3.4 The blood
Chapter 3.4a The physiology of the blood
The composition of the blood
In Chapter 2.1c it was explained that the blood is composed of a fluid called plasma and three types of blood cells: the red blood cells (erythrocytes), the white blood cells (leukocytes) and the platelets (thrombocytes).
The plasma
Plasma is quite a thick (viscous) fluid, a property resulting from the proteins dissolved in it. One important function of these proteins is to help keep the watery part of the blood within the blood vessels. As the proteins are too large to move out of the blood vessels by diffusion, they maintain a level of concentration in the blood which contributes to its osmotic pressure (see Chapter 1.1c) (see Q3.4a-2) .
.
The blood cells
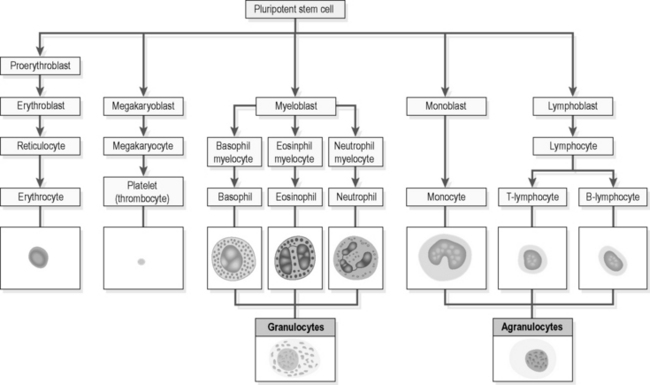
All three types of blood cell originate from the bone marrow. The bone marrow contains a number of immature cells called ‘stem cells’, and it is these that are the starting material for all the different subtypes of blood cells, including all the leukocytes, such as macrophages and mast cells, which leave the blood to perform immune functions in the tissues. Figure 3.4a-I gives a diagrammatic representation of how the stem cell is the ‘great grandparent’ of the red blood cell (the erythrocyte), the platelet and the six different categories of white blood cell (the granulocytes and agranulocytes). It is important to appreciate this process before approaching the study of the condition of leukaemia.
Red blood cells (erythrocytes)
The production of red blood cells is stimulated by the hormone erythropoietin, which is released by the kidneys. The hormone is released when the blood fails to perform its role of oxygenation of tissues in the conditions of anaemia and acute blood loss (see Chapters 3.4c and 3.4d).
Before the maturing red blood cell leaves the bone marrow to enter the blood, the nucleus breaks down. The red blood cell then takes on a disc-like shape, which enables it to be flexible enough to move in large numbers through the finest capillaries. Once in the circulation, the life of the red blood cell is about 120 days, after which it is broken down in the spleen, the liver, and parts of the bone marrow by phagocytic white blood cells. In this process, the iron is removed from the haemoglobin and recycled for further use in the body. The by-product of this process is bilirubin, which is a digested form of haemoglobin, and this is taken up by the liver and excreted into the bile (see Chapter 3.1a) (see Q3.4a-3) .
.
Platelets (thrombocytes)
The platelets, like the red blood cells, are cells without nuclei that originate from the bone marrow. Their function is to work together with the clotting-factor proteins in the plasma to enable an efficient and controlled clotting reaction (see Chapter 2.1c).
White blood cells (leukocytes)
The diverse functions of the white blood cells were introduced in the description of wound healing, inflammation and the immune system in Sections 2.1 and 2.2.
There are two broad groups of white blood cell, which are categorised according to whether or not the cytoplasm contains granules. These are the granulocytes and agranulocytes (see Figure 3.4a-I).
Granulocytes contain granules, which consist of chemicals (enzymes) that are important for the destruction of unwanted foreign matter and in the generation of inflammation. Some of the granulocytes are able to phagocytose (see Chapter 1.1c) small particles such as damaged bacteria. All the granulocytes can move, like an amoeba, out of the blood vessels and into the tissues when their presence is required.
The role of the blood
 Information Box 3.4a-I The functions of the blood: comments from a Chinese medicine perspective
Information Box 3.4a-I The functions of the blood: comments from a Chinese medicine perspective
 Self-test 3.4a The physiology of the blood
Self-test 3.4a The physiology of the blood
2. Why is it important to ensure a good ‘match’ of blood groups before a blood transfusion is given to a patient?
3. How does the function of physical blood relate to the protecting function of Qi?
Answers
2. A mismatch of blood groups is called ‘incompatibility’. Incompatible blood cells tend to clump together and break down. This can be life-threatening if it occurs within the blood vessels of a patient receiving a transfusion.
3. The blood performs a protective role in two main ways. First, it contains clotting factors and platelets, which work together to ensure a healthy clotting response in the case of injury to the blood vessels. This would be related in Chinese medicine partly to the role of Spleen Qi in Holding Blood. (The other contributing factor in Chinese medicine in prevention of bleeding is healthy Yin, which is the energetic foundation to the healthy substance of tissue. Bleeding can be a result of the Empty or Full Heat, which can follow on from Yin Deficiency– see Chapter 2.1c.)
4. All blood cells originate from the immature stem cells, which are situated in the bone marrow. (In newborns this marrow is situated within all the bones, but in adults the blood-forming marrow is largely confined to the vertebrae, the ribs, the skull bones and the ends of the long bones.)
Chapter 3.4b The investigation of the blood
Physical examination
The physical examination of a patient with a suspected disease of the blood involves the stages listed in Table 3.4b-I.
Table 3.4b-I The stages of physical examination of the blood
Blood tests
Biopsy and other tests to visualise the lymph nodes
The two most common forms of cancer that affect the cells of the blood are leukaemia and lymphoma. These diseases are the focus of Chapter 3.4e. In both these conditions the lymph nodes may become engorged with increased numbers of cancerous white blood cells.
 Self-test 3.4b The investigation of the blood
Self-test 3.4b The investigation of the blood
1. You have referred a patient to her GP because you think that her symptoms suggests that she actually may be clinically anaemic. She is pale and tired, but is also very breathless on exertion and experiences frightening palpitations after very little physical effort. These symptoms have responded only a little to your treatment. What can you explain to this patient about the investigations she might have to undergo?
Chapter 3.4c Anaemia
Introduction
In Chapter 3.4d the ways in which a sudden loss of a large quantity of blood might affect the body are explored. Although this condition also reduces the ability of the blood to transport oxygen to the tissues, this is not the same as anaemia. In acute blood loss, the red cells and the concentration of haemoglobin are normal, but the volume of the circulating blood is reduced.
The clinical features of anaemia
The causes of anaemia
The causes of anaemia are conventionally categorised into two groups:
The anaemias resulting from impaired production of red blood cells
Iron-deficiency anaemia
Another group of people who are at risk of iron deficiency are those who cannot absorb iron from the diet because of malabsorption (see Chapter 3.1e).
In all cases of iron-deficiency anaemia, the diagnosis alone is not a sufficient basis on which to start treatment. In all cases, the possibility of malabsorption or excessive blood loss should also be excluded, and this may involve the patient in a referral to a gastroenterologist to exclude chronic bowel disease or bleeding from the bowel. A referral to a gynaecologist may be made for the treatment of heavy menstrual bleeding (see Chapter 5.2c).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 .
.
 .
. Information Box 3.4a-II
Information Box 3.4a-II .
. Information Box 3.4c-I
Information Box 3.4c-I .
. Information Box 3.4c-II
Information Box 3.4c-II
