CHAPTER 29 The Immature Spine and Athletic Injuries
Most spine injuries in athletically active children and adolescents are chronic, resulting from repetitive demand on the immature spine during participation in sports. The most serious injuries are acute as a result of direct trauma. The age at which a child can be considered an athlete varies and may be 3 years old when a child puts on skis or 10 years old when he or she begins to ride bulls (Fig. 29–1). Several sports, such as skiing, football, and horseback riding, involve increased risk of acute traumatic events, making spine fracture a significant concern when considering an adolescent athlete. This chapter discusses the initial evaluation and on-field management of spine fractures; the complete treatment of spine fractures is covered elsewhere.
According to surveys of patients seen in sports medicine specialty clinics, the most common cause of back pain in adolescent athletes is stress fracture, or spondylolysis. Spine hyperextension and repeated twisting contribute to the high rate of spondylolysis seen in sports such as gymnastics, football, and weightlifting. The rate of spondylolysis in gymnasts is 20% compared with 5% to 6% in the general population.1
Principles of Diagnosis
History
The term interview implies an interaction with the patient as opposed to the traditional notion of extracting information from the patient. When allowed to tell his or her story, an adult patient takes an average of 90 seconds.2 Adolescents tend to be more taciturn and talk less than the average adult. The average physician cuts off the patient with a question after 18 seconds because he or she has formed a differential diagnosis. Such interruption stops the flow of information, and often the patient is never permitted to relate pertinent facts.
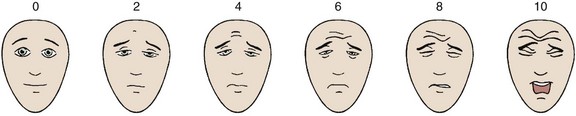
The use of a visual pain scale facilitates consistent documentation. The patient’s assessment of the intensity of the pain using a visual scale (Fig. 29–2) often stimulates a description of the circumstances that exacerbate or alleviate that pain. When making the differential diagnosis, the physician can classify the clinical syndrome into one of three categories: (1) nonmechanical back or leg pain (or both), (2) mechanical back or leg pain (or both), and (3) sciatica.
Warning signs for possible cancer include a history of cancer or constitutional symptoms such as fever or weight loss. Risk factors for infection include a history of recent bacterial infection, intravenous drug use, or an immunocompromised state. Patients with a spine cancer or spine infection often have pain that is not diminished by rest. Warning signs of possible spine fracture are major trauma (e.g., motor vehicle accident, blunt trauma, fall from a height), prolonged corticosteroid use, and osteoporosis. Symptoms suggestive of cauda equina syndrome, which requires urgent surgical consultation, include saddle anesthesia (found in 75% of patients); recent onset of bladder or bowel dysfunction (with urinary retention the most common symptom); and severe or progressive weakness of the lower extremities,3 especially involving both lower extremities.
There are several findings to note when ascertaining psychosocial contributions to nonorganic back pain, as follows4:
Genetics
The “wild card” in the etiology of sciatic pain is genetics. Ala-Kokko5 noted that scientific studies have identified specific versions of the genes encoding collagen, aggrecan, vitamin D receptor, and matrix metalloproteinase-3 that have significant associations with lumbar disc disease. Many other genes may also play a role in disc disease.6–8
Imaging
The Cochrane group performed a meta-analysis of the literature and concluded that there is no correlation between radiographic changes and back pain.9 Contrary to that opinion, researchers in Tokyo reported a study in which they correlated preparticipation spinal radiographs with the incidence of back pain and disability among young football players.10 They followed 171 high school and 742 college football players over a 1-year period. High school players with spondylolysis had a higher incidence of low back pain (79.8%) than players with no radiographic abnormality (37.1%). College players with spondylolysis, disc space narrowing, and spinal instability had a higher incidence of low back pain (80.5%, 59.8%, and 53.5%) than players with normal radiographs (32.1%). College players with spondylolysis had a higher incidence of low back pain than players with disc space narrowing and spinal instability.
Single Photon Emission Computed Tomography
With single photon emission computed tomography (SPECT), gamma camera detectors rotate around the patient in small increments (usually 3- or 6-degree steps), and emission data are obtained from different plane angles. Computer algorithms break the image into pixels, each of which represents an approximately 6-mm area of the planar image. Pixel data are used to render clinically useful volumetric images. SPECT is arguably the best screening examination for significant spinal abnormality versus nonspecific back pain in children and the first examination that should be ordered. Auerbach11 showed that SPECT exceeded MRI or plain radiography in accurately defining spondylolysis in a series of 100 children with significant back pain.
Principles of Treatment and Rehabilitation
Acute Treatment
When pain onset is acute and severe, bed rest may be necessary for 2 or 3 days for initial pain control. A longer period of bed rest quickly becomes counterproductive. The key to recovery is modified activity within a minimal range to start, followed by gentle progression of activity. The sooner the athlete begins a level of tolerated activity, the quicker and more effective is the recovery. Research and experience have dispelled the notion that prolonged absolute rest is beneficial for treatment of back pain.12
Bracing
Bracing is effective in some cases, if used intermittently and primarily as a tool for returning to activity. If used as a “crutch,” extended time in a brace produces atrophy and loss of motion. The Cochrane Collaboration reported a meta-analysis on the use of braces for low back pain in 2004.13 There was moderate evidence that lumbar supports are no more effective for primary prevention than other types of treatment or no intervention. The authors found no data promoting the effectiveness of lumbar supports for secondary prevention. This opinion is consistent with the generally held concept that passive treatment such as bracing should be limited to acute pain relief and that active rehabilitation is an early goal for return to participation in sports and prevention of future injury. Spinal manipulation can provide short-term improvement, but the evidence for longer term relief is inconclusive.14
Rehabilitation
Flexibility
Exercise programs that load the spine throughout the range of motion have poorer outcomes. Greater mobility is associated with poorer outcomes as well. The range of motion of the spine has little predictability for future low back pain. Programs emphasizing trunk stabilization with a neutral spine have had the most success.16–18 These programs emphasize increasing the range of motion of the hips and knees.
Muscle Performance (Strength versus Endurance)
The term strength is defined as the maximum force a muscle can produce during a single exertion to create joint torque. The term endurance refers to the ability to maintain a force for a period of time. Muscle performance includes strength and endurance. The few studies available suggest that endurance has a much greater prophylactic value than strength.19 The emphasis should be placed on endurance and should precede strengthening exercises in a gradual, progressive exercise program (i.e., longer duration, lower effort exercises).
Deep Water Running and Swimming
Walking in a swimming pool is a gentle strengthening exercise for the back. Deep water running is excellent for treating athletes with back pain. The buoyancy of the water helps to unload the spine. Athletes run in the deep end of a swimming pool, normally with the aid of a flotation vest. Water is about 800 times denser than air, so resistance met during water running is greater than when running on land. Deep water running can help to maintain aerobic performance for 6 weeks in trained endurance athletes; sedentary individuals can appreciate significantly increased maximal oxygen uptake. During spine rehabilitation programs, deep water running can be used for maintenance training, but deep water running is not a substitute for conventional training.20–22 Swimming is an excellent exercise for the back, but caution is advised for the novice. The swimming strokes can produce or exacerbate back injury if proper technique is not practiced.
Program Guidelines
The following caveats should be considered when prescribing and monitoring any “return to sport” rehabilitation program23:
Education
Several studies have documented the value of patient education in the treatment of spine problems.29 Education has been shown to be as valuable to the patient’s recovery as physical therapy. In 2004, Frost and colleagues29 measured the effectiveness of routine physical therapy compared with a single assessment session and advice from a physical therapist for patients with low back pain. They used a multicenter, randomized controlled trial in seven British National Health Service physiotherapy departments. These authors concluded that routine physical therapy was no more effective than a single assessment and advice session from a physiotherapist in treating low back pain.
In the physician’s office, handouts are an excellent source of education and can be reference guides for the patient during rehabilitation activities (Table 29–1). Good preprinted handouts are available from multiple sources, such as the Krames (http://www.krames.com/) or the AAOS (http://www.aaos.org/) websites. Personalizing the handouts gives the athlete assurance in his or her provider’s interest and commitment to the rehabilitation plan and confidence in the treatment plan on leaving the office. With the availability of digital radiography, it is inexpensive to give the patient a copy of his or her radiograph to take home. Being educated regarding the nature of the injury and being part of the rehabilitation team, and not merely the subject, motivates the athlete and can bring about speedier and more complete recovery.
TABLE 29–1 Ways to Avoid Overuse Injuries
| 1. Use good technique | An overhand pitch produces less strain than a side-arm pitch |
| 2. If it hurts, don’t do it | “No pain—no gain” is a poor concept. You feel the fatigue of a good workout, but you must recognize the pain of going beyond fatigue to injury |
| 3. Stop when fatigued | Avoid the temptation of an extra repetition. Sprints are best done after a rest |
| 4. Increase duration gradually | It takes time for the body to respond to increased demand and to strengthen |
| 5. Rest for a time after major increases | It is better to alternate 3 hard days with an easy day and then rest for 2 days |
| 6. Quit when you are tired | When you have exhausted the glycogen stored in your muscles, your technique falters, and you are prone to injury |
| 7. Do preventive exercises | Keep your body in balance by stretching to gain full range of motion and loosening contractures |
| 8. Remember your old injuries | When you recall your old injuries, you can work to avoid repeating them |
| 9. Warm up slowly | Use gentle stretching and gradually increasing effort to limber up muscles and deep breathing to stimulate the heart and lungs |
Disorders and Treatment
Low Back Pain in Adolescent Athletes
Lumbar spine pain or low back pain accounts for 5% to 8% of athletic injuries.30 Injuries are often due to poor conditioning of the spine, poor biomechanics, or repetitive stresses placed on the spine by the nature of the sport. Overuse injuries from repeated lumbar hyperextension may be common in children participating in sports such as gymnastics, volleyball, and rowing.
Historical studies show that the correct diagnosis of acute low back pain is established on the first visit only 2% of the time. After 6 weeks, the diagnostic accuracy increases to 15%, and it increases to 30% at 3 months.31 The physician’s initial visit is best used to rule out serious disorders, such as disc herniation or malignant disease. Although less than 1% of back pain complaints are related to serious spine pathology or require emergent treatment, such as neoplasm or cauda equina syndrome, it is important to exclude these conditions and reassure the patient accordingly.
Back pain that follows an acute injury is usually attributed to muscle strain. There is little scientific evidence showing muscle strain as a back pain generator, however, probably because pain produced by an injury cannot be differentiated to the various soft tissues of the back.32 The pain may be localized or diffuse. The patient frequently relates that more stiffness occurred after a night’s sleep. This type of back pain attributed to muscle strain tends to improve with time.
Mechanical backache secondary to poor posture is more common in sedentary children. Athletic children are less likely to report nonspecific back pain than their nonathletic counterparts. Children who do not walk to school and have a poor self-image of their health in general report more back pain. Multivariate analysis showed that the incidence of low back pain in adolescents is inversely related to time spent doing physical activity (e.g., regular walking or bicycling) and directly related to television or computer time.33
Posture and inactivity contribute to low back pain. The intervertebral discs have the highest fluid content in the morning, which influences the pressure generated on spinal tissues during flexion.34 Avoidance of flexion after arising in the morning significantly reduces nonspecific back pain.35
Spondylolysis
Spondylolysis is a stress fracture of the pars interarticularis. It is generally considered to be a low-risk fracture that heals on its own. The fracture occurs most frequently at L5, followed by L4 and L3. Spondylolysis occurs in 5% to 6% of the general population.1 The lesion is usually asymptomatic and appreciated only incidentally on a radiograph. Generally, no single traumatic event causes spondylolysis; rather, repetitive stress produces fatigue defects, and a single event may complete the fracture. These fractures may develop fibrous nonunion or heal in an elongated state.36
The incidence of pars defects is greater in adolescent athletes than in the general population and is a particular clinical problem for this population.37 Sports that require repetitive hyperextension or extension combined with rotation such as gymnastics, wrestling, and weightlifting are more often associated with a stress fracture of the pars interarticularis. White female gymnasts experience a rate of spondylolysis (11%) five times that of the general white female population.38 Certain participants in sports such as diving, weightlifting, wrestling, and gymnastics have disproportionately high rates of spondylolysis. A study of elite Spanish athletes showed the highest rates of spondylolysis in gymnasts and weightlifters followed by throwing athletes and rowers.39 Other reports suggest that a wide variety of sports increase the risk of spondylolysis, including soccer, volleyball, and baseball.40
A major concern for patients with defects in the pars interarticularis is the progressive development of symptomatic spondylolisthesis. The incidence of progressive spondylolisthesis is low (3% to 10%) and mainly occurs during adolescence.41,42 There is no known correlation between active sports participation and either the occurrence or the progression of spondylolisthesis.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree