3 The Lateral Approach in Total Knee Arthroplasty
Patient Presentation and Symptoms
Patients presenting for total knee arthroplasty (TKA) experience considerable pain, swelling, and various types of angular deformities that produce instability and functional disability. Surgical approaches to the knee should enable the surgeon to access the knee in the safest, most direct manner that allows for predictable stability at the patella—femoral and femoral—tibial interfaces. The direct lateral approach is a technique that offers many advantages in correction of the fixed valgus deformity.
Indications
- Fixed valgus deformity with patella subluxation
- Partially correctable valgus with lateral orientation and/or patella subluxation
- Varus knee with severe tibial rotation, increased Q-angle, tight retinaculum, and iliotibial band (ITB) with patella tilt or subluxation
- Grossly unstable knee in a rheumatoid with expanded suprapatellar pouch
- Previous lateral incisions in multiply operated knee, when skin is at risk (with undermining)
- Lateral unicompartmental replacement
Contraindications
- Fixed varus deformity
- Neutral, or mild valgus knees with normal patella tracking and without tight lateral soft tissue structures
- Previous medial incisions in multiply operated knee
- Surgeon unfamiliarity with lateral knee anatomy
Physical Examination
- Valgus knee deformity, usually fixed/noncorrectable to a physiologic biomechanical axis
- Tight lateral retinaculum with patella tilt or subluxation
- Tight ITB
- Increased Q-angle with lateral positioning of Gerdy’s and the tibial tubercle
- External tibial rotation
- Unstable medial sleeve (severe type II valgus)
Diagnostic Tests
- Standard x-rays to include
- Erect weight bearing
- Lateral flexion/extension
- Skyline patella
- Erect weight bearing
- Long film to include hip/ankle
Special Considerations
- Fixed lateral contractures require sequential releases that include the capsule, ITB, vastus lateralis (VL) tendon, lateral collateral ligament (LCL), and at times the popliteus, lateral gastrocnemius, and inner aspect of the fibular head (preserving and lengthening the LCL). These releases are best addressed by the direct access using the lateral approach.
- Valgus deformity (developmental) is most common in females (95%) with a higher percentage of rheumatoid patients. Patients tend to be more fragile from a bone (osteopenia) and soft tissue standpoint. Minimal surgical soft tissue trauma with avoidance of undermining skin flaps is critical.
- Use of revision (stemmed components) should be considered if bone quality is an issue, especially in the rheumatoid patient.
- Atrophy or pressure resorption of the lateral femoral condyle distorts the normal anatomy. Measured bone resection techniques, used with some TKA instrumentation systems, must be modified because minimal resection of the atrophic lateral femoral condyle is the norm. Bone graft or augments of the lateral femoral condyle may be required in extreme cases.
- The varus knee with
- excessive rotation/internal tibial torsion (extraarticular deformity)
- lateral tubercle (patella tendon) positioning
- tight retinaculum/ITB is at high risk for patella maltracking. The lateral approach is an option, with or without tibial tubercle transfer to medialize the patella tendon insertion.
- Atrophy or pressure resorption of the lateral femoral condyle distorts the normal anatomy. Measured bone resection techniques, used with some TKA instrumentation systems, must be modified because minimal resection of the atrophic lateral femoral condyle is the norm. Bone graft or augments of the lateral femoral condyle may be required in extreme cases.
Preoperative Planning and Timing of Surgery
- Similar to routine TKA protocol
- Long film to include hip-knee-ankle
- If severe hindfoot deformity is present, consider foot surgery first.
- If ipsilateral hip osteoarthritis, especially with high valgus angle, consider total hip arthroplasty (THA) first. Extreme circumstances may warrant consideration of simultaneous THA and TKA.
- If extraarticular deformity (>15 degrees) or fixed valgus (>30 degrees) with unyielding (at risk) soft tissue/skin, consider a supracondylar osteotomy as a first-stage TKA.
Special Instruments
- A modern TKA instrument system that allows for proper rotational positioning of the femoral component
- Reference to the tibial axis with balanced flexion tension or to the transepicondylar axis will be most reliable.
- Beware of rotational variables and landmark identification in severe cases.
- Reference to the tibial axis with balanced flexion tension or to the transepicondylar axis will be most reliable.
- Newer navigation systems may prove valuable in the future.
Anesthesia
Single shot spinal with epinephrine and Duramorph is preferred; epidural, general anesthesia acceptable. Consider femoral nerve block.
Figure 3-1 Skin incision.
Patient Position
- Supine with lateral bolster to counter external rotation
- Tourniquet optional, especially in very short, obese patients
Surgical Procedure
Skin Incision
The skin incision (Fig. 3–1) is placed over the lateral patella border, extending proximally along the VL and distally between Gerdy’s tubercle and the tibial tubercle. Previous anterior or lateral incisions should be utilized and extended proximally and distally to avoid potential for skin necrosis.
Iliotibial Band Release/Lengthening
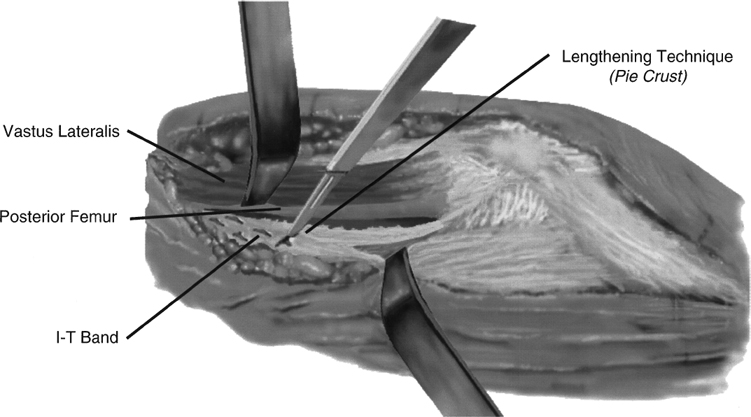
The ITB is exposed proximally by separating the inner fascial sleeve from the VL muscle (Fig. 3–2). The band is released from the posterior femur and “finger stripped” to the posterolateral corner. A varus stress at the knee joint will “bow-string” the tight fascial bands, allowing for a multiple puncture “pie-crusting” lengthening under visual and digital control. The release is performed approximately 10 cm proximal to the joint line. The peroneal nerve can be palpated or explored, but this is seldom required and not recommended except in very severe cases.
Lateral Retinacular Incision (Superficial Layer)
The course of the lateral parapatella incision begins 2 to 4 cm lateral to the patella and extends distally into the midportion of Gerdy’s tubercle (Fig. 3–3). Proximally, the incision extends into the central quadriceps tendon. The lateral arthrotomy separates the superficial from the deep layers; therefore, proceed cautiously through the outer layers.
Lateral Arthrotomy (Deep Layer)
The superficial layer is separated from the deep layer with a coronal plane Z-plasty, from superficial lateral to deep medial (Fig. 3–4). Proximally, an oblique arthrotomy incision from the lateral to medial takes advantage of the laminated anatomy of the central quadriceps tendon. The VL tendon is unyielding but substantially thick and allows for a horizontal (coronal) plane expansion release as shown. The VL tendon incision begins near the musculotendinous junction and ends distally at the midcoronal plane of the patella insertion. The midportion (lateral retinaculum) separates naturally from the deep capsule and fat pad. The capsule is incised from the patella rim. The fat pad incision continues obliquely to the inter-meniscal ligament, retaining approximately 50% of the fat pad with the patella tendon and 50% with the lateral sleeve, which includes the lateral meniscus rim for increased soft tissue stability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








