Nevertheless we can assume that a healthy person, well balanced from the psychophysical point of view, shows a reduced number of tender points at PPT. We cannot, on the other hand, accept the reverse statement, since there are people who in certain circumstances, or for particular diseases, demonstrate a negative auricle.
Another confounding factor may be related to the normal functions of the body. Portnov, for example, observed that in 90% of healthy subjects the bladder point was sensitive. It was, however, sufficient to invite these people to empty their bladders to see an evident reduction of this tenderness.4
A further example is Bourdiol’s1 observation of a variation in auricular reactivity during digestion; in the hours following ingestion of food he was able to describe the auricular areas sensitized subsequently by the digestive process such as stomach, duodenum, gallbladder, liver, etc.
To verify the hypothesis that a healthy subject has a lower number of points compared to other subjects with any type of disorder, I examined a consecutive group of patients attending my general practice. My aim was to find a possible association between the presence of sensitive points and the scoring of the General Health Questionnaire (GHQ), developed by Goldberg for the screening of minor mental disorders in the field of general and community medicine. It is an easily understandable questionnaire, validated in several languages, which proposes a series of questions on general health during the preceding weeks. A significant correlation was found between the intensity of the health disorder and the GHQ scores.5,6
I examined 121 consecutive subjects of my practice with the reduced form of GHQ (30 items) and I obtained a significant regression line between the number of tender points and the GHQ score (Fig. 5.4). We may therefore assume that a tender point does not indicate only the suffering of the corresponding structure of the body, but more generally a psychophysical indisposition which may be only slightly expressed.
WHAT IS THE AVERAGE PAIN THRESHOLD FOR PRESSURE ON THE AURICULAR POINTS?
So far, a systematic study of the pain threshold of the different parts of the ear has never been carried out. One reason is perhaps that a consensus has never been reached on the methods to measure the degree of sensitivity felt when pressure is applied. Probably the simplest way is to ask the patient to indicate the point which is especially tender with either ‘Now’ or ‘There’. Alternatively, we could use the same range of numerical or verbal responses used by Oleson in his historical article on auricular diagnosis (see Fig. 9.1). He proposed a score of 1–4: 1 for low-level tenderness; 2 for medium-level tenderness; 3 for high-level tenderness; and 4 for extremely high-level tenderness. It is also worth noting the behavior of the patient reacting to the application of the pressure-probe by knitting his brows or demonstrating the well-known ‘grimace sign’ described by Nogier.
Another characteristic of the pain threshold of an auricular point is that it may vary when using the probe repeatedly: the threshold usually increases and this reset is probably due to the stimulation provoked by the PPT itself. This phenomenon, which is observable in almost every patient, has also been called ‘relativity of tenderness’. In my opinion it is not given sufficient consideration by those conducting clinical research, but may represent an interesting method for selecting points for treatment in a hierarchical order (see section ‘Which strategy should be used in selecting points?’ in Chapter 10).
WHAT IS THE GENERAL DISTRIBUTION OF TENDER POINTS ON THE OUTER EAR?
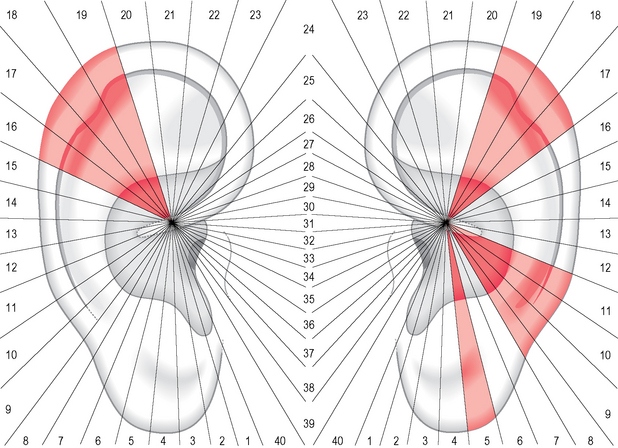
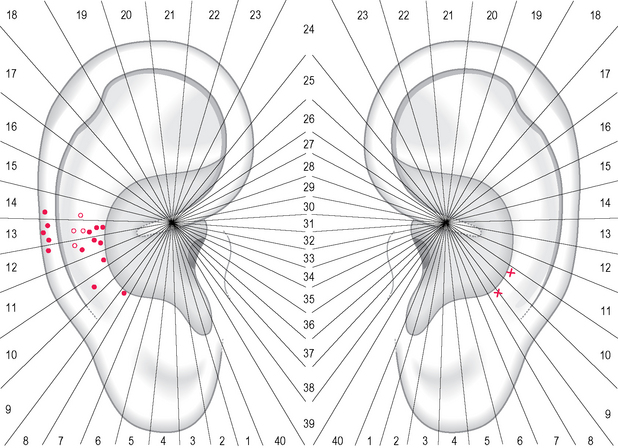
Since 325 patients examined blindly presented an equivalent number of tender points on the right ear and on the left ear (average 4.2 and 4.4), it would be natural to expect too a fairly equal distribution of points on both ears. This was not the case in my group of patients. Cluster analysis showed an asymmetrical distribution with a larger number of sectors of high value on the left ear (Fig. 5.5).
The larger number of sectors of high value on the left ear may indicate lateralization phenomena possibly associated with the laterality of cerebral functions of the human brain such as language, handedness, etc. (see Ch. 9).
THE ROLE OF PPT IN IDENTIFYING AREAS RELATED TO SYMPTOMS COMMONLY MET IN PRACTICE: THE MUSCULOSKELETAL SYSTEM
There are some important issues which have not yet been fully resolved, for example the different representations of the lower limb and the ‘shorter’ representation of the lumbar and cervical tract of the spine.
THE REPRESENTATION OF THE LOWER LIMB
The experienced acupuncturist knows very well that the representation of the lower limb is quite different in the French and the Chinese schools of thought. The Russian school, represented by Ruben Durynian, agreed with the Chinese and located the lower limb on the upper branch of the anthelix. The French map shows clearly that the lower and upper limb are separated by a neutral area, whereas on the Chinese map they are represented as being close together. The latter somatotopic arrangement is very similar indeed to that drawn by Bachmann in the first historical map of the ear (see Fig. 1.9). Some other drawn parts coincide with the later Chinese map, as for example the toe (AH2 zhi), whereas others coincide with the later French map, such as the heel; the knee was, however, reproduced on the boundary line between the fossa triangularis and the anthelix.
I would also like to direct the reader’s attention to some other somatic areas of Bachmann’s drawing which were faithfully reproduced on the standardized Chinese map, such as shoulder (SF4 and SF5 jian), clavicle (SF6 suogu), abdomen (AH8 fu) and chest (AH10 xiong) (see Fig. A1.2).
I made my contribution to the question of the representations of the lower limb by identifying the tender points using a pressure-probe of 250 g on selected patients affected by pain disorders on the different parts of the lower limb. Figure 5.6 shows the tender areas related to heavy coxarthrosis (nine cases), knee sprain (10 cases), ankle sprain (10 cases) and toe pain of traumatic origin (12 cases). As can be seen, the distribution of tender points, even in such small groups of patients, allows the identification of some partially overlapping areas which extend themselves from the fork of the upper and lower branch of the anthelix to the internal border of the helix. The axis of orientation of these areas lies in the middle, between the Chinese and French representations of the lower limb: it is possible therefore that both representations are valid, but also that the point to treat for a specific disorder needs to be identified case by case. Another possibility, however, is that different parts of the anatomical structure represented on the ear may have a different topography coinciding more with one map than with the other. This hypothesis was forwarded by Caterina Fresi using the needle contact test (NCT) for identifying the origin of knee and ankle pain. From her study it is possible that a knee pain caused by the injury of the medial capsule–ligament complex may sensitize sectors 21 and 22, whereas a disorder of the lateral complex may sensitize sectors 20 and 21. In a similar way a lesion of the medial malleolus of the ankle may correspond to sector 22, whereas the lateral malleolus appears to be represented more on sector 21 (see Fig. 8.5).
THE REPRESENTATION OF THE THORACOLUMBAR SPINE
As regards the ‘shorter’ representation of the thoracolumbar spine on the Chinese maps, the divergence with Bachmann’s reproduction of the spine is still mysterious. The puzzle is that both schools agreed with the representation of sciatic nerve but never reached a consensus on the representation of these parts of the spine. Nogier carried out what is probably the most accurate study, identifying single vertebrae of the thoracolumbar tract, one by one, through his system of radii centered on point 0 (see Fig. 3.19). Chinese acupuncturists, on the other hand, on the maps published before standardization, placed the lumbosacral vertebrae where Nogier located the thoracic tract of the spine. The neurophysiologist Durynian reproduced the thoracolumbar spine in his work in a similar way to the Chinese maps. On the standardized map the lumbosacral vertebrae (AH9 yaodizhui) occupy a large area of the anthelix which is separated from the sciatic area by the gluteus area (AH7 tun). This area seems to be a key area for the treatment of every kind of backache, even if Bachmann drew the gluteus point very close to that which was historically cauterized for sciatic pain.
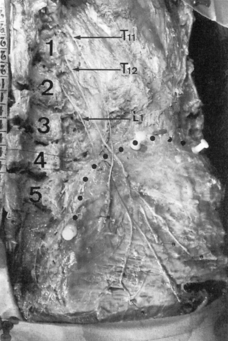
One of the authors who has faced this issue systematically for many years is Robert Maigne.7,8,9 He demonstrated that this pain commonly stems from the irritation of the lateral branch of the posterior ramus of the lower thoracic and/or the first lumbar spinal nerves, carrying motor and sensory fibers. Classically the cutaneous innervation of the lower lumbar and gluteal regions has been attributed to the cutaneous branches of L1–L2–L3. Anatomical dissections have shown, however, that the cutaneous innervation of the gluteal region originates more often from the lateral branches of the posterior rami of the nerves of T11–T12–L17 (Fig. 5.7).
Maigne confirmed the relation between the thoracolumbar tract of the spine and the iliac–gluteal region by a diagnostic block, injecting a solution of procaine 1 cm lateral to the spinal process directly into the joint region. After the injection, when the diagnosis of ‘thoracolumbar junction syndrome’ (TLJS) was correct, the backache disappeared and the skin-rolling test was subsequently negative. Maigne8,9 examined 320 patients with lumbago and found 138 patients with TLJS, 120 with low back pain (L4–L5 or L5–S1) and 62 of mixed origin.
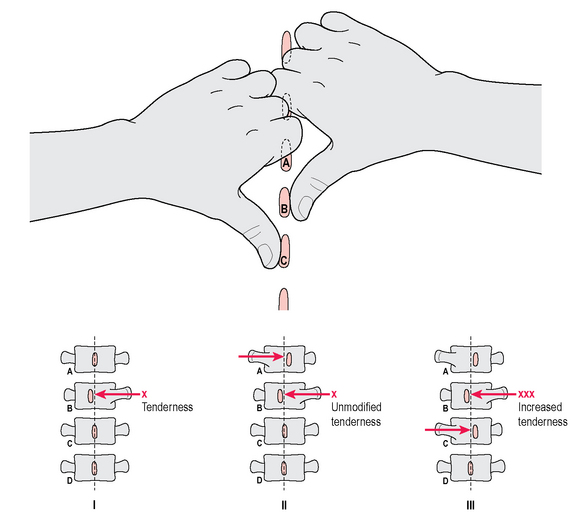
Before the diagnostic block, however, he systematically examined the spine segments from T9 to L5 with the patient prone. One of the most reliable methods for determining the source of pain was pressure applied by the thumb on the spinal processes both vertically and laterally, either from right to left or vice versa. Once a clear tenderness was elicited on one side, the contralateral side was challenged with the so-called ‘opposed thumbs technique’ on the upper and lower level (Fig. 5.8). As one of these movements provoked an increase in pain, the involvement of the two vertebrae was diagnosed by Maigne as a ‘minor intervertebral derangement’ (MID). In the group of 138 patients with TLJS mentioned above, 59.4% presented one MID, 26.1% two MID and 14.5% three MID. The first group showed MID at various levels, but in 75.6% the vertebrae involved were T11–T12 and T12–L1 (Table 5.1).
Table 5.1 Location of the ‘minor intervertebral derangement’ (MID) according to Maigne in 82 patients with thoracolumbar junction syndrome (TLJS)
| MID | Level | % |
|---|---|---|
| MID (1 level) | T9–T10 | 4.9% |
| T10–T11 | 12.2% | |
| T11–T12 | 41.5% | |
| T12–L1 | 34.1% | |
| L1–L2 | 7.3% | |
| Total | 100% |
When considering how to contribute to the issue of the ‘short’ lumbar spine I realized that the only possible way was to check the tenderness of the auricle before and after manipulation. Therefore I identified the MID with the opposed thumbs technique proposed by Maigne in a series of consecutive patients with possible TLJS. To ascertain the exact level of MID I placed in some patients a small metal disc 5 mm in diameter on the most painful spinal process before performing X-ray, as in the following case:
A 34-year-old male patient had been suffering for a few days from lumbago without pain radiating to his legs; the pain manifested abruptly after he lifted a weight. The most tender spot at pressure was on the right side corresponding to the spinal process of T11 (see the metallic disc in Figure 5.9). On the auricle of the same side I found one tender point on the anthelix and a second aligned on the helix (Fig. 5.10). After manipulations of the spine, as recommended by Maigne in rotation and extension for the relief of thoracolumbar disorders, the point on the anthelix lost its tenderness whereas the point on the helix remained partially sensitive.
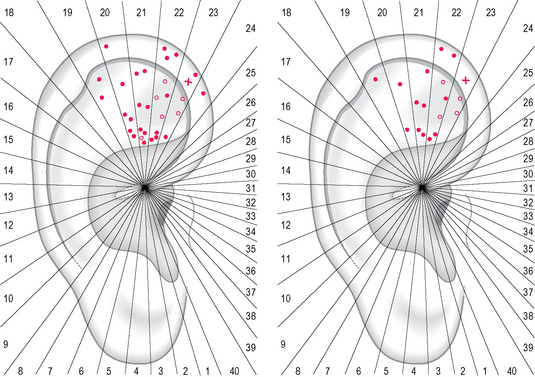
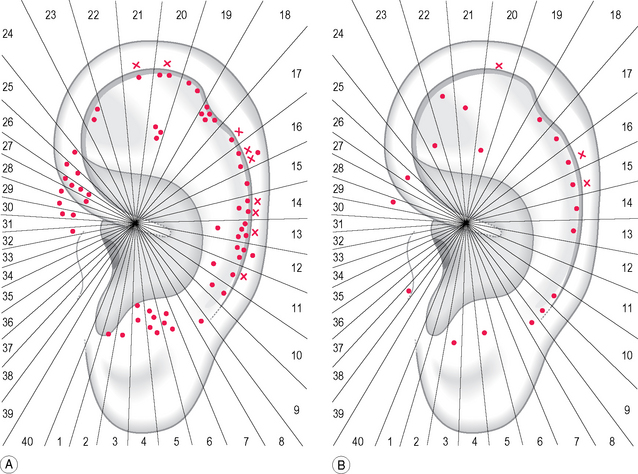
This experience permitted me to study a consecutive series of 10 male patients (average age 36.2 years) with lumbago and MID at the level of T11–T12, detecting the tender points before and after the manipulations described in the case study. Before manipulation two-thirds of the points were concentrated on sectors 18 and 19, especially on the anthelix (on the left of Fig. 5.11). After manipulation the total number of points decreased to 44.5% and only sector 19 maintained a higher concentration of points with respect to the other sectors (on the right of Fig. 5.11).
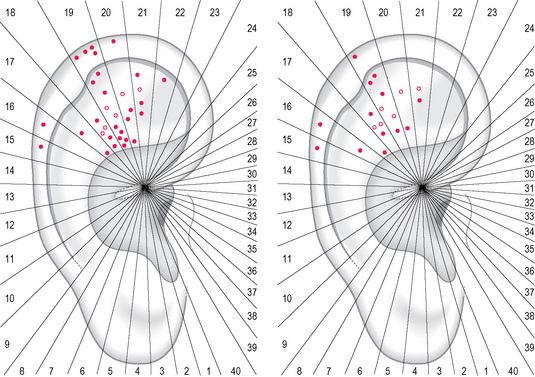
Fig. 5.11 Tender points in 10 male patients, average age 36.2 years, with lumbago associated with an MID in T11–T12, before manipulation (left) and after manipulation (right). Dots = lateral surface; circles = medial surface.
As a control group for my observations I examined 10 male patients (average age 47.6 years) with sciatic pain due to a disk lesion in L5–S1. The tender points were concentrated before the manipulation on sectors 21 and 22 (on the left of Fig. 5.12); after manipulation only sector 22 maintained a higher concentration of points (on the right of Fig. 5.12).
THE REPRESENTATION OF THE CERVICAL SPINE
A minor issue concerns the cervical tract of the spine which seems, like the lumbar tract, to be ‘shorter’ both on Nogier’s and the Chinese map. It is possible that the cervicothoracic junction could be represented higher up on the anthelix and the scapha.
The more cranial representation of the lower cervical vertebrae may be appreciated in Figure 5.13 which relates to five female patients with a mean age of 58.2 years suffering from cervical syndrome and radiation of pain consistent with a disk lesion at C6–C7. The distribution of tender points was mainly on sectors 12 and 13 (on the left of Fig. 5.13). In the case of a disk lesion at C7–T1 related points would probably be found above the horizontal line on sectors 14 and 15.
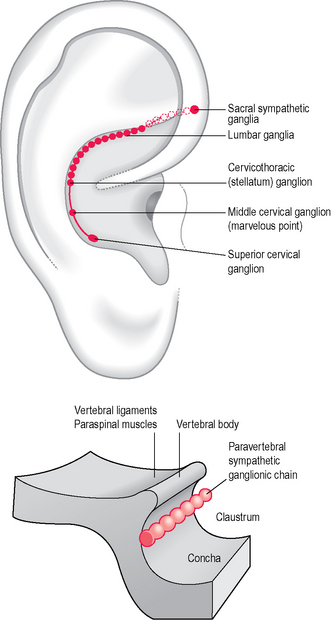
Regarding the cervical spine, for diagnostic and therapeutic purposes we must not forget the points on the internal border of the anthelix related to whiplash syndrome (on the right of Fig. 5.13). Depending on the modalities and strength of impact we may find one or more tender points in this area (representing the cervical sympathetic plexus according to Nogier and Bourdiol) which are very effective on accompanying symptoms such as headache and dizziness (Fig. 5.14).
THE ETIOLOGICAL PUZZLE OF FIBROMYALGIA
The diagnostic criteria of the American College of Rheumatology (ACR) for fibromyalgia syndrome include widespread musculoskeletal pain, morning stiffness and muscle fatigue for at least 3 months, accompanied by pain on palpation in at least 11 of 18 anatomically defined painful tender points.10 Other well known symptoms commonly observed are non-restorative sleep, depressive/anxious mood, fatigue and headache. The National Arthritis Data Workgroup11 reviewed published analyses from available national surveys and provided a prevalence estimate for the US of 5.0 million adults suffering with fibromyalgia. The etiology of fibromyalgia is as yet unclear and a co-morbidity has been described with irritable bowel syndrome (IBS), depression, chronic fatigue syndrome and tension-type headache.
Current hypotheses center on atypical sensory and pain processing in the CNS and dysfunction both of skeletal muscle nociception and autonomic nervous system.12 Seemingly therapies targeting central pain mechanism should give the best results; this is the reason why the US Food and Drug Administration recently approved pregabalin as the first specific medication for fibromyalgia syndrome.
As regards acupuncture, the systematic review of Mayhew and Ernst13 concluded cautiously that ‘the notion that acupuncture is an effective systematic treatment for fibromyalgia is not supported by the results from rigorous clinical trials. On the basis of this evidence, acupuncture cannot be recommended for fibromyalgia’.
As regards ear acupuncture and fibromyalgia, however, an interesting experiment is currently being carried out by my assistant Dr Riccardo Mazzoni on a group of patients who are members of Scudo Amico (Association for Fibromyalgia) in our city. In a still ongoing pilot study he included 16 selected patients for observation, according to the diagnostic criteria of the ACR (15 females and 1 male with an average age of 49.1 years), and treated them with ear acupuncture. Three patients dropped out of the study: one became pregnant during the therapeutic course and two others had an increase of the severity of pain during the first sessions. The remaining 13 patients received 10 weekly sessions of ear acupuncture. Figure 5.15 shows the distribution of tender points at the first treatment (on the left) and at the last treatment (on the right).
As is visually appreciable, 70% of the points lost their tenderness during the course of the therapy and this variation was accompanied by an evident improvement of scoring in the two scales adopted: the Psychological General Well-Being index (PGWB), a specific function and symptom questionnaire, and the Regional Pain Score (RPS).14
This line of points, very close to the helix, has been defined by Lange15 as the ‘vegetative groove’ and was supposed by the author to be essential for regulating the functions of a disturbed segment of the body according to Nogier’s principle of alignment.
The second interesting aspect is that while routinely examining some immunological parameters, high titers (between fifteen- and a hundredfold normal levels) of IgG of cytomegalovirus were found in 14 of the 16 patients. In addition, in two patients a high IgG level of the Epstein–Barr virus was documented. These findings may be fortuitous or may represent a further factor in the etiological puzzle of fibromyalgia. Some authors16 have indeed reported the possibility that viral infection or vaccination may be associated with this syndrome: the symptoms of fibromyalgia, such as myalgia and fatigue, would therefore appear to overlap considerably with those of a viral or atypical infection.
PSYCHOLOGICAL/PSYCHIATRIC AREAS DETECTED BY PPT
INTRODUCTION
The treatment of mental disorders would seem to be a promising field for acupuncture but there are some important issues which have slowed down research and hindered clinical application. One of these concerns the terminology and international classification of mental disorders (DSM IV) which is being accepted only gradually by Chinese physicians (see also section entitled ‘The diagonal ear lobe crease or Frank’s sign’ in Ch. 4). For example, several textbooks on ear acupuncture still use outdated or obsolete terms such as neurasthenia, neurosis, hysteria and only a few authors use recent terms such as anxiety and/or depression.17–19
The reader may consult Figure A1.16 and check for the terms adopted in the standardization process. He will agree that the list of psychological/psychiatric terms is reduced and still incomplete. For example, the indication for depression has been adopted only for the liver area. The situation does not look any better if we examine Nogier’s psychological points which appear to be more the result of a process of anecdotal evidence built up over time rather than systematic research on auricular areas and their association with specific mental disorders. The classical points identified by Nogier are those for fear and aggressiveness on the anterior part of the ear lobe; the Jérôme point for depressive disorders on the transition zone between the scapha and ear lobe; the anxiety point on the stomach area; and the internal border of the anthelix for treating dysfunctions of the vegetative system. Something else to remember is the historical line connecting the point of aggression with the so-called omega points which were presumed to regulate psychological stress (ω), visceral stress (ω1) and somatic stress (ω2). A further point for regulating mood was presumably the representation of the hypothalamus on the posterior part of the antitragus20,21 (see Fig. A1.15).
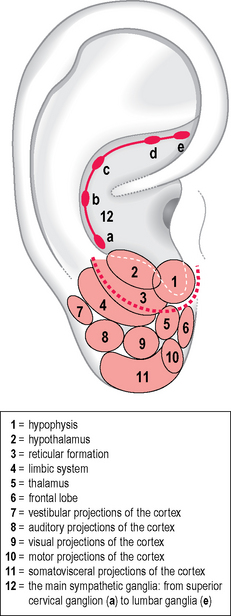
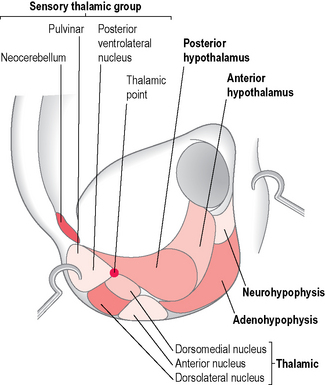
The neurophysiologist Durinyan,22,23 presenting an original somatotopic arrangement of the CNS, offered me some interesting clues for the development of my research in the psychosomatic area. He circumscribed the antitragus and the intertragic incisure in the same functional area, considering them as related to the hypophysis, the hypothalamus and the reticular formation (Fig. 5.16). Durinyan’s intention was probably to attribute a greater extension to this area, according to the principle of the homunculus on the auricle. Interesting, moreover, on his map, are the representation of the frontal lobe on the anterior part of the ear lobe and the representation, in a totally different position to Bourdiol’s, of the limbic system on the posterior part of the ear lobe and on the junction with the scaphoid groove (see Fig. 4.13).
STRESS RESPONSE AREAS
Even 20 years ago, when my interest in psychosomatic disorders began to develop, I was disappointed by the lack of rationale and consensus on many of the above-reported points/areas. In particular, with a few exceptions, I could not find points which could be clearly defined as having an anxiolytic or antidepressant effect. I became aware, however, when systematically using a pressure-probe to examine patients with symptoms of possible psychosomatic origin, that the auricle presented a more or less constant sensitivity in some specific areas. I started therefore to study the auricular ‘stress response’ of those patients who associated the onset of symptoms such as tachycardia, dyspepsia and IBS with some particular stressful life events that had occurred in the previous months. Applying tools such as the Paykel scale24 for life events I was able to measure the number of stressful events that had occurred in the previous 6 months and their objective impact using a five-point scale. I added a distress scale, Kellner’s Symptom Rating Test (SRT),25 which is a combination of subscales scoring anxiety, depression, somatization and inadequacy.
A group of 50 patients with one or more of the functional symptoms mentioned above, for which all possible investigation had been negative, were compared to 20 volunteers without any of those symptoms.26
The first information I obtained from this study, published several years before those of Wang,27,28 was that ear acupuncture may have a rapidly balancing effect on parameters such as anxiety, depression and somatization. This positive effect is more pronounced in patients with stress-related symptoms, but also measurable in apparently symptom-free subjects.
This hypothesis may be supported by the fact that stress response seems to sensitize the auricles on recurrent areas and some of them have a significantly higher number of points. I identified in 50 subjects with stress response at least nine areas with a variable concentration of points (Fig. 5.17): the first ranked area (number 5, summing 44.9% of the total in the stress group) may be associated with both Triple Energy (CO17 sanjao) and the neighboring endocrinal area (CO18 neifenmi) of the standardized map. This area corresponds to the representation of the hypophysis for Durinyan and the representation of the hypothalamus for Bourdiol (Fig. 5.18). In second place I identified area number 4 (16.3% of the total) on the tragus, which may be associated with the adrenal gland shenshangxian or Nogier’s adrenocorticotropic hormone (ACTH) point on the internal wall of the tragus. Next came area number 6 (8.8% of the total), which is rather a broad one overlapping with both the heart (CO15 xin) and spleen (CO13 pi) zones, corresponding on Bourdiol’s map to the upper cervical sympathetic ganglia (see Fig. 5.14). In decreasing order came the other zones on the anterior part of the ear lobe, on the Shen men area, etc. (Table 5.2).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree