Approaches to the structures of the ankle and foot usually are straightforward; the bones and joints that are explored commonly are superficial, if not subcutaneous. Apart from technical problems associated with the surgery itself, the most common complication in foot and ankle surgery is poor wound healing. For this reason, it is important to evaluate both the circulation and the sensation of the foot. Ischemic or neuropathic feet heal poorly and are a frequent contraindication to elective surgery. In patients with diabetes, ischemia and neuropathy may coexist; all feet of such patients must be evaluated carefully before any foot surgery is undertaken. Smoking is also a relative contraindication to surgery, especially in cases of open reduction and internal fixation for fractures of the calcaneus.
Wound healing also is affected by the thickness of the skin flaps that are cut; it is important to cut these flaps as thickly as possible and to avoid forceful retraction. Longer incisions require less forceful retraction to achieve identical exposure. As a result, they often are safer than are short incisions. (Remember that skin incisions heal from side to side and not from end to end.)
This chapter is divided into three sections. The first describes approaches to the ankle and the hindpart of the foot, because most provide access to both areas. The anterior approach to the ankle is used for arthrodesis; it offers excellent exposure of the anterior compartment of the ankle joint. The approach to the medial malleolus is a commonly used incision, providing access to the distal tibia in cases of fracture. A more extensive approach to the medial side of the ankle joint also exposes the distal tibia, but involves an osteotomy. The posteromedial approach to the ankle exposes the soft tissues of the area. It is used frequently for soft-tissue operations, including the surgical correction of clubfoot. The posterolateral approach to the ankle joint provides limited access to the back of the joint and the posterior facet of the subtalar joint. The lateral approach to the ankle and hindpart of the foot exposes the ankle and the joints of the hindfoot. The lateral approach to the hindpart of the foot and the posterolateral approach to the talocalcaneal joint are used for surgery on the joints of the posterior part of the foot. The lateral approach to the calcaneus exposes the lateral aspect of the calcaneus, the calcaneocuboid, and subtalar joints. It is mainly used for open reduction and internal fixation of the os calcis.
The second section of this chapter describes approaches to the midportion of the foot, the tarsometatarsal and midtarsal joints and those muscles that attach to them. Surgery in this area is relatively uncommon in general orthopaedic practice; it usually is associated with specific operative procedures designed for single pathologic states. Because these structures are very superficial, the approaches are dealt with mainly pictorially.
The final section comprises three of the most common approaches in surgery of the forepart of the foot. The dorsal and dorsomedial approaches to the metatarsophalangeal joint of the great toe are used in surgery for hallux valgus; the dorsal approach to the metatarsophalangeal joints of the second, third, fourth, and fifth toes provides safe access to these joints; and the approach to the dorsal web spaces can be used for the treatment of several conditions, including Morton’s neuroma. The latter approach also can be used to reach the metatarsophalangeal joint.
The applied anatomy of the foot appears in two sections after this group of approaches. The first section deals with the applied anatomy of the approaches, that is, the applied anatomy of the dorsum of the foot. The second section, an account of the anatomy of the sole of the foot, should provide an understanding of those structures that may be damaged in severe foot trauma or infection.
Anterior Approach to the Ankle
The anterior approach provides excellent exposure of the ankle joint for arthrodesis.1 The decision to use this approach rather than the lateral transfibular approach, the medial transmalleolar approach, or the posterior approach depends on the condition of the skin and the surgical technique to be used. Its other uses include the following:
Drainage of infections in the ankle joint
Removal of loose bodies
Open reduction and internal fixation of comminuted distal tibial fractures (pilon fractures)
Position of the Patient
Place the patient supine on the operating table. Partially exsanguinate the foot either by elevating it for 3 to 5 minutes or by applying a soft rubber bandage loosely to the foot and binding it firmly to the calf. Then, inflate a thigh tourniquet. Partial
exsanguination allows the neurovascular bundle to be identified, because the venous structures will appear blue. Some continuous vascular oozing must be expected, however (Fig. 12-1).
P.625
exsanguination allows the neurovascular bundle to be identified, because the venous structures will appear blue. Some continuous vascular oozing must be expected, however (Fig. 12-1).
Landmarks and Incision
Landmarks
The medial malleolus is the bulbous, subcutaneous, distal end of the medial surface of the tibia.
The lateral malleolus is the subcutaneous distal end of the fibula.
Incision
Make a 15-cm longitudinal incision over the anterior aspect of the ankle joint. Begin about 10 cm proximal to the joint, and extend the incision so that it crosses the joint about midway between the malleoli, ending on the dorsum of the foot. Take great care to cut only the skin; the anterior neurovascular bundle and branches of the superficial peroneal nerve cross the ankle joint very close to the line of the skin incision (Fig. 12-2A). Alternatively, make a 15-cm longitudinal incision with its center overlying the anterior aspect of the medial malleolus (see Fig. 12-2).
Internervous Plane
Although the approach uses no true internervous plane, the extensor hallucis longus and extensor digitorum longus muscles define a clear intermuscular plane. Both muscles are supplied by the deep peroneal nerve, but the plane may be used because both receive their nerve supplies well proximal to the level of the dissection. The plane must be used with great caution, however, because it contains the neurovascular bundle distal to the ankle (see Figs. 12-58 and 12-59).
 |
Figure 12-1 Position for the anterior approach to the ankle. |
Superficial Surgical Dissection
Incise the deep fascia of the leg in line with the skin incision, cutting through the extensor retinaculum (see Fig. 12-2B). Find the plane between the extensor hallucis longus and extensor digitorum longus muscles a few centimeters above the ankle joint, and identify the neurovascular bundle (the anterior tibial artery and the deep peroneal nerve) just medial to the tendon of the extensor hallucis longus (see Fig. 12-2C). Trace the bundle distally until it crosses the front of the ankle joint behind the tendon of the extensor hallucis longus. Retract the tendon of the extensor hallucis longus medially, together with the neurovascular bundle. Retract the tendon of the extensor digitorum longus laterally. The tendons become mobile after the retinaculum has been cut, but the neurovascular bundle adheres to the underlying tissues and requires mobilization (Fig. 12-3A).
Alternatively, in pillion fractures, incise the deep fascia to the medial side of the tibialis anterior tendon (Fig. 12-4), and expose the underlying surface of
the tibia together with the anteromedial ankle joint capsule.
P.626
P.627
P.628
the tibia together with the anteromedial ankle joint capsule.
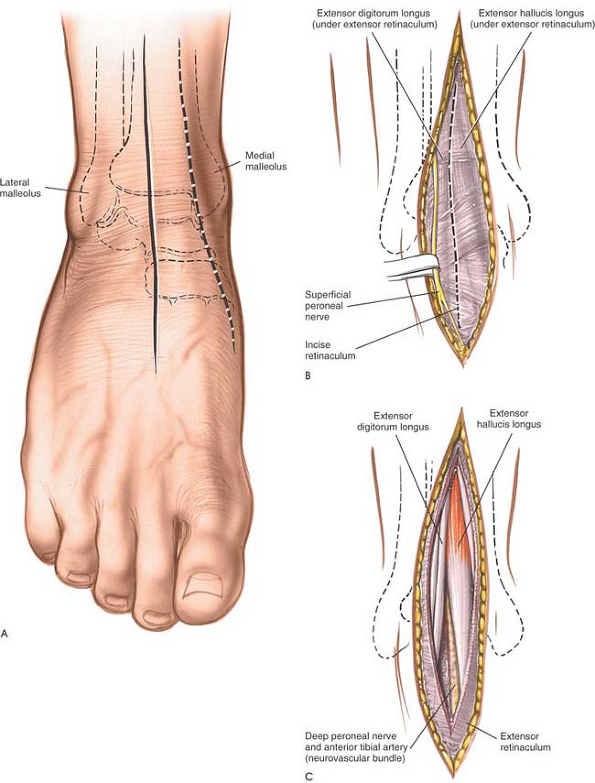 |
Figure 12-2 (A) Make a longitudinal incision over the anterior aspect of the ankle joint. (B) Identify and protect the superficial peroneal nerve. Incise the extensor retinaculum in line with the skin incision. (C) Identify the plane between the extensor hallucis longus and the extensor digitorum longus, and note the neurovascular bundle between them. |
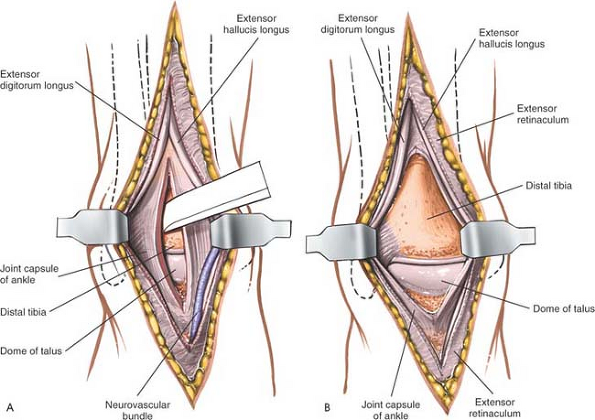 |
Figure 12-3 (A) Retract the tendon of the extensor hallucis longus medially with the neurovascular bundle. Retract the tendon of the extensor digitorum longus laterally. Incise the joint capsule longitudinally. (B) Retract the joint capsule to expose the ankle joint. |
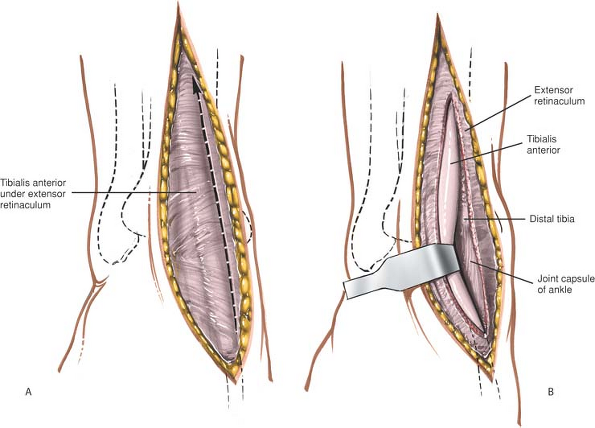 |
Figure 12-4 (A) Alternately, incise the extensor retinaculum on the medial side of the tibialis anterior tendon. (B) Retract the tibialis anterior laterally to expose the anterior surface of the ankle joint. |
Deep Surgical Dissection
For arthrodesis surgery, incise the remaining soft tissues longitudinally to expose the anterior surface of the distal tibia. Continue incising down to the ankle joint, then cut through its anterior capsule. Expose the full width of the ankle joint by detaching the anterior ankle capsule from the tibia or the talus by sharp dissection (see Fig. 12-3). Some periosteal stripping of the distal tibia may be required. Although the periosteal layer usually is thick and easy to define, the plane may be obliterated in cases of infection; the periosteum then must be detached piecemeal by sharp dissection.
If the approach is used in fracture surgery, take great care to preserve as much soft-tissue attachments to bone as possible. Meticulous preoperative planning will allow smaller, precise incisions with consequent reduction in soft-tissue damage.
Dangers
Nerves
Cutaneous branches of the superficial peroneal nerve run close to the line of the skin incision just under the skin. Take care not to cut them during incision of the skin (see Fig. 12-2A).
The deep peroneal nerve and anterior tibial artery (the anterior neurovascular bundle) must be identified and preserved during superficial surgical dissection. They are in greatest danger during the skin incision, because they are superficial and run close to the incision itself (see Figs. 12-58 and 12-59). Above the ankle joint, the neurovascular bundle lies between the tendons of the extensor hallucis longus and tibialis anterior muscles at the joint; the tendon of the extensor hallucis longus crosses the bundle. The plane between the tibialis anterior and the extensor hallucis longus can be used as long as the neurovascular bundle is identified and mobilized so as to preserve it (see Fig. 12-59).
P.629
How to Enlarge the Approach
Extensile Measures
Although this approach does not descend through an internervous plane, on occasion it can be extended proximally to expose the structures in the anterior compartment. To expose the proximal tibia, use the plane between the tibia and the tibialis anterior muscle (see Fig. 12-4). Distal extension to the dorsum of the foot is possible, but rarely, if ever, required (see Fig. 12-59).
Anterior and Posterior Approaches to the Medial Malleolus
The anterior and posterior approaches are used mainly for open reduction and internal fixation of fractures of the medial malleolus.2 The approaches provide excellent visualization of the malleolus.
Position of the Patient
Place the patient supine on the operating table. The natural position of the leg (slight external rotation) exposes the medial malleolus well. Exsanguinate the limb by elevating it for 3 to 5 minutes, then inflate a tourniquet. Standing or sitting at the foot of the table makes it easier to angle drills correctly (Fig. 12-5).
Incisions
Two skin incisions are available.
The anterior incision offers an excellent view of medial malleolar fractures. It also permits inspection of the anteromedial ankle joint and the anteromedial part of the dome of the talus.
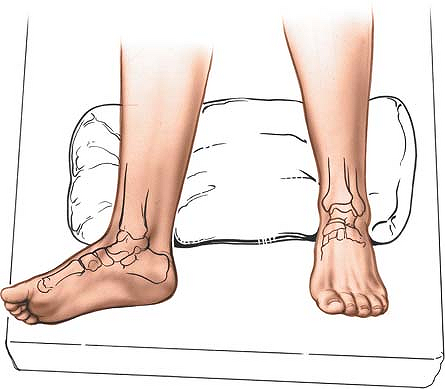
Figure 12-5 Position for the approach to the medial malleolus. The leg falls naturally into a few degrees of external rotation to expose the malleolus.
Make a 10-cm longitudinal curved incision on the medial aspect of the ankle, with its midpoint just anterior to the tip of the medial malleolus. Begin proximally, 5 cm above the malleolus and over the middle of the subcutaneous surface of the tibia. Then, cross the anterior third of the medial malleolus, and curve the incision forward to end some 5 cm anterior and distal to the malleolus. The incision should not cross the most prominent portion of the malleolus (Fig. 12-6).
The posterior incision allows reduction and fixation of medial malleolar fractures and visualization of the posterior margin of the tibia.
Make a 10-cm incision on the medial side of the ankle. Begin 5 cm above the ankle on the posterior border of the tibia, and curve the incision downward, following the posterior border of the
P.630
medial malleolus. Curve the incision forward below the medial malleolus to end 5 cm distal to the malleolus (see Fig. 12-10).
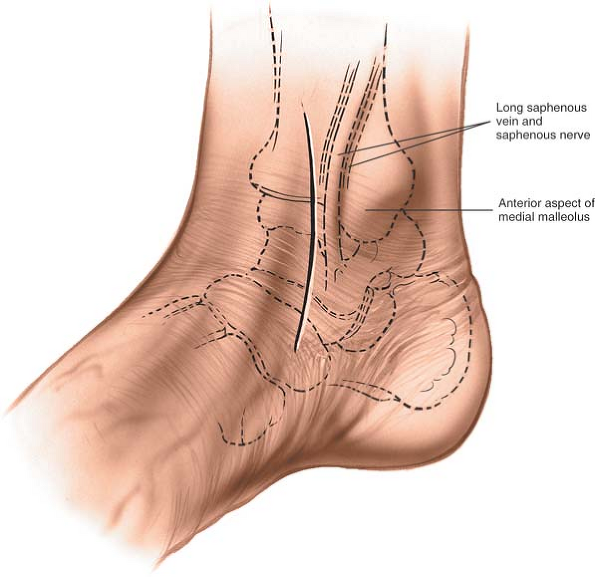 |
Figure 12-6 Keep the incision just anterior to the tip of the medial malleolus. |
Internervous Plane
No true internervous plane exists in this approach, but the approach is safe because the incision cuts down onto subcutaneous bone.
Superficial Surgical Dissection
Anterior Incision
Gently mobilize the skin flaps, taking care to identify and preserve the long saphenous vein, which lies just anterior to the medial malleolus. Accurately locating the skin incision will make it unnecessary to mobilize the skin flaps extensively. Next to the vein runs the saphenous nerve, two branches of which are bound to the vein. Take care not to damage the nerve; damage leads to the formation of a neuroma. Because the nerve is small and not easily identified, the best way to preserve it is to preserve the long saphenous vein, a structure that on its own is of little functional significance (Fig. 12-7).
Posterior Incision
Mobilize the skin flaps. The saphenous nerve is not in danger (see Fig. 12-11).
Deep Surgical Dissection
In cases of fracture, the periosteum already is breached. Protect as many soft-tissue attachments to
the bone fragment as possible to preserve its blood supply.
P.631
the bone fragment as possible to preserve its blood supply.
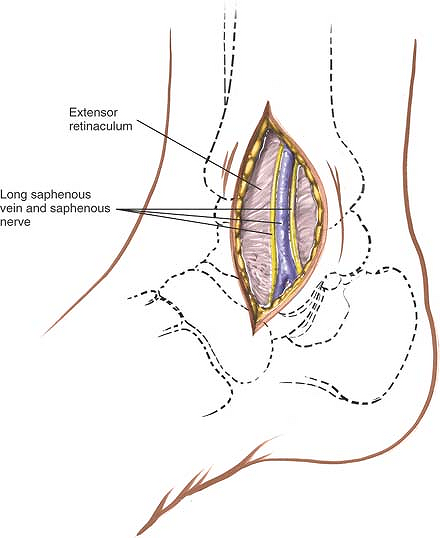 |
Figure 12-7 Widen the skin flaps. Identify the long saphenous vein and the accompanying saphenous nerve. |
Anterior Incision
Incise the remaining coverings of the medial malleolus longitudinally to expose the fracture site. Make a small incision in the anterior capsule of the ankle joint so that the joint surfaces can be seen after the fracture is reduced (Fig. 12-8). This is especially important in vertical fractures of the medial malleolus where impaction at the joint surface frequently occurs. The superficial fibers of the deltoid ligament run anteriorly and distally downward from the medial malleolus; split them so that wires or screws used in internal fixation can be anchored solidly on bone, with the heads of the screws covered by soft tissue (Fig. 12-9; see Fig. 12-56).
Posterior Incision
Incise the retinaculum behind the medial malleolus longitudinally so that it can be repaired (Figs. 12-10 and 12-11). Take care not to cut the tendon of the tibialis posterior muscle, which runs immediately behind the medial malleolus; the incision into the retinaculum permits anterior retraction of the tibialis posterior tendon. Continue the dissection around the back of the malleolus, retracting the other structures that pass behind the medial malleolus posteriorly to reach the posterior margin (or posterior malleolus) of the tibia. The exposure allows reduction of some fractures of that part of the bone.
Note that, although this approach will allow visualization of most fractures using appropriate reduction forceps, the angle of the approach is such that the displaced fragments cannot be fixed internally from this approach. Separate anterior approaches are required to lag any posterior fragments back. It always is advisable to obtain an intraoperative radiograph showing the displaced fragment fixed temporarily with a K-wire before definitive fixation is inserted. Reduction of these fragments is difficult because of limited exposure, and inaccurate reduction may occur. To improve the view of the posterior malleolus, externally rotate the leg still further (Fig. 12-12; see Figs. 12-55 and 12-56).
P.632
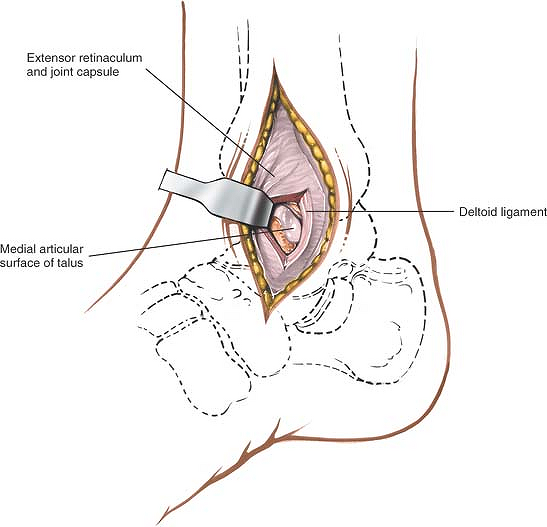 |
Figure 12-8 Make a small incision in the anterior capsule of the ankle joint to see the articulating surface. |
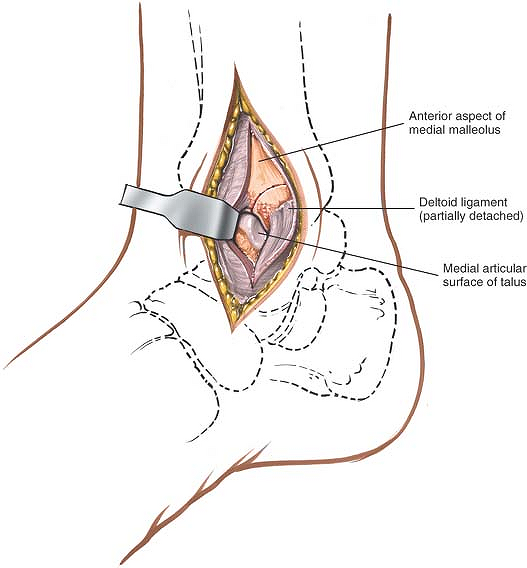 |
Figure 12-9 Split fibers of the deltoid ligament to allow for internal fixation of the fractured malleolus. |
P.633
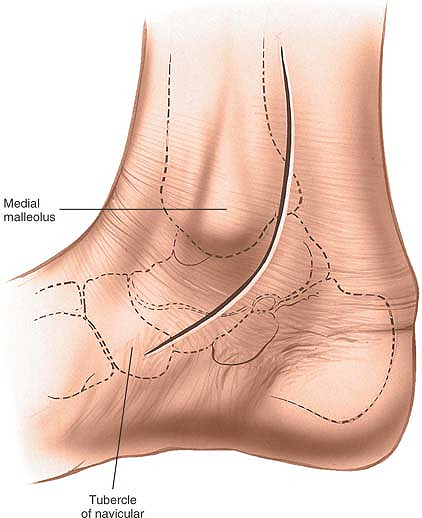 |
Figure 12-10 The posterior incision for the approach to the medial malleolus follows the posterior border of the medial malleolus. |
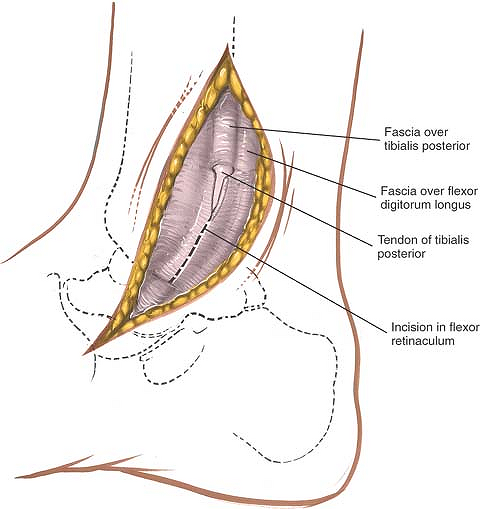 |
Figure 12-11 Retract the skin flaps and begin to incise the retinaculum behind the medial malleolus. |
P.634
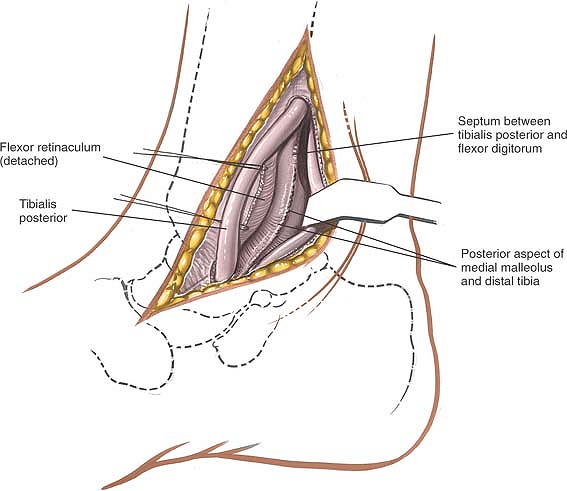 |
Figure 12-12 Anteriorly retract the tibialis posterior. Free up and retract the remaining structures around the back of the malleolus posteriorly to expose the posterior aspect of the medial malleolus. |
Dangers of the Anterior Incision
Nerves
The saphenous nerve, if cut, may form a neuroma and cause numbness over the medial side of the dorsum of the foot. Preserve the nerve by preserving the long saphenous vein.
Vessels
The long saphenous vein is at risk when the anterior skin flaps are mobilized. Preserve it if possible, so that it can be used as a vascular graft in the future (see Fig. 12-54).
Dangers of the Posterior Incision
All the structures that run behind the medial malleolus (the tibialis posterior muscle, the flexor digitorum longus muscle, the posterior tibial artery and vein, the tibial nerve, and the flexor hallucis longus tendon) are in danger if the deep surgical dissection is not carried out close to bone (see Figs. 12-54, 12-55 and 12-56).
Leave as much soft tissue attached to fractured malleolar fragments as possible; complete stripping renders fragments avascular.
How to Enlarge the Approach
Extensile Measures
To enlarge both approaches proximally, continue the incision along the subcutaneous surface of the tibia. Subperiosteal dissection exposes the subcutaneous and lateral surfaces of the tibia along its entire length.
The exposure can be extended distally to expose the deltoid ligaments and the talocalcaneonavicular joint.
P.635
Approach to the Medial Side of the Ankle
The medial approach exposes the medial side of the ankle joint.3 Its uses include the following:
Arthrodesis of the ankle
Excision or fixation of osteochondral fragments from the medial side of the talus
Removal of loose bodies from the ankle joint
Position of the Patient
Place the patient supine on the operating table. Exsanguinate the limb either by elevating it for 5 minutes or by applying a soft rubber bandage firmly; then inflate a tourniquet. The natural external rotation of the leg exposes the medial malleolus. The pelvis ordinarily does not have to be tilted to improve the exposure (see Fig. 12-5).
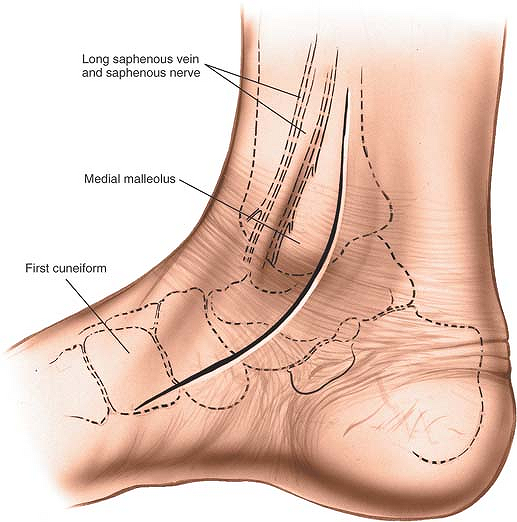 |
Figure 12-13 Make a 10-cm longitudinal incision on the medial aspect of the ankle joint, with its center over the tip of the medial malleolus. Distally, curve the incision forward onto the medial side of the middle part of the foot. |
Landmark and Incision
Landmark
The medial malleolus is the palpable distal end of the tibia.
Incision
Make a 10-cm longitudinal incision on the medial aspect of the ankle joint, centering it on the tip of the medial malleolus. Begin the incision over the medial surface of the tibia. Below the malleolus, curve it forward onto the medial side of the middle part of the foot (Fig. 12-13).
P.636
Internervous Plane
The approach uses no internervous plane. Nevertheless, the surgery is safe because the tibia is subcutaneous and all dissection stays on bone.
Superficial Surgical Dissection
Mobilize the skin flaps, taking care not to damage the long saphenous vein and the saphenous nerve, which run together along the anterior border of the medial malleolus (Fig. 12-14).
Deep Surgical Dissection
To uncover the point at which the medial malleolus joins the shaft of the tibia, make a small longitudinal incision in the anterior part of the joint capsule.
Divide the flexor retinaculum and identify the tendon of the tibialis posterior muscle, which runs immediately behind the medial malleolus, grooving the bone (see Fig. 12-14). Retract the tendon posteriorly to expose the posterior surface of the malleolus (Fig. 12-15A).
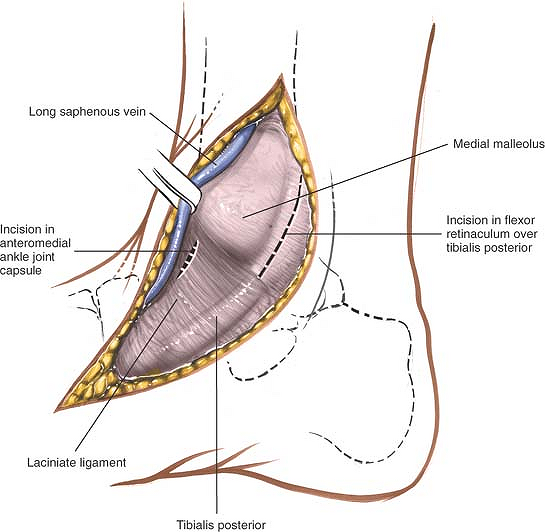 |
Figure 12-14 Carefully retract the skin flaps to protect the long saphenous vein and the accompanying saphenous nerve. Incise the posterior retinaculum, and make a small incision into the anterior joint capsule. |
Score the bone longitudinally to ensure correct alignment of the malleolus during closure. Then, drill and tap the medial malleolus so that it can be reattached (see Fig. 12-15B).
Using an osteotome or oscillating saw, cut through the medial malleolus obliquely from top to bottom; cut laterally at its junction with the shaft of the tibia, checking the position of the cut through the incision in the anterior joint capsule (see Fig. 12-15).
Retract the medial malleolus (with its attached deltoid ligaments) downward and forcibly evert the foot, bringing the dome of the talus and the articulating surface of the tibia into view (Figs. 12-16 and 12-17). Eversion is limited because of the intact fibula.
P.637
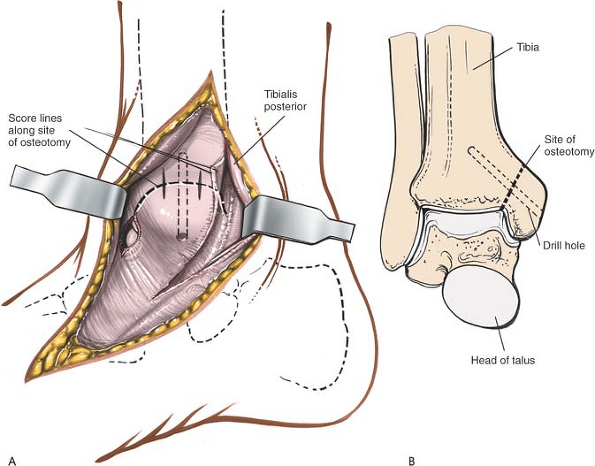 |
Figure 12-15 (A) Retract the tibialis tendon posteriorly. Drill and tap the medial malleolus, and score the potential osteotomy site for future alignment. (B) The line of the osteotomy and the score marks for the reattachment of the medial malleolus. |
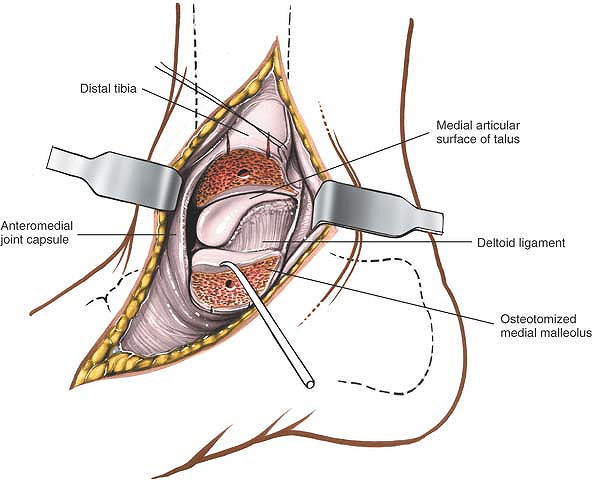 |
Figure 12-16 Retract the osteotomized medial malleolus downward. |
P.638
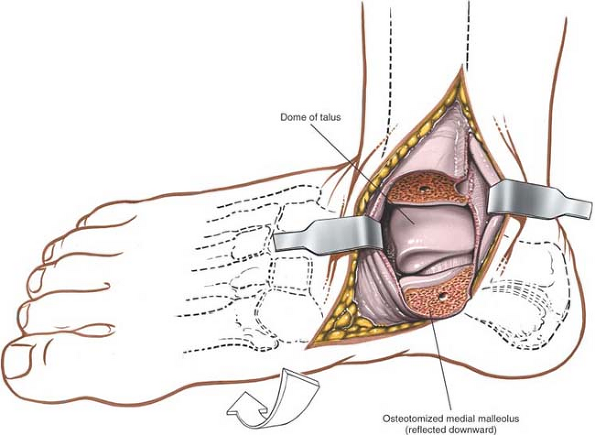 |
Figure 12-17 Forcefully evert the foot to bring the dome of the talus and the anterior surface of the tibia into view. |
Dangers
The saphenous nerve and the long saphenous vein should be preserved as a unit, largely to prevent damage to the saphenous nerve and subsequent neuroma formation.
The tendon of the tibialis posterior muscle is in particular danger during this approach, because it lies immediately posterior to the medial malleolus. Preserve the tendon by releasing and retracting it while performing osteotomy of the malleolus (see Figs. 12-14 and 12-15A). The tendons of the flexor hallucis longus and flexor digitorum longus muscle, together with the posterior neurovascular bundle, lie more posteriorly and laterally. They are in no danger as long as the osteotomy is performed carefully (see Figs. 12-55 and 12-57).
Special Surgical Points
In cases of fracture, the interdigitation of the broken ends of bone prevents rotation between the two fragments when a screw is inserted and tightened. No such interdigitation exists in an osteotomy. Therefore, two Kirschner wires should be used in addition to a screw to prevent rotation when the screw is tightened. After the osteotomy has been stabilized with the screw, the two Kirschner wires can be removed. Tension band fixation also may be used. In any case, align the bones correctly by aligning the score marks made on the bone before the osteotomy.
How to Enlarge the Approach
The approach usually is not enlarged either distally or proximally.
P.639
Posteromedial Approach to the Ankle
The posteromedial approach to the ankle joint is routinely used for exploring the soft tissues that run around the back of the medial malleolus. This approach is used for the release of soft tissue around the medial malleolus in the treatment of clubfoot.
The approach can also be used to allow access to the posterior malleolus of the ankle joint, but gives limited exposure of the fracture site and is technically demanding. For this reason reduction and fixation of posterior malleolar fractures is usually achieved by indirect techniques.4
Position of the Patient
Either of two positions is available for this approach. First, place the patient supine on the operating table. Flex the hip and knee, and place the lateral side of the affected ankle on the anterior surface of the opposite knee. This position will achieve full external rotation of the hip, permitting better exposure of the medial structures of the ankle (Fig. 12-18). Alternatively, place the patient in the lateral position with the affected leg nearest the table. Flex the knee of the opposite limb to get its ankle out of the way.
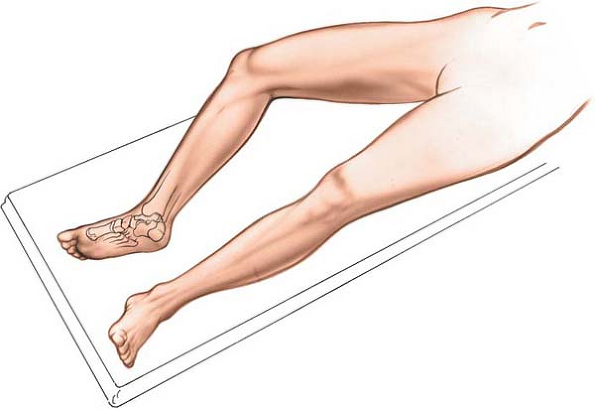 |
Figure 12-18 Place the patient supine on the operating table with the knee and the hip flexed to expose the medial structures of the ankle. |
Exsanguinate the limb by elevating it for 3 to 5 minutes or applying a soft rubber bandage; then inflate a tourniquet.
Landmarks and Incision
Landmarks
The medial malleolus is the bulbous, distal, subcutaneous end of the tibia.
Palpate the Achilles tendon just above the calcaneus.
P.640
Incision
Make an 8- to 10-cm longitudinal incision roughly midway between the medial malleolus and the Achilles tendon (Fig. 12-19).
Superficial Surgical Dissection
Deepen the incision in line with the skin incision to enter the fat that lies between the Achilles tendon and those structures that pass around the back of the medial malleolus. If the Achilles tendon must be lengthened, identify it in the posterior flap of the wound and perform the lengthening now. Identify a fascial plane in the anterior flap that covers the remaining flexor tendons. Incise the fascia longitudinally, well away from the back of the medial malleolus (Figs. 12-20 and 12-21).
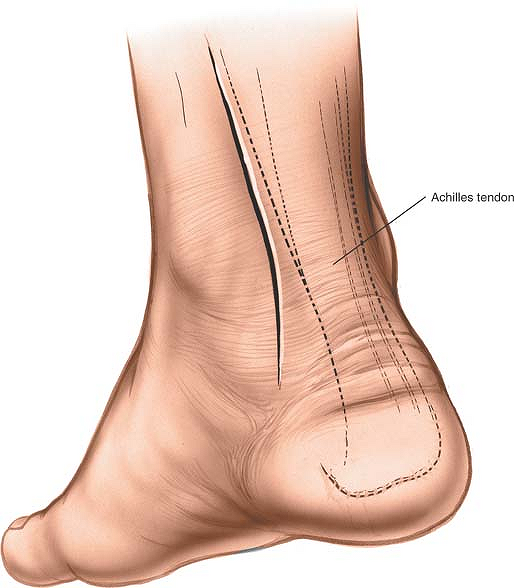 |
Figure 12-19 Make an 8- to 10-cm longitudinal incision roughly between the medial malleolus and the Achilles tendon. |
Deep Surgical Dissection
There are three different ways to approach the back of the ankle joint.
First, identify the flexor hallucis longus, the only muscle that still has muscle fibers at this level (see Fig. 12-21). At its lateral border, develop a plane between it and the peroneal tendons, which lie just lateral to it (Fig. 12-22). Deepen this plane to expose the posterior aspect of the ankle joint by retracting the flexor hallucis longus medially (Fig. 12-23).
Second, identify the flexor hallucis longus and continue the dissection anteriorly toward the back of the medial malleolus. Preserve the neurovascular bundle by mobilizing it gently and retracting it and the flexor hallucis longus laterally to develop a plane between the bundle and the tendon of the flexor digitorum
longus. This approach brings one onto the posterior aspect of the ankle joint rather more medially than does the first approach.
P.641
P.642
longus. This approach brings one onto the posterior aspect of the ankle joint rather more medially than does the first approach.
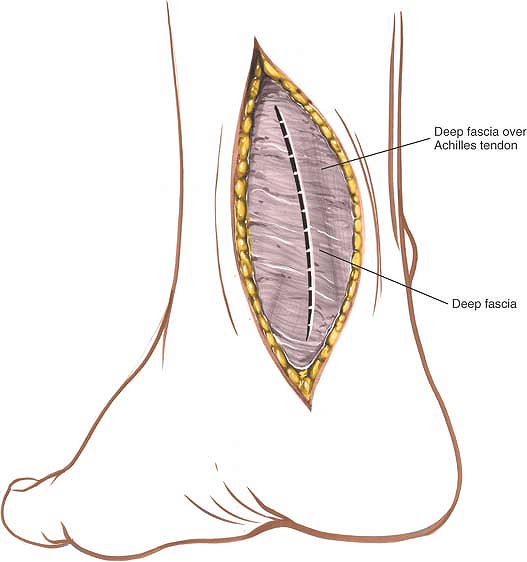 |
Figure 12-20 Incise the deep fascia in line with the skin incision. |
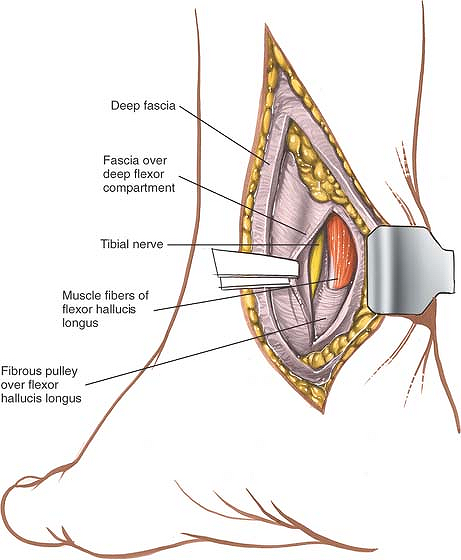 |
Figure 12-21 Retract the Achilles tendon and the retrotendinous fat laterally, exposing the fascia of the deeper flexor compartment. Open the compartment, and identify the muscle fibers of the flexor hallucis longus. |
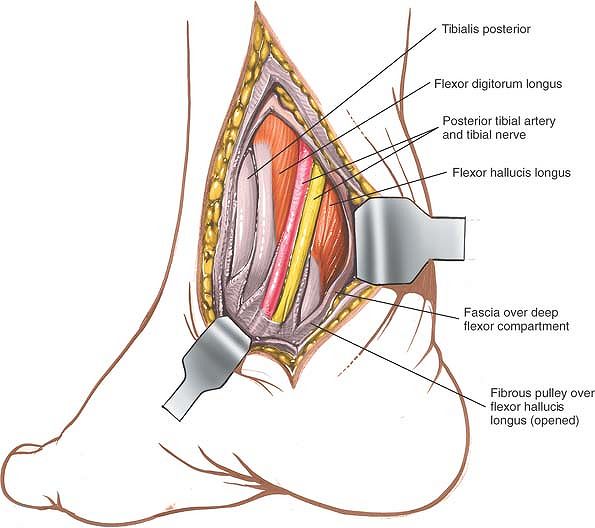 |
Figure 12-22 Identify the posterior tibial artery and tibial nerve. Then, incise the fibro-osseous tunnel over the flexor hallucis longus tendon and the other medial tendons so that the structures can be mobilized and retracted medially. |
Third, when all the tendons that run around the back of the medial malleolus (the tibialis posterior, flexor digitorum longus, and flexor hallucis longus) must be lengthened, the back of the ankle can be approached directly, because the posterior coverings of the tendons must be divided during the lengthening procedure.
For all three methods, complete the approach by incising the joint capsule either longitudinally or transversely.
Dangers
The posterior tibial artery and the tibial nerve (the posterior neurovascular bundle) are vulnerable during the approach. Take care not to apply forceful retraction to the nerve, as this may lead to a neurapraxia. Note that the tibial nerve is surprisingly large in young children and that the tendon of the flexor digitorum longus muscle is extremely small. Take care to identify positively all structures in the area before dividing any muscle tendons (see Figs. 12-54 and 12-55).
How to Enlarge the Approach
Extensile Measures
Extend the incision distally by curving it across the medial border of the ankle, ending over the talonavicular joint. This extension exposes both the talonavicular joint and the master knot of Henry. As is true for all long, curved incisions around the ankle, skin necrosis can result if the skin flaps are not cut thickly or if forcible retraction is applied.
P.643
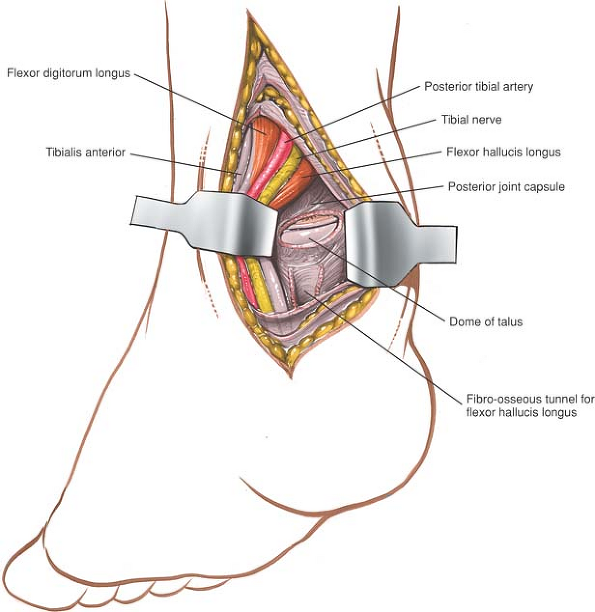 |
Figure 12-23 Retract the posterior structures medially, exposing the posterior portion of the ankle joint. |
Posterolateral Approach to the Ankle
The posterolateral approach is used to treat conditions of the posterior aspect of the distal tibia and ankle joint. It is well suited for open reduction and internal fixation of posterior malleolar fractures. Because the patient is prone, however, it is not the approach of choice if the fibula and medial malleolus have to be fixed at the same time. In such cases, it is better to use either a posteromedial approach or a lateral approach to the fibula, and to approach the posterolateral corner of the tibia through the site of the fractured fibula. Neither of these approaches provides such good visualization of the bone as does the posterolateral approach to the ankle, but both allow other surgical procedures to be carried out without changing the position of the patient on the table halfway through the operation. Its other uses include the following:
Excision of sequestra
Removal of benign tumors
Arthrodesis of the posterior facet of the subtalar joint
P.644
Posterior capsulotomy and syndesmotomy of the ankle
Elongation of tendons
Position of the Patient
Place the patient prone on the operating table. As always, when the prone position is being used, longitudinal pads should be placed under the pelvis and chest so that the center portion of the chest and abdomen are free to move with respiration. A sandbag should be placed under the ankle so that it can be extended during the operation. Next, exsanguinate the limb by elevating it for 3 to 5 minutes or applying a soft rubber bandage; then inflate a tourniquet (Fig. 12-24).
Landmarks and Incision
Landmarks
The lateral malleolus is the subcutaneous distal end of the fibula.
The Achilles tendon is easily palpable as it approaches its insertion into the calcaneus.
 |
Figure 12-24 Position of the patient for the posterolateral approach to the ankle joint. |
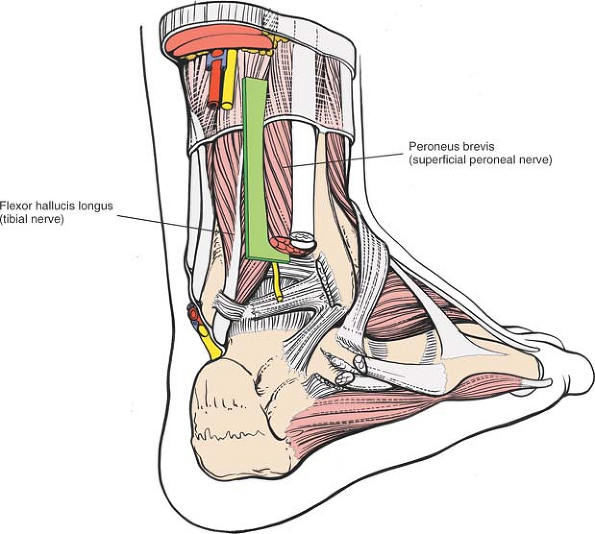 |
Figure 12-25 The internervous plane lies between the peroneus brevis (which is supplied by the superficial peroneal nerve) and the flexor hallucis longus (which is supplied by the tibial nerve). |
P.645
Incision
Make a 10-cm longitudinal incision halfway between the posterior border of the lateral malleolus and the lateral border of the Achilles tendon. Begin the incision at the level of the tip of the fibula and extend it proximally (Fig. 12-26).
Internervous Plane
The internervous plane lies between the peroneus brevis muscle (which is supplied by the superficial peroneal nerve) and the flexor hallucis longus muscle (which is supplied by the tibial nerve; Fig. 12-25).
Superficial Surgical Dissection
Mobilize the skin flaps. The short saphenous vein and sural nerves run just behind the lateral malleolus; they should be well anterior to the incision. Incise the deep fascia of the leg in line with the skin incision, and identify the two peroneal tendons as they pass down the leg and around the back of the lateral malleolus (Fig. 12-27). The tendon of the peroneus brevis muscle is anterior to that of the peroneus longus muscle at the level of the ankle joint and, therefore, is closer to the lateral malleolus. Note that the peroneus brevis is muscular almost down to the ankle, whereas the peroneus longus is tendinous in the distal third of the leg (see Figs. 12-64 and 12-65).
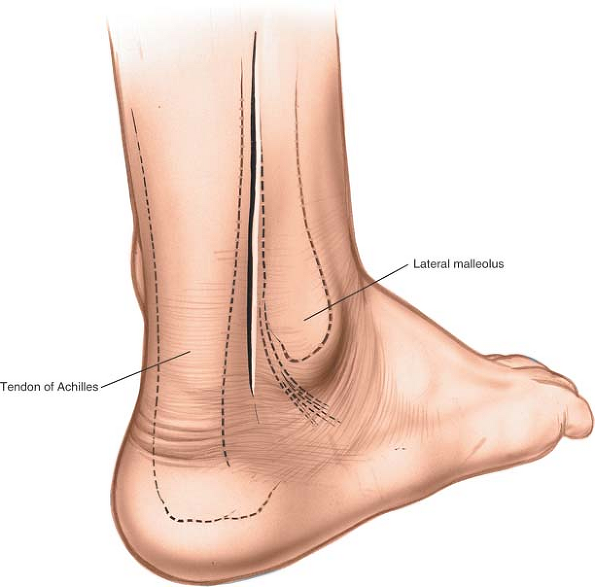 |
Figure 12-26 Make a 10-cm longitudinal incision halfway between the posterior border of the lateral malleolus and the lateral border of the Achilles tendon. |
Incise the peroneal retinaculum to release the tendons, and retract the muscles laterally and anteriorly to expose the flexor hallucis longus muscle (Fig. 12-28). The flexor hallucis longus is the most lateral of the deep flexor muscles of the calf. It is the only one that is still muscular at this level (see Fig. 12-65).
P.646
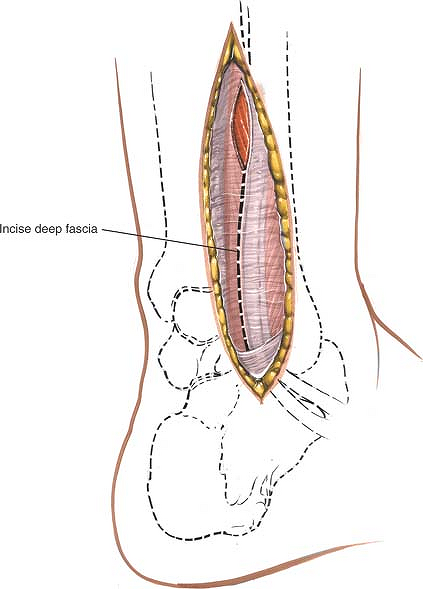 |
Figure 12-27 Mobilize the skin flaps. Incise the deep fascia of the leg in line with the skin incision. Identify the two peroneal tendons as they pass around the ankle. |
P.647
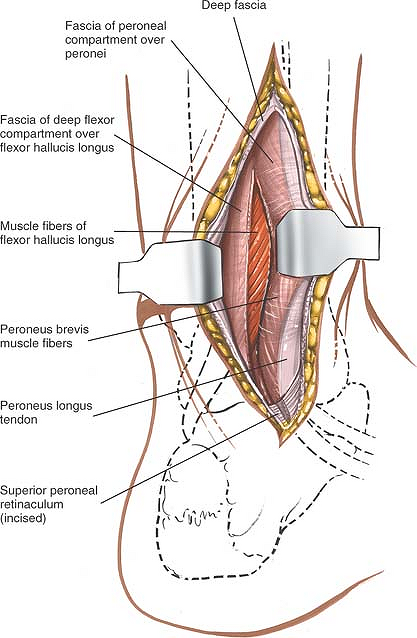 |
Figure 12-28 Incise the peroneal retinaculum to release the tendons. Retract them laterally and anteriorly. Incise the fascia over the flexor hallucis longus to expose its muscle fibers. |
P.648
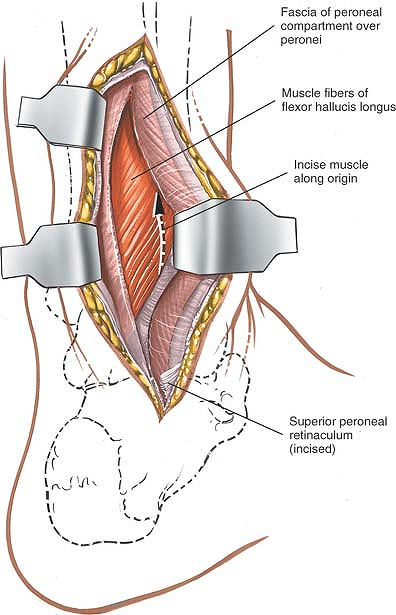 |
Figure 12-29 Make a longitudinal incision through the lateral fibers of the flexor hallucis longus as they arise from the fibula. |
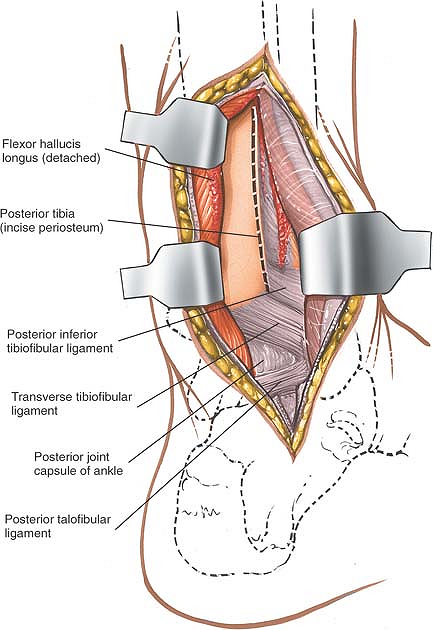 |
Figure 12-30 Retract the flexor hallucis longus medially to reveal the periosteum covering the posterior aspect of the tibia. |
P.649
Deep Surgical Dissection
To enhance the exposure, make a longitudinal incision through the lateral fibers of the flexor hallucis longus muscle as they arise from the fibula (Fig. 12-29). Retract the flexor hallucis longus medially to reveal the periosteum over the posterior aspect of the tibia (Fig. 12-30). If the distal tibia must be reached, develop an epi-periosteal plane between the periosteum covering the tibia and the overlying soft tissues. To enter the ankle joint, follow the posterior aspect of the tibia down to the posterior ankle joint capsule and incise it transversely.
Dangers
The short saphenous vein and the sural nerve run close together. They should be preserved as a unit, largely to prevent the formation of a painful neuroma (see Fig. 12-64).
How to Enlarge the Approach
Extensile Measures
To enlarge the approach proximally, extend the skin incision superiorly and identify the plane between the lateral head of the gastrocnemius muscle and the peroneus muscles. Develop this plane down to the soleus muscle; retract it medially with the gastrocnemius. Next, reflect the flexor hallucis longus muscle medially, detaching it from its origin on the fibula. Continue the dissection medially across the interosseous membrane to the posterior aspect of the tibia (see Posterolateral Approach to the Tibia in Chapter 11).
Lateral Approach to the Lateral Malleolus
The approach to the lateral malleolus is used primarily for open reduction and internal fixation of lateral malleolar fractures. It also offers access to the posterolateral aspect of the tibia.
Position of the Patient
Place the patient supine on the operating table with a sandbag under the buttock of the affected limb. The sandbag causes the limb to rotate medially, bringing the lateral malleolus forward and making it easier to reach (Fig. 12-31). Tilt the table away from you to further increase the internal rotation of the limb. Operating with the patient on his or her side also provides excellent access to the distal fibula, but the medial malleolus cannot be reached unless the patient’s position is changed, something that is necessary in the fixation of bimalleolar fractures (Fig. 12-32). Exsanguinate the limb by elevating it for 3 to 5 minutes, then inflate a tourniquet.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








