7

The Acromioclavicular and Sternoclavicular Joints
This chapter discusses the examination of the acromioclavicular (AC) and sternoclavicular (SC) joints. Although AC joint conditions are more commonly seen in patients, conditions of the SC joint continue to be some of the more vexing problems in the shoulder to treat. Even though they are infrequent, injuries to both ends of the clavicle at the AC joint and SC joint can occur, so the examiner should be able to see the SC joint as part of the AC examination.
Examination of the Acromioclavicular Joint
AC Examination
The AC joint may be one of the few joints in the shoulder where an examiner can get his or her hands on the joint and where the tests upon examination are fairly accurate and reliable. Although this makes the joint easier to examine and to treat, there are some AC joint conditions that require further study before definitive statements can be made about the accuracy and reliability of examination for those entities. The most common conditions of the AC joint include idiopathic osteoarthritis, posttraumatic arthritis, AC separations, and osteolysis.1 Most of these can be reliably diagnosed with a history, physical examination, and radiographs. In patients with a history of trauma, AC separations and posttraumatic arthritis are the most common. In patients with insidious onset of pain without trauma, the most frequent diagnosis will be idiopathic osteoarthritis or osteolysis.
Osteolysis is a condition of increased bone turnover due to stress at the distal clavicle, but its presentation is similar to primary or secondary osteoarthritis. It is most common in weight lifters and active individuals who perform exercises known to stress the AC joint and to cause pain, specifically push-ups, bench presses, and dips. Other conditions that can cause this condition are hyperparathyroidism, rheumatoid arthritis, and other forms of systemic arthritis.2–7
The examination of the AC joint should involve comparing both sides; this may be one of the most helpful tools in making the diagnosis (Fig. 7-1). Asymmetry of the AC joints can be a helpful finding upon examination but does not necessarily correlate with symptoms in all cases. It is important to do a complete examination because other conditions may mimic AC joint problems.
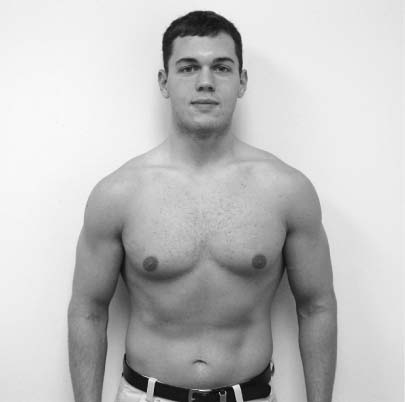
FIGURE 7-1 The examination of the acromioclavicular (AC) joint, comparing both sides.
It is also possible that AC joint problems can mimic other shoulder pathologies. Patients with severe AC joint pain may have significant inflammation and pain of the whole shoulder region, with or without loss of range of motion and function.8 Patients may be unable to lift their arms over shoulder level, and they may report dysfunction with other activities.
AC joint disease can also mimic other shoulder pathologies by presenting with a pain distribution similar to rotator cuff problems and by producing pain with maneuvers traditionally felt to be diagnostic of impingement. In our study of patients with isolated AC joint problems, 57% had a positive Neer sign, 47% a positive Hawkins sign, 50% a painful arc, 24% a positive Speed’s test, and 35% a drop arm sign.9 In their study of patients with isolated AC joint problems, Maritz and Oosthuizen10 found that 59% had a painful arc sign, 86% a positive Speed’s test, 57% neck tenderness, and 91% a positive Jobe’s test. (see chapter 4)
There are three major entities that can mimic AC joint problems. The first is cervical spine disease, which frequently radiates down the trapezius into the superior shoulder. The second entity, which can have symptoms similar to AC joint problems, is a superior labrum anterior and posterior (SLAP) lesion. Berg and Ciullo11 reported on SLAP lesions that were missed and discovered only after the distal clavicle excision did not relieve the patient’s pain. The third most common entity that can mimic AC joint problems is rotator cuff disease.
In addition, more than one diagnosis can occur at one time, and the most common condition seen to coexist with AC joint problems is rotator cuff disease.1,12–16 In our cohort of 737 patients who underwent surgery between 1992 and 2001, there were 42 cases of isolated distal clavicle resection, but there were 105 cases of distal clavicle excision with acromioplasties and rotator cuff repairs. This indicates that AC joint problems frequently coexist with rotator cuff problems, which require surgery. When operating on younger patients with AC joint problems, Berg and Ciullo16 recommended arthroscopy of the shoulder to avoid missing other entities such as SLAP lesions that might be masked or coexist with AC joint pathologies. We agree with these recommendations and routinely perform diagnostic arthroscopy of the shoulder in patients who are having what seem to be isolated AC joint problems.
The other reason to do a complete examination is to verify the findings of AC joint pathology seen in imaging modalities and to determine if they are part of the clinical presentation. In our practice, many patients present to the office with plain radiographs or magnetic resonance imaging (MRI) scans that demonstrate arthritis of the AC joint. Patients often confuse AC arthritis with glenohumeral arthritis and seek consultation with the orthopedic surgeon because they have arthritis in their shoulder. Patients and practitioners often do not realize that AC joint arthritis is nearly a normal condition with aging of the individual.
The incidence of asymptomatic idiopathic arthritis of the AC has been shown to increase linearly with age. This has been verified in studies using plain radiographs, MRIs, and cadaveric studies.17,18 Cadaveric studies show degenerative changes of the AC joint in the fourth decade, with increasing frequency with each successive decade.19 Petersson20 performed dissections of the acromioclavicular joint in 85 cadavers (168 AC joints) of all ages. He found increased severity of degenerative changes with age and suggested that this was a consequence of regression of the acromioclavicular disk. Bonsell et al18 studied radiographs of 84 asymptomatic individuals between 40 and 83 years of age and found significant relationship between specific radiological degenerative changes and age. In this study, 45% individuals overall had radiological evidence of AC degenerative disease.
Recent MRI studies demonstrate that degenerative changes begin in the AC joint in the third decade and can affect up to 93% of shoulders over the fourth decade.17 A vast majority of these degenerative acromioclavicular joints are not symptomatic, and they do not warrant treatment. In a study on 50 shoulders by Stein et al,17 the prevalence of AC joint arthritis with MRI in asymptomatic patients was 68% in the 30-and-under age group and 93% in the over-30 age group. In one study of asymptomatic volunteers, MRI findings indicative of AC joint arthritis were present in 75% of shoulders.21
Observation
One of the most helpful hints for the presence of AC joint problems is to compare the two shoulders for asymmetry of the AC joints. There is a wide range of normal variation in the degree of prominence of the AC joint in patients; this is probably because of the high degree of asymptomatic arthritis in the AC joint. Asymmetry is not diagnostic of any one condition, but it should direct the examiner to inquire about pathology or pain in the AC joint.
Other causes of swelling of the AC joint region can be due to trauma, tumors, infections, or synovial cysts. Malignant tumors of the distal clavicle are unusual, but the authors are reminded of a case of a metastatic breast cancer to the distal clavicle in their practice, which was the cause of swelling and pain. The diagnosis was made by a history of increasing pain and increasing swelling near the AC joint with no trauma in a patient with a history of breast cancer. Plain radiographs revealed the tumor and imminent pathological fracture. Although this presentation is uncommon, it demonstrates that the AC joint region is not immune to conditions that can affect other joints.
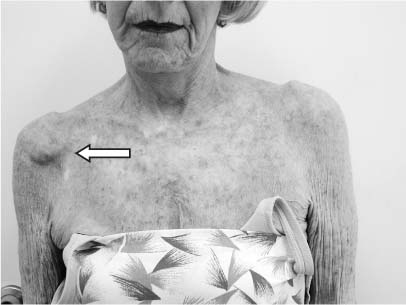
FIGURE 7-2 Synovial cyst near the AC joint (arrow).
Sepsis of the AC joint can produce symptoms of pain and swelling, but usually the patient has or eventually develops other symptoms of a septic arthritis such as a fever, redness, and warmth. It can be due to hematogenous seeding of the joint, but this is more common in immunosuppressed individuals, such as those patients who are leukopenic due to chemotherapeutic agents or human immunodeficiency virus (HIV) disease. Sepsis can be iatrogenic after AC joint injections or after surgical procedures.
Synovial cysts can appear near the AC joint, and the patient typically will have a painless swelling that is insidious. These cysts sometimes regress in size, and they can be quite small or very large (Figs. 7-2, 7-3). They can be associated with isolated AC joint arthritis, rotator cuff tears, rheumatoid arthritis, or other conditions about the shoulder.12,22,23 Some authors have suggested transilluminating the cysts with a light to establish the diagnosis, because cysts should transilluminate, and more solid masses will not. This is not diagnostic, however, and in patients where the diagnosis is uncertain, either aspiration of the cyst or MRI of the shoulder and AC joint may confirm the diagnosis.

FIGURE 7-3 Clinical presentation of a synovial cyst over the AC joint.
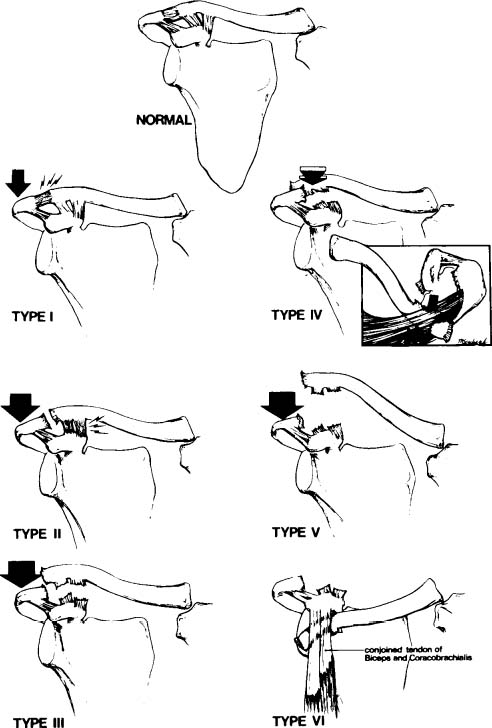
Ecchymosis, swelling, and pain after trauma are common in this region, and the differential diagnosis is quite long. The major differential diagnosis is between fractures and AC separations. AC separations have been classified as three types by Allman24 and modified by Rockwood25 as six types (Fig. 7-4). Almost each of these types can be mimicked by a distal clavicle fracture, so observation and examination should be accompanied by radiographic evaluation. Grade I injuries typically have only swelling and no deformity (Fig. 7-5). Grade II injuries usually have swelling and a mild deformity, but this diagnosis must be confirmed with radiographs that demonstrate a step-off between the AC joint and the acromion (Fig. 7-6).
Grade III injuries have displacement of the clavicle superiorly with a characteristic deformity (Fig. 7-7). Sometimes this displacement can be difficult to evaluate acutely due to swelling and in patients who are large or heavy. In addition, patients often present hunched over due to pain with the involved extremity lower than the other side. This often makes the diagnosis uncertain, and other injuries should be ruled out. Grade IV injuries are displacement of the clavicle posteriorly into the trapezius fascia. These injuries are less common, but axillary radiographs can confirm the displacement (Fig. 7-8). Grade V injuries are where the clavicle displaces significantly superiorly and may tent the skin (Fig. 7-9). They are difficult to distinguish from grade III lesions acutely and warrant further evaluation once the pain and swelling have diminished. Radiographs can help with determining the degree of displacement, but often the clinical appearance is the more important determinant of treatment. Last, grade VI lesions are subcoracoid dislocations of the clavicle, and these are extremely rare. A review of the literature demonstrates only a handful of cases of grade VI lesions, but these patients may present with a wide variety of symptoms due to compression of the brachial plexus by the displaced clavicle. Patients with trauma, deformity of the shoulder, and neurovascular findings should be carefully and thoroughly evaluated for these lesions.
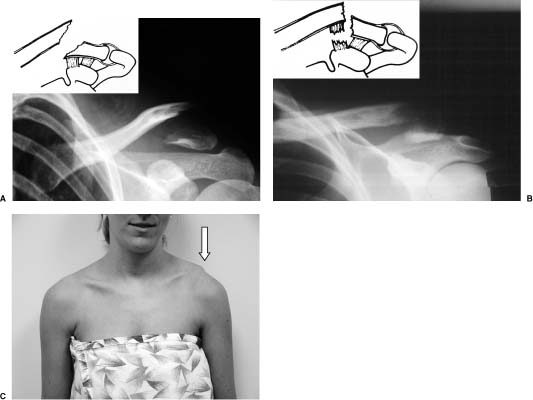
Fractures of the distal clavicle can mimic or coexist with AC joint problems. As a result, radiographs are indicated in most cases of deformity of the AC joint. Distal clavicle fractures are classified according the location and displacement (Figs. 7-10, 7-11, 7-12). Type I fractures can appear like grade I or II AC separations. Type II clavicle fractures can appear like grade III or IV AC separation. The clinical appearance of type II A and type II B distal clavicle is the same, and they cannot be distinguished by physical examination. Type III distal clavicle fracture typically appears like grade II or III AC separation (Fig. 7-12).
FIGURE 7-4 Types of AC joint separation. (Adapted with permission from Rockwood CA Jr. Subluxations and dislocations about the shoulder: injuries to acromioclavicular separations. In: Rockwood CA Jr, Green DP, eds. Fractures. Philadelphia: JB Lippincott; 1984:860–910.)

FIGURE 7-5 Clinical presentation of a grade I AC separation (right side) can be very subtle.
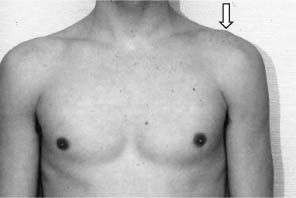
FIGURE 7-6 Clinical presentation of a grade II AC joint separation (arrow).
FIGURE 7-7 Clinical and radiological presentation of a grade III AC joint separation (arrow).

FIGURE 7-8 Clinical presentation of a grade IV AC joint separation.
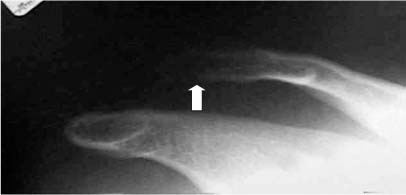
FIGURE 7-9 Radiograph of a grade V AC joint separation showing elevation of the distal clavicle (arrow).

FIGURE 7-10 An artist’s depiction (A) and a radiographic appearance (B) of a type I distal clavicle fracture.
FIGURE 7-11 Type IIa (A) and IIb (B) distal clavicle fractures can appear similar on clinical examination (C). (Adapted with permission from Craig EV Fractures of the clavicle. In: Rockwood CA Jr, Matsen FA, eds. The Shoulder, Vol. 1. Philadelphia: WB Saunders; 1998:428–482.)
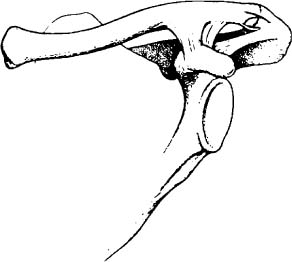
FIGURE 7-12 Type III distal clavicle fracture where the fracture enters the AC joint. (Adapted with permission from Craig EV. Fractures of the Clavicle. In: Rockwood CA Jr, Matsen FA, eds. The Shoulder, Vol. 1. Philadelphia: WB Saunders; 1998:428–482.)
Pain Distribution and Local Tenderness
One of the major hints that a patient may have AC joint pathology is the distribution of pain. Whereas rotator cuff symptoms typically radiate into the deltoid and proximal arm, the pain of the AC joint is usually located over the joint and radiates into the trapezius (Fig. 7-13). Afflictions of the AC joint should be considered in the differential diagnosis of trapezius and neck pain.
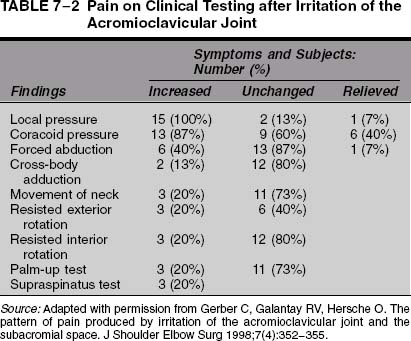
Gerber et al26 performed a simple but elegant study to demonstrate the difference in pain distributions by injecting saline selectively into either the AC joint or the subacromial space. The injection into the AC joint produced pain into the trapezius in 80% of patients (12 of 15), and injections into the subacromial space produced pain into the deltoid region in 100% (8 of 8 patients). Gerber and colleagues concluded that the pain pattern alone is a reliable observation to support the diagnosis of AC joint pathology; however, they noted that patients reported pain in a variety of locations after irritation of the AC joint (Table 7-1). This indicates that other pain patterns can be present due to AC joint irritation. One limitation of their study was that the pain distribution of AC joint pathology could not be compared with that of SLAP lesions, which can mimic AC joint problems.11,27
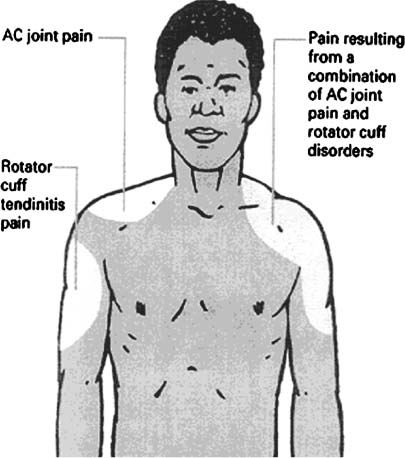
FIGURE 7-13 Pathology of the AC joint and rotator cuff creates different pain patterns. (Adapted with permission from McFarland EG, Hobbs WR. The active shoulder: AC joint pain and injury. Your Patient & Fitness 1998;12 (4):23–27.)
| Local pain | 15 (100%) |
| Supraspinatus fossa | 12 (80%) |
| Upper trapezius muscle | 12 (80%) |
| Lateral clavicle | 12 (80%) |
| Anterolateral deltoid region | 9 (60%) |
| Medial aspect of upper arm | 4 (27%) |
| Thumb | 4 (27%) |
| Sternocleidomastoid muscle | 3 (20%) |
| Posterolateral acromion | 2 (13%) |
| Radial forearm | 1 (7%) |
| Infraspinatus fossa | 0 |
| Triceps region | 0 |
| Posterior deltoid region | 0 |
Source: Adapted with permission from Gerber C, Galantay RV, Hersche O. The pattern of pain produced by irritation of the acromioclavicular joint and the subacromial space. J Shoulder Elbow Surg 1998;7(4):352–355.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree