The Neuromuscular Hip
Mathias P.G. Bostrom and Michael B. Cross
Key Point
Introduction
Although relatively rare, adult patients with hip pathology secondary to neuromuscular disorders remain a unique and varied group of patients who require different approaches to the care of their hip disease. The goal of this chapter is to describe the unique nature of these pathologies while presenting appropriate treatment algorithms for the care of these special patients and their hip pathology.
Although the definition varies among clinicians, in this chapter we will define a neuromuscular disorder as any disease that involves any part of the muscle or nerve. This includes myopathies, muscular dystrophies, upper and lower motor neuron diseases/injuries, neurodegenerative disorders, movement disorders, and diseases of the neuromuscular junction. Similarly, we will define adult neuromuscular hip disorders as pathology of the hip directly or indirectly caused by neuromuscular disease states. These disorders can be categorized further into intrinsic and extrinsic disorders.
In the literature, it has been shown repeatedly that muscle imbalance about the hip caused by an underlying neuromuscular disease can result in subluxation and dislocation of the hip in growing children and may predispose adult patients to degenerative joint disease of the hip. Specifically, the muscle imbalance that directly causes acquired hip instability and dysfunction is due to the presence of strong hip flexors and adductors that overpower weaker or absent hip extensors and abductors. Although the direct cause of the instability is this muscle imbalance, the underlying cause of the hip dysfunction may involve intrinsic or extrinsic factors. Intrinsic muscle imbalance about the hip manifests during childhood and plays the primary role in subsequent hip problems. Extrinsic causes of neuromuscular imbalance occur in stable hips and play a secondary role in the development of osteoarthritis and contractures in later life.
The two basic types of paralysis or paresis are flaccid paralysis, which is caused by injury to the lower motor neurons or peripheral nerves, and spastic paralysis, which is caused by injury to the upper motor neurons or the cortex of the brain. In approaching the neuromuscular hip, certain differences between flaccid and spastic paralysis must be delineated. The spastic muscle has increased tone and often functions in both phases of gait (i.e., in phase and out of phase). The flaccid muscle has decreased tone but always functions according to its normal role. Both spastic and flaccid types of pareses are found in both intrinsic and extrinsic disorders.
Extrinsic movement disorders, such as dyskinesis, athetosis, Parkinson’s disease, and multiple sclerosis (which may be more specifically classified as a demyelinating disorder), may have elements of spasticity, but hip subluxation-dislocation is rare in this group of patients because the onset of disease usually occurs after growth is complete. However, movement disorders are frequently associated with contractures about the hip, and these patients often develop painful degenerative arthritis.
On the other hand, children who are born with intrinsic neuromuscular disorders (e.g., cerebral palsy, myelomeningocele), or in whom a neuromuscular affliction occurs while the hip is still in early development (e.g., poliomyelitis, encephalitis, cerebrovascular accident, childhood spinal cord injury, brain trauma), are at increased risk for hip subluxation-dislocation. In these children, frequent examinations and hip x-rays can detect and even predict those hips at risk. If detected, botulinum toxin A injections, early muscle releases or transfers, and appropriate varus rotation femoral osteotomies can improve hip stability. Still, in spite of treatment, a number of hips remain subluxated or dislocated and thus can be a source of pain and disability in the adult.
Although diminished sensation itself plays no role in hip instability, the lack thereof is an important consideration in planning surgery, as well as in the prognosis of the joint. For example, intact sensation is usually present in cerebral palsy but may be diminished in adult patients who have had a cerebrovascular accident. Additionally, myelomeningocele patients have significant loss of sensation, but polio patients have intact sensation.
Sensation in general does not play a role in hip instability; however, compromised proprioception may play a role. Clearly diminished or absent proprioception, whether it existed preoperatively or was compromised as the result of surgery about the hip, may cause instability after total hip arthroplasty. Unfortunately, assessing proprioception about the hip is challenging clinically, and therefore truly assessing its role is difficult.
Intrinsic Disorders
Spasticity
Among intrinsic neuromuscular hip disorders, major causes of spasticity include cerebral palsy, cerebrovascular accident, and spinal cord injury in the young child. Despite differing origins, the hip pathology seen in these patients is similar; thus their treatment may be approached in a like manner. Among the more severely neurologically affected children with any one of these disorders, hip subluxation or dislocation often occurs. As was noted earlier, the direct cause of hip instability is muscle imbalance resulting from strong hip adductors and flexors overpowering weaker hip abductors and extensors. Coxa valga, increased femoral anteversion, and pelvic obliquity also contribute to the problem of hip instability. However, scoliosis plays less of a role, except for its relationship to pelvic obliquity. In the subluxated or dislocated hip, the uncovered femoral capital epiphysis becomes deformed and often becomes associated with painful arthritic changes later in life. Early treatment during childhood consists of nonoperative measures such as physical therapy, bracing, wheelchair modifications, botulinum toxin A injections, and operative treatment, including muscle releases and transfers to obtain muscle balance and early varus rotation femoral osteotomies to better stabilize the hip(s). When the acetabulum is deficient, acetabuloplasty should also be considered as operative treatment. Although these procedures may be suitable for the growing child, salvage operations are usually necessary in the treatment of adult patients.
In the adult patient, regardless of the cause and ambulatory status, the goal of treatment is to preserve or restore a functional range of painless hip motion in all patients. In the cerebral palsy population, the most severely involved patients (e.g., spastic quadriplegics) have the greatest frequency of mental retardation and seizure disorder, and often suffer from malnutrition, especially if they reside in large institutions. They are also the most likely patients to develop subluxation or dislocation of the hip. In fact, the incidence in this group is reported to be as high as 50% to 60%. Further, among hips that dislocate, approximately 50% will become painful. In addition to causing pain, subluxation-dislocation of the hip is often accompanied by contractures (e.g., adduction and/or flexion), which prevent standing, limit or prohibit sitting, and make perineal care difficult.
Therefore, the goals of treatment of the adult spastic neuromuscular hip are twofold: (1) prevent contractures, and (2) if the dysplastic hip becomes painful or the sitting position and perineal care become difficult because of contractures, perform salvage procedures to improve function and eliminate pain.
The uncovered, unprotected, growing femoral capital epiphysis is subjected to deforming forces from overlying spastic hip abductors and the tight superior capsule, and to the pressure of the elongated and hypertrophied ligamentum teres. The former two produce the pathognomonic flattening of the superolateral portion of the spastic subluxated-dislocated femoral head, and the latter, that is, the ligamentum teres, produces medial notching. The combination creates the typical “triangulation” effect (Fig. 80-1).

Figure 80-1 Radiograph of a hip demonstrating the “triangulation” effect with flattening of the superolateral femoral head caused by spastic hip abductors and a tight superior capsule, and medial notching of the head caused by the ligamentum teres.
In young children who still have significant growth, a deformed femoral head can remodel after reduction. In early adult years, if the femoral head is not deformed, femoral and pelvic osteotomies may achieve adequate femoral head coverage with functional range of motion. On the other hand, in the adult, if the femoral head is deformed, repositioning it in the acetabulum will result in an incongruous and painful joint. Valgus or Schantz pelvic support osteotomies may relieve hip pain, but the abducted position of the hip may prevent wheelchair sitting, which is essential for the severely involved patient. As outlined by the treatment algorithm in Figure 80-2, the three traditional treatments of the painful, dislocated hip in the adult are (1) head-neck resection with or without interposition arthroplasty, (2) hip arthrodesis, and (3) total hip replacement.
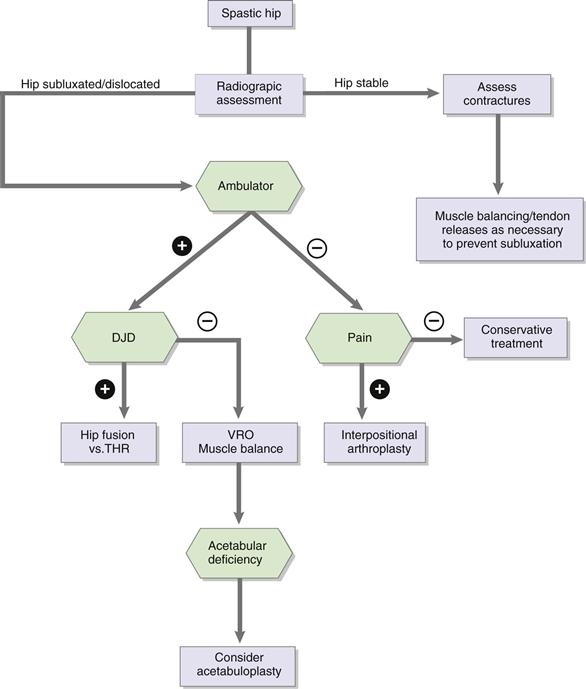
Figure 80-2 Treatment algorithm for the spastic hip.
Head-Neck Resection and Interposition Arthroplasty
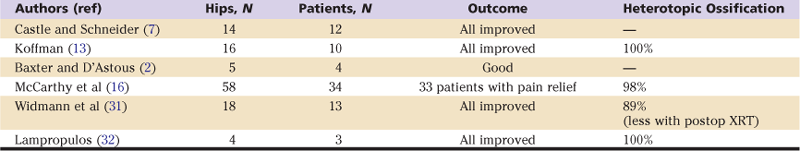
Resection arthroplasty, as described by Girdlestone,30 has not been traditionally recommended for spastic cerebral palsy patients, given its high incidence of stiffness, seating difficulty, heterotopic ossification, and proximal migration of the femur.31 Castle and Schneider in 1978 were the first to describe an extensive proximal femoral resection with interposition arthroplasty. In this operation, the proximal femur is resected below the level of the lesser trochanter, the capsule is closed over the acetabulum with the detached end of the iliopsoas tendon, and the vastus lateralis is sutured over the stump of the proximal femur. Then, the abductor muscle mass is interposed between the two (Fig. 80-3). In their series, they reported good long-term pain relief, improved sitting, and ease of perineal care in 12 patients (Table 80-1).7
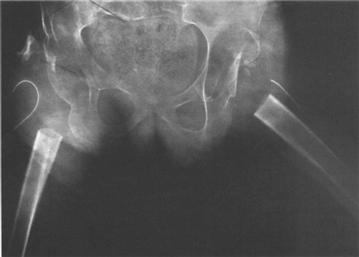
Figure 80-3 Anteroposterior radiograph of a pelvis demonstrating bilateral proximal femoral resections.
Table 80-1
Interpositional Arthroplasty in Cerebral Palsy
XRT, Radiotherapy.
This technique was further modified by McCarthy and associates, who published the largest series to date in 1988 by combining the results of groups of severely neurologically involved, institutionalized patients from Massachusetts and Arkansas. In their procedure, using extraperiosteal dissection, they resected the proximal femur to 3 cm below the level of the lesser trochanter (at a line drawn from the distal ischium); they performed this procedure on 58 proximal femurs in 34 patients, with ages ranging from 15 to 60 years. Pain was relieved and sitting was improved in 33 of the 34 patients. Still, ectopic bone was noted in 53 hips: 32 with just capping of the proximal femur, 12 hips with a lateral spike of the proximal femur, and 9 with bone interposed between the acetabulum and the femur. However, only 3 hips required revision because of heterotopic bone formation.
McHale and colleagues described a procedure that included adductor release, resection of the femoral head and neck, valgus proximal femoral osteotomy to achieve 45 degrees of abduction, suturing of the psoas tendon to the ligamentum teres, and capsulorrhaphy, followed by postoperative spica casting for 3 weeks. In all 5 patients, investigators noted improved sitting, pain, and range of motion with no cases of proximal femoral migration and less heterotopic ossification.
In 1999, Widmann and coworkers reported on outcomes at The Hospital for Special Surgery (HSS). In all, 13 patients (18 hips) with an average age of 26.6 years underwent proximal femoral resection–interposition arthroplasty. Postoperatively, 6 hips were treated with skeletal traction and 9 hips were treated with skin traction. Five hips in the study had postoperative localized radiation at 700 cGy. Investigators reported statistically significant improvements in pain, perineal care, and sitting ability. In addition, range of motion improved with respect to flexion, extension, and especially abduction, where motion improved from 10.6 degrees preoperatively to 43.6 degrees postoperatively. In addition, a significant difference in postoperative heterotopic ossification was noted among patients treated with postoperative radiation. No difference in proximal femoral migration occurred in patients treated with skin traction, as opposed to skeletal traction.
Still, although Bleck was an early proponent of head-neck resection, the incidence of recurring pain and heterotopic bone formation has altered his advocacy.4 Because of poor results, several authors have abandoned this procedure. In 2008, to combat the problem of proximal femoral migration and to allow for immediate upright sitting, Lampropulos and associates published results in a series of 4 hips in 3 patients who had undergone proximal femoral resection–interpositional arthroplasty as described by Castle and Schneider, with the addition of an external fixator for articulated hip distraction. All patients showed improvement in pain, perineal care, and sitting tolerance. One patient had proximal femoral migration above the level of the acetabulum with associated pain requiring a revision resection, and all patients had some degree of heterotopic ossification that did not interfere with outcomes. Complications associated with the external fixator were not seen.32
Although most authors have achieved favorable results with this procedure, it is important for the clinician to understand the limitations and contraindications of the procedure. Proximal femoral resection is contraindicated in walking patients because the restored limb cannot bear weight. It should not be performed in young, growing children because of upward migration and heterotopic bone formation in this group, which usually occur by the third to the fifteenth week. Furthermore, notwithstanding the complexity of attempted reconstruction, in the young child the potential for achieving satisfactory hip function with reduction and appropriate osteotomies makes this far preferable to proximal femoral resection. Finally, in all patients following proximal femoral resection, pain may be present for several months.
Hip Arthrodesis
Arthrodesis of a painful hip joint has been a time-honored orthopedic solution for treatment of the painful arthritic hip in the young adult; however, its use in neuromuscular disorders about the hip is less well documented. Indications for arthrodesis include disabling hip pain, a normal contralateral hip, and no evidence of spinal deformity. Thus, because most painful, subluxated, or dislocated hips occur in severely neurologically involved patients who have contralateral hip dysplasia, as well as spinal deformity, hip arthrodesis as a surgical option in this population is relatively limited. Advantages of a successfully arthrodesed hip include elimination of pain, improved ability to sit and stand, and long-term durability. Disadvantages include the high incidence of failure and the need for prolonged postoperative immobilization. The latter may be reduced or eliminated with the use of larger and stronger internal fixation devices such as an AO-Cobra plate or the use of an external fixator. Although these stronger internal devices may improve fusion rates, they should be used with caution because a possible future total hip arthroplasty may be compromised if the abductor muscles are excessively weakened.
In 1986, Root and colleagues reported on 8 cerebral palsy patients with ages ranging from 13 to 34 years who had unilateral hip arthrodeses.22 All patients had painful arthrosis of the hip associated with subluxation or dislocation. Of the original 8 patients, 6 fused successfully and 2 required revisions. One of the revisions was ultimately converted to a total hip replacement. Fucs and coworkers published the largest series in 2003, when they analyzed 14 patients with spastic cerebral palsy and painful chronic hip dislocations or subluxations that were treated with hip arthrodesis.51 Six hips were stabilized with an AO-DCP 4.5-mm plate, 4 hips with an AO-Cobra plate, and 3 hips with 6.5-mm cancellous screws. One hip was initially stabilized with Kirschner wires and went on to develop a nonunion, which was eventually revised with a Cobra plate. A hip spica was used on 8 patients, and 1 of the patients who was not casted developed a nonunion. Among the 14 hips, 11 hips fused without a nonunion. Three patients developed a pseudarthrosis with aseptic loosening of the hardware requiring reoperation, and all 3 cases eventually fused. All patients noted relief of pain, and of the 3 sitting patients preoperatively, 2 became household ambulators postoperatively. In addition, most of the bedridden patients became sitters, and ambulatory patients maintained or improved their ambulatory status.
Total Hip Arthroplasty
Total hip replacement is a successful treatment option for painful hips in cerebral palsy, regardless of whether the hip is dislocated. Contrary to Koffman’s poor experience with total hip replacement in 5 patients reported in 1981,13 the experience of the HSS of 19 total hip replacements in 18 patients with an average follow-up of 10 years was remarkably good.6 Whereas Koffman used various constrained prostheses, the HSS series reported no constrained total hip replacements. In addition, all acetabular and femoral components in the HSS series were fixed with polymethylmethacrylate. Four hips had bone graft augmentation for a deficient acetabulum. Notably, a postoperative hip spica cast was used in 16 of 18 patients to prevent dislocation and promote healing of the greater trochanter. Pain was completely resolved at long-term follow-up in 16 of 18 patients, and 12 patients improved by at least one functional category. Two patients had recurrent dislocation because of component malposition, and both had successful revisions. Thus, survivorship was 95% at 10 years when the endpoint was loosening, and 86% when the endpoint was revision for any reason. Similar results were published in 2009 by Schroeder and associates, who reported on 18 total hip replacements in 16 ambulatory cerebral palsy patients. However, their series had slightly higher dislocation and acetabular loosening rates.33
Indications for performing a total hip replacement in the spastic patient include the following:
1. Hip pain refractory to medication.
2. Decreased function in standing, limited sitting, and difficulty with perineal hygiene.
3. Potential standing or walking, transfer ability, or upright sitting in a wheelchair.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








