6

Examination of the Biceps Tendon and Superior Labrum Anterior and Posterior (SLAP) Lesions
Examination of the long head of the biceps tendon and of its attachments to the superior glenoid demonstrates many of the challenges that are part of the shoulder in general. Although there have been significant advances in our knowledge of the anatomy and pathologies of the biceps tendon, it is still unknown what causes pain in the region of the biceps tendon in the anterior shoulder.
Codman in 19341 argued with Meyer2,3 whether the pain into the deltoid and front of the shoulder was due to lesions of the biceps tendon or to rotator cuff tears. Since that time several areas of controversy still exist: What is the real function of the biceps tendon in the shoulder? Does biceps tendonitis occur as an isolated diagnosis? Does biceps instability really exist, and how do you make the diagnosis? Do lesions of the biceps attachment (superior labrum anterior and posterior, or SLAP lesions) have a distinctive clinical picture that explains the pathophysiology of those lesions and the findings upon examination?
Anatomy of the Biceps Tendon
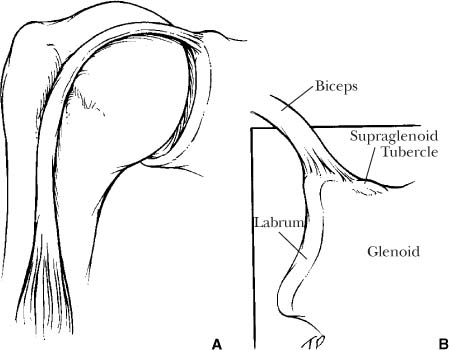
The biceps muscle is made of two heads, which run from the humerus to the scapula by very different routes (Fig. 6-1). The short head is more medial and becomes confluent with the coracobrachialis muscle. These two muscles form a tendon that attaches to the coracoid. The long head of the biceps muscle superiorly turns into a thin tendon about the thickness of a pencil. In the proximal humerus this tendon runs behind or posterior to the pectoralis major attachment to the humerus. At the upper end of the pectoralis major insertions, it is covered by a thin fascia for 1 to 2 cm before it enters the intertubercular groove. The roof over the intertubercular groove is a thick fascia, which helps to stabilize the tendon in the groove.
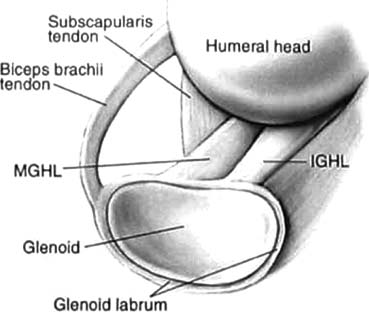
The biceps tendon then enters the glenohumeral joint and attaches to the superior aspect of the glenoid. The structures around where the tendon enters the shoulder are called the “pulley” system. The structures that contribute to this pulley system which stabilize the tendon include the superior glenohumeral ligament, the coracoacromial ligament, the upper portion of the subscapularis tendon, and some fibers of the supraspinatus tendon.4
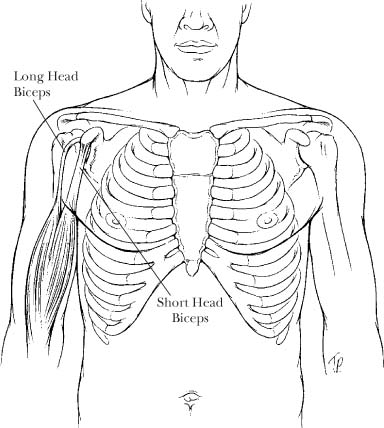
FIGURE 6-1 The biceps muscle consists of a long head that attaches to the superior glenoid and a short head that attaches to the coracoid process.
FIGURE 6-2 The long head of the biceps tendon has an attachment to the superior glenoid tubercle and also to the superior labrum. (A = coronal view; B = coronal cut through glenoid)
Biceps Attachment Anatomy
The biceps tendon attaches to the superior glenoid by direct tendon attachment to the superior glenoid tubercle. It also contributes portions to the labrum anteriorly and posteriorly at the top of the joint (Fig. 6-2). The labrum in the superior half of the joint typically attaches to the edge of the glenoid via strong collagen fibers In the upper half of the glenoid, it is very common for there to be no attachment of the labrum to the articular cartilage5 (Fig. 6-3). This gives the labrum an appearance in some ways like a meniscus of the knee. Below the level of the equator the labrum typically has a transition zone to the articular cartilage, so that a probe cannot be placed between it and the articular surface (Fig. 6-4).
The attachment of the biceps to the labrum can be highly variable. Vangsness et al5 dissected 105 fresh-frozen shoulders from cadavers and found that there were four different types of attachment of the biceps to the superior glenoid (Fig. 6-5). The most common type of attachment (37%) was where the fibers of the biceps tendon as they attached to the labrum were split equally between the anterior labrum and the posterior labrum (type III). The second most common type (33%) was where most of the attachment of the biceps to the superior labrum was directed to the posterosuperior labrum (type II). The third most common type (22%) was where the biceps attachment was to the posterior labrum with no contribution to the anterior labrum. The least common type was where most of the biceps attachment was to the anterior labrum, and there was only a small attachment to the posterior labrum. The authors speculated that these different patterns may influence the predisposition of the labrum to be injured in some patients.
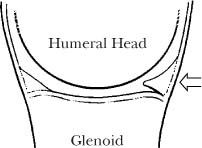
FIGURE 6-3 The labrum above the level of the equator of the glenoid frequently does not attach to the articular cartilage.
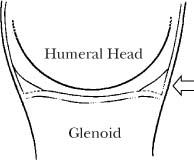
FIGURE 6-4 The labrum below the level of the equator of the glenoid typically attaches directly to the articular cartilage.
This variability of the labrum attachment to the superior glenoid is also complicated by a large variability in the attachment of the labrum to the glenoid rim in the anterior and superior portion of the glenoid. In most instances the labrum is present and attaches to the superior rim (Fig. 6-6). The second most common variation is the presence of a sublabral hole under the labrum (Fig. 6-7). The third most common type is where the labrum does not attach to the superior glenoid at all (Fig. 6-8).
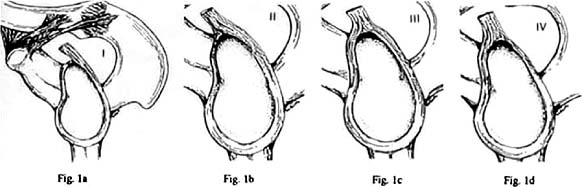
FIGURE 6-5 The superior labrum can have different configurations where the biceps attaches. (Adapted with permission from Vangsness CT Jr, et al. The origin of the long head of the biceps from the scapula and glenoid labrum: an anatomical study of 100 shoulders. J Bone Joint Surg Br 1994; 76(6):951–954.)
FIGURE 6-6 The most common pattern of the anterior and superior labrum attachment to the superior glenoid. (Adapted with permission from Rao AG, Kim TK, Chronopoulos E, McFarland EG. Anatomical variants in the anteroposterior aspect of the glenoid labrum: a statistical analysis of seventy-three cases. J Bone Joint Surg Am 2003;85(4):653–659.)
The other structure that is highly variable in the anterior shoulder is the middle glenohumeral ligament (MGHL). It can be flat and wide like a sheet (Fig. 6-6), or it can be cordlike on the upper edge (Fig. 6-9). In a minority of instances, the MGHL is a thick cord without any bandlike portion. When this cordlike type of MGHL is seen without a labrum attached to the glenoid rim in the anterior and superior quadrant, it is known as a Buford complex6,7 (Fig. 6-10) and is observed to occur in 1.5% of patients with SLAP lesions. There is some evidence that shoulders with a combination of a cordlike MGHL and labrum detachments in the anterior and superior quadrant of the glenoid may predispose the shoulder to further damage to the structures in that area.7
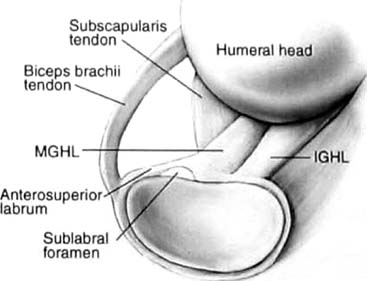
FIGURE 6-7 The labrum may not attach to the anterior and superior labrum, so that there is a “sublabral hole” between the labrum and the glenoid rim. This is a normal variation. (Adapted with permission from Rao AG, Kim TK, Chronopoulos E, McFarland EG. Anatomical variants in the anteroposterior aspect of the glenoid labrum: a statistical analysis of seventy-three cases. J Bone Joint Surg Am 2003;85(4):653–659.)
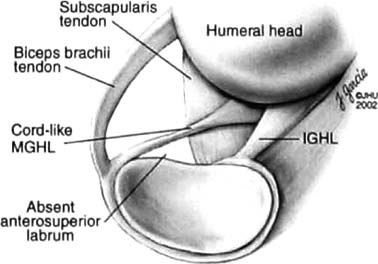
FIGURE 6-8 Another normal variation of the labrum in the anterior and superior glenoid is the lack of attachment of the labrum to the glenoid in this area. (Adapted with permission from Rao AG, Kim TK, Chronopoulos E, McFarland EG. Anatomical variants in the anteroposterior aspect of the glenoid labrum: a statistical analysis of seventy-three cases. J Bone Joint Surg Am 2003;85(4):653–659.)
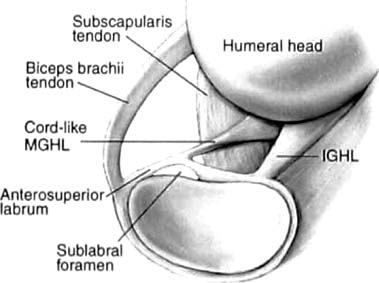
FIGURE 6-9 The middle glenohumeral ligament can be either flat or cordlike. (Adapted with permission from Rao AG, Kim TK, Chronopoulos E, McFarland EG. Anatomical variants in the anteroposterior aspect of the glenoid labrum: a statistical analysis of seventy-three cases. J Bone Joint Surg Am 2003; 85(4): 653–659.)
FIGURE 6-10 An arthroscopic view with the arthroscope in a posterior portal showing a Buford complex where the superior labrum does not attach to the superior glenoid.
Biceps Tendon Tears
The biceps tendon is one of the most commonly torn tendons in the body, and the incidence of spontaneous, complete tearing of the tendon increases linearly with age.8 When the tendon tears, there is typically a “pop” sound, with an immediate bulging of the tendon in the middle of the arm (Fig. 6-11). Biceps tendon tears can occur at any age, but the incidence increases sharply over the age of 50 years.8 The exact etiology of what causes biceps tendons to tear is not known. There are several theories, including senescence of the tendon, wear of the tendon on the acromion as part of impingement disease, and wear of the tendon in the bicipital groove.
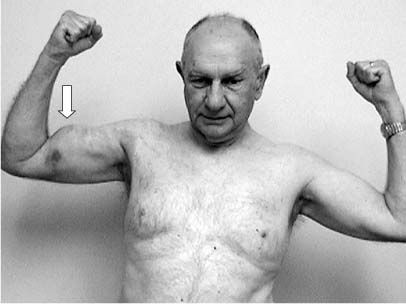
FIGURE 6-11 An acute tear of the long head of the biceps tendon produces a characteristic lump in the arm, sometimes with ecchymosis.
The most common location of biceps tendon tears is near or at the level of the bicipital groove where it enters into the joint. Neer9,10 reported that the majority of biceps tendon ruptures occurred at the superior edge of the bicipital groove. He thought that the rupture of the long head of the biceps may be due to subacromial impingement. Hitchcock and Bechtol,11 Meyer,2,3 and others have noted that biceps ruptures tend to occur at the level of the bicipital groove, but they suggested that the geometry of the bone of the bicipital groove was responsible for biceps tendon wear and rupture.
Biceps tendon tears have also been reported in conjunction with tears of the labrum attachment to the superior glenoid. The association of biceps tears intra-articularly with detachments of the labrum was first noted by Snyder et al.12 Burkhart and Fox13 reported two cases of traumatic rupture of the long head of the biceps from its insertion on the glenoid labrum, which was associated with glenoid chondromalacia and a superior labrum detachment.
SLAP Lesions
The biceps complex where it attaches to the superior glenoid can be the site of tears and detachments of the biceps. This damage can take the form of just fraying, or the biceps tendon can be pulled off its attachments to the superior glenoid tubercle. Likewise, it can be torn with the superior labrum, so that the labrum is torn off the anterior and superior glenoid rims. These lesions were labeled superior labrum anterior and posterior (SLAP) lesions by Snyder et al.12
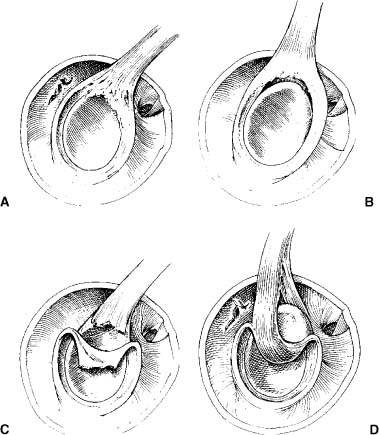
The identification of superior labrum pathology was first described arthroscopically by Andrews et al in 1985.14 The first classification of SLAP lesions was published by Snyder et al12 in 1990 and included four types (Fig. 6-12). Type I was just fraying of the superior labrum with no detachment. A type II lesion was a detachment of the biceps anchor and of the attachments of the anterior and superior labrum from the superior glenoid rim. Type III was a bucket handle tear of the superior labrum without detachment of the biceps anchor to bone. A type IV lesion was a type III with extension of the tear up into the biceps tendon itself.
Further types of SLAP lesions were described by Maffet et al15 and included other labral pathologies (Fig. 6-13). A type V SLAP was a type II labrum tear with extension anteriorly and inferiorly to include a Bankart lesion, a type VI was a flap tear of the superior labrum, and a type VII was a type II with an extension into the middle glenohumeral ligament. Maffet et al reported that these subtypes comprised 38% of all the SLAP lesions seen in their 52 patients with SLAP lesions.
FIGURE 6-12 (A-D) Snyder’s classification of SLAP lesions. (Adapted with permission from Snyder SJ, et al. SLAP lesions of the shoulder. Arthroscopy 1990;6(4):274-279.)
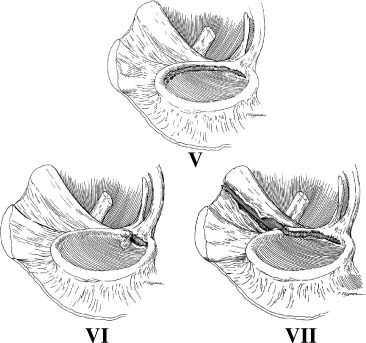
FIGURE 6-13 Maffet et al expanded the classification of SLAP lesions to include several more types of labrum pathology. (Adapted with permission from Maffet MW, Gartsman GM, Moseley B. Superior labrum-biceps tendon complex lesions of the shoulder. Am J Sports Med 1995;23(1):93–98.)
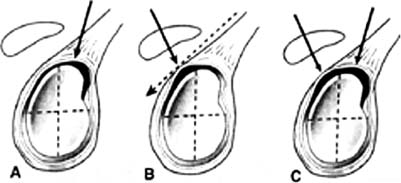
FIGURE 6-14 (A-C) Morgan et al divided type II SLAP lesions into three subtypes. In all three subtypes the attachment to the superior glenoid tubercle is torn. (Adapted with permission from Morgan CD, Burkhart SS, Palmeri M, Gillespie M. Type II SLAP lesions: three subtypes and their relationships to superior instability and rotators cuff tears. Arthroscopy 1998;14(6):553–565.)
Type II SLAP lesions have been further subdivided into three subtypes by Morgan et al16 (Fig. 6-14). All of these variants include an avulsion of the biceps anchor from the superior glenoid tubercle. According to their study, there is a type II anterior that has the posterior portion of the labrum attachment intact, a type II posterior where the anterior labral attachment is intact, and a type III combined where the labrum is detached completely, including the anterior and posterior portions. Morgan et al postulated that these three variations had different pathophysiologies, different clinical presentations, and different findings upon physical examination.
Function of the Biceps Tendon
The function of the long head of the biceps tendon is the first controversy that hinders examination and treatment of biceps tendon disorders. The long head of the biceps tendon has been proposed to serve three functions. The first is a static function, where it acts as a spacer between the humeral head and the acromion, a function that it shares with the supraspinatus tendon.11,17 Evidence for this is sparse because there is only one study that has suggested that this distance diminishes 2 to 6 mm after isolated biceps tenodesis.18 In that study, seven patients with isolated biceps problems underwent biceps tenodesis. Serial radiographs at minimum of 24 months of follow-up revealed that the space diminished with the arm in various degrees of elevation but not with the arm at the side. Although other factors might have explained these changes, such as coexisting pathology in the rotator cuff, the authors concluded that it is possible that the biceps tendon does serve as a static or dynamic spacer with arm elevation.
The second postulated function of the biceps tendon is as a static constraint to anterior and posterior shoulder translations, especially with the arm elevated as when throwing a baseball. The biceps tendon undergoes relatively little motion with internal rotation of the arm, whereas it undergoes its greatest excursion with external rotation. With the arm in external rotation, it is in maximum contact with the bicipital groove, and in this position it acts as a static depressor of the humeral head.19,20
Itoi et al21 demonstrated that with production of a Bankart lesion in a cadaver model, the biceps tendon acted as an anterior stabilizer when the arm was in abduction and external rotation. A study by Pradhan et al22 using strain gauges in the superior labrum found that the strain was highest when the arm was in maximum external rotation, which is similar to that in the late cocking position of throwing. With the arm in this position, the strain was higher in the posterior portion of the labrum than in the anterior portion.
This function of the biceps tendon as a stabilizer of the shoulder in abduction and external rotation has been seen as a possible reason that athletes in overhead sports develop lesions of the biceps anchor. One theory is that the tension on the biceps tendon is increased when it is in abduction and external rotation and also when the biceps muscle is pulling on the tendon. This chronic tension on the biceps with throwing or overhead activities eventually pulls the tendon attachment from the superior glenoid.
Another theory is that the biceps tendon has a dynamic function at the shoulder, so that when the biceps muscle contracts, it stabilizes the humeral head. This theory was first promulgated by Andrews et al,14 who noticed using electromyograms (EMGs) that there was high biceps muscle activity after ball release. They also noted that when viewing the biceps tendon in the shoulder joint during arthroscopy, if they stimulated the biceps muscle to contract with an electrode, the biceps tendon could be seen to tug the superior labrum complex from the bone.
Since that time there have been two major criticisms of the theory that tension produced by biceps muscle contraction contributes to the development of SLAP lesions. First, studies using EMG and high-speed videography have suggested that the main function of the increased biceps muscle activity just after ball release is to control elbow flexion and not to control shoulder motion.23 The only way the increased biceps muscle activity in the follow-through phase of throwing might contribute to biceps lesions is by increasing tension in the whole biceps muscle tendon unit.
Secondly, several studies have demonstrated that biceps muscle activity is minimal when the shoulder was moved in a variety of motions; this suggests that the proximal biceps tendon may not be affected by biceps muscle activity. Both Levy et al23 and Yamaguchi et al24 performed experiments where the elbow was immobilized in flexion with a splint; with movement of the arm, the only motions were allowed at the shoulder. There was little to no biceps activity demonstrated for almost all of the shoulder motions, and because the elbow was held so that the muscle could not bend the elbow, these studies suggest that the major dynamic function of the biceps tendon is at the elbow and not the shoulder.
The last argument against a dynamic effect of the biceps muscle and its tendon at the shoulder is the long lever arm between the muscle and the tendon insertion in the joint. The tendon distance between the muscle and its attachment at the superior glenoid is quite long, and significant muscle action would be necessary to place enough tension on the tendon to produce either motion or stability.
The Biceps Tendon and Shoulder Instability
There are two diverging theories about the relationship of superior labrum pathology to shoulder laxity and instability. The first theory is that of Jobe et al,25 who suggest that throwing creates lengthening of the inferior glenohumeral ligament. This lengthening produces a form of occult instability, which then leads to pain, partial rotator cuff tears, and superior labrum tears. As the arm becomes more unstable, there is increasing tension in the biceps tendon and anchor at the time of ball release. Studies26 have demonstrated that the highest force seen by the shoulder in throwing are a 1000-N force at ball release; this force is essentially pulling the arm away from the body. The theory is that over time the biceps anchor eventually sustains a tension overload, and the biceps is pulled off the superior glenoid.
This theory is supported by a biomechanical study by Bey et al,27 which shows that inferior subluxations of the shoulder joint could produce SLAP lesions. The theory was that as the shoulder subluxates inferiorly, the head puts tension on the biceps tendon. This theory is supported by the finding that the more severe varieties of SLAP lesions, specifically types III and IV, are found almost exclusively in patients who have experienced an anterior shoulder dislocation or who are overhead athletes with potential subclinical instability.28
The second interpretation of the relationship between SLAP lesions and shoulder laxity has been the reverse of that suggested by Jobe et al. Several surgeons have suggested that the SLAP lesion comes first and that the SLAP lesion then results in increased laxity and a form of occult instability. In other words, the Jobe theory suggests that instability creates SLAP lesions, and the diverging theory suggests that the SLAP lesion comes first and results in a unique form of instability.29–31
Morgan et al16 have suggested that superior labral lesions may result in this form of instability, which they say is a “superior instability” pattern. They suggest that when the arm is in abduction and external rotation, as in the cocking phase of throwing, the biceps tendon is rotated superiorly on the glenoid, and there is tension on the biceps anchor. This twisting motion of the biceps tendon stresses the labrum attachments, and eventually the labrum begins to “peel” off the posterosuperior glenoid (Fig. 6-15).
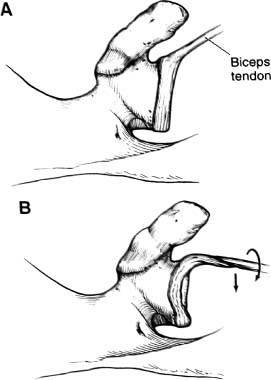
FIGURE 6-15 (A,B) The peel-back mechanism of SLAP lesions is due to torsional forces upon the labrum. (Adapted with permission from Morgan CD, Burkhart SS, Palmeri M, Gillespie M. Type II SLAP lesions: three subtypes and their relationships to superior instability and rotators cuff tears. Arthroscopy 1998;14(6):553–565.)
It is also possible that injury to the biceps attachment is due to a combination of anteroinferior glenohumeral instability and tension in the biceps by other mechanisms. Morgan et al16 suggested that a torsional mechanism may be the primary cause of the superior labrum failure, or that it may be a secondary contributing cause once the lesion has been initiated by the “tension overload” mechanism as described by Andrews et al.14 Andrews et al supported the idea that superior labrum lesions are due to a combination of twisting and pulling, which they compared to “pulling weeds.” Once the superior labrum is torn, this results in the increased shoulder laxity observed in athletes upon examination and at the time of surgery.
This increased laxity due to superior labrum lesions has been called a form of “superior” instability by some authors and an “anterior pseudolaxity” by others.30 The more likely explanation is that these labrum abnormalities do effect glenohumeral translations in many subtle ways, including in an anteroinferior and possibly an anterosuperior direction; however, the exact mechanism continues to be elusive, and this inexact understanding of the mechanism producing SLAP lesions affects our understanding of the physical examination and our treatment strategies.
The first evidence that the superior labrum may affect the biomechanics of the shoulder comes from a clinical study that found that some presumably normal labrum variants are associated with more superior labrum fraying and labrum detachments.7 The exact mechanism by which those variations lead to pathologies could not be determined because it was an observational study.
Schulz et al32 studied the effect of the presence of a sublabral hole in the superior labrum upon the density of the glenoid bone in cadavers. They found no difference in the bone densities and concluded that simple sublabral holes alone did not affect stability of the shoulder. This conclusion is supported by a study by Pagnani et al,33 who evaluated the effect of an isolated release of the anterosuperior labrum upon translations of the shoulder. They found that there was no effect on translations until a larger release of the labrum attachments was performed. This release had to include the attachments of the middle glenohumeral ligament anteriorly, the biceps attachment to the superior glenoid tubercle, and the superior labrum attachments anteriorly and posteriorly.
Biomechanical studies, however, do support the possibility that superior labrum pathology contributes to anterior, inferior, and possibly superior laxities. Pagnani el al33 demonstrated that once a complete lesion of the biceps anchor was produced (i.e., a type II SLAP lesion), there were significantly increased translations of the shoulder in an inferior-superior direction and in an anteroposterior direction. McMahon et al34 found similar results when a superior labrum detachment was created in a cadaver model, and the effects on shoulder joint translations were studied with a robotic device. They found significant increases in anterior and inferior translations with either a partial or full detachment of the superior labrum complex, which indicates that the superior labrum complex may contribute to shoulder instability in some way.
Burkhart and Morgan35 have suggested clinically that when a SLAP lesion is repaired arthroscopically, the laxity of the shoulder is decreased. The drive-through sign, which is performed by trying to push the arthroscope through the joint under arthroscopy, has been demonstrated to be an indication of laxity of the shoulder and not of overt instability.36 Burkhart and Morgan35 found that the drive-through sign was eliminated in patients who underwent a SLAP repair, supporting the idea that the superior labrum complex influences anterior and inferior shoulder laxities.
It may be that the biceps tendon attachment is important for shoulder function only in certain circumstances, such as when performing overhead sports or strenuous activities. Isolated rupture of the biceps tendon is clinically tolerated in many individuals. Surgical procedures on the biceps tendon would also question that the biceps tendon serves a significant role in the function of the shoulder. There have been many who suggest that the biceps is a vestigial structure that can be released from its attachments to the superior glenoid (called a tenotomy) or tenodesed to the proximal humerus (where the tendon is sutured to the bone to maintain tension in the biceps muscle) with impunity.17,37
Both biceps tenotomy and biceps tenodesis have been found to produce few to no deficits in shoulder function postoperatively. Gill et al.38 in 2001 reported the clinical follow-up of 30 patients who underwent arthroscopic release of the biceps for bicipital tenosynovitis, dislocation, or partial rupture of the biceps tendon. Most (90%) of their patients returned to the same level of sports with minimal or no pain. Osbahr et al.39 in 2002 compared the clinical results of 80 patients who underwent biceps tenotomy and 80 patients who underwent biceps tenodesis. They did not find a significant difference between the two groups in terms of anterior shoulder pain, muscle spasm, or cosmetic deformity. These studies would suggest that one could live and function quite well without the long head of the biceps tendon attached to the superior glenoid.
Several studies would suggest, however, that biceps tenotomy or tenodesis may be associated with some dysfunction of the biceps muscle, particularly in its superior portion. A study by West et al.40 found that 25% of their patients with tenotomy of the long head of the biceps tendon continued to have cramping and pain in the superior biceps muscle region. This compared with patients in their study who had tenodesis who did not experience either of these complications (0%). Neither group complained of shoulder weakness or dysfunction, whereas the tenotomy group was less likely to return to their previous level of activity. Despite that observation, shoulder scores between the two groups did not differ, which suggests that the shoulder can function perfectly well without the long head of the biceps.
None of these studies have demonstrated that removing the biceps tendon from the shoulder joint affects its function or its stability. No study has shown that a biceps tenotomy or tenodesis produces shoulder instability. It may be that the biceps tendon functions as a stabilizer in only select patient groups; however, it is safe to assume that, like most other structures in the body, the long head of the biceps tendon is there for a reason, and that resection should not be performed without some concern.
The Biceps Tendon and Shoulder Pain
Another quandary involves the relationship of the biceps tendon pathology to pain in the shoulder. The biceps tendon as a source of pain has been supported by the observation that the pain that precedes a biceps tendon rupture is typically gone once the tendon tears.41 This concept is supported by the fact that biceps tenolysis can be an effective procedure for the relief of pain in the anterior shoulder that is believed to be due to biceps tendon pathology.42
Some physicians have suggested, however, that anterior shoulder pain due to isolated biceps tendinitis is not common. In 1972 Neer43 commented that because the biceps tendon was so commonly involved in impingement (rotator cuff) disease, “we now consider it unwise to operate upon the biceps tendon alone without having considered the possibility of a concomitant element of subacromial impingement” (p. 49). Especially in patients older than 40 years of age, Neer suggested that any biceps surgery should be accompanied by an anterior acromioplasty and coracoacromial ligament release. He felt that impingement of the rotator cuff and the biceps tendon upon the acromion was the cause of the biceps pain and pathology and that they typically occurred together.43,44
It has been suggested by some physicians that pain in the region of the biceps tendon is actually referred pain from rotator cuff pathology or other sources.23,43 Becker and Cofield45 found that of patients who had an isolated biceps tenodesis, 15% required further surgery, usually an acromioplasty, to eliminate their pain.
Some of the uncertainty about the diagnosis of isolated biceps pathology relates to the lack of a distinctive pain pattern associated with biceps tendon pathology. There is little doubt that lesions of the biceps tendon are capable of producing pain. A study by Soifer et al46 of the distribution of nerve pain fibers in the shoulder was highest in the bursa, followed by the biceps tendon and the rotator cuff. It has been supposed by most physicians that the pain produced by biceps pathology radiates down the front of the shoulder in the region of the biceps tendon (Fig. 6-16), but this has never been convincingly established by any injection studies or other methods.41
Part of the challenge is that pain of rotator cuff pathology typically radiates into the anterior and lateral shoulder just like biceps pathology. Also, signs upon examination of impingement that involve internal rotation (i.e., Kennedy-Hawkins sign) of the arm can produce pain in the deltoid and anterior aspect of the shoulder, so this pattern of pain could be due either to the biceps or to the rotator cuff in patients who have both problems. What exactly causes the pain in either the Kennedy-Hawkins sign or with the coracoid impingement sign has not been determined, and the degree that biceps pathology contributes to the pain typical of impingement has not been established.
There are several cadaveric studies suggesting that arm positions that have been felt to compress the rotator cuff may also cause impingement of the biceps tendon. Valadie et al47 in a study of cadaver shoulders found that with a Kennedy-Hawkins impingement sign (flexion and internal rotation), the biceps tendon made contact with the coracoacromial ligament in two of four specimens. Another study by Burns and Whipple48 using cadaver dissections also suggested that the biceps made contact with the coracoacromial ligament with the arm in flexion and internal rotation.
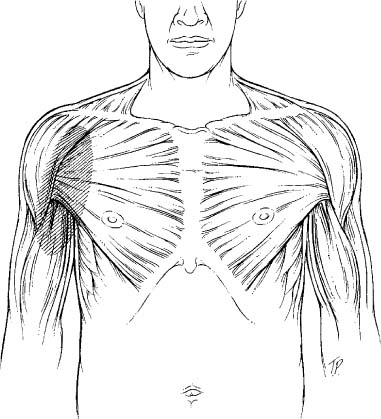
FIGURE 6-16 Biceps tendon pathology may cause pain to radiate down the front of the arm, but this is not specific to the biceps tendon.
Using three-dimensional electrogoniometers in a cadaver model, we simulated a Hawkins impingement sign, which places the arm in flexion and internal rotation. This study found that the bicipital groove and lesser tuberosity made contact with the coracoacromial ligament as the arm was placed into internal rotation (Fig. 6-17). Likewise, a Neer impingement sign was performed (flexion of the arm), and the lateral edge of the acromion had very close proximity to the lateral edge of the bicipital groove (Fig. 6-18). This study supported the cadaveric studies above, which would suggest that in certain positions the biceps tendon could be an integral part of the impingement process.

FIGURE 6-17 Coracoid impingement occurs when the arm is flexed and internally rotated so that the lesser tuberosity and bicipital groove make contact with the coracoid, coracoacromial ligament, and superior glenoid.
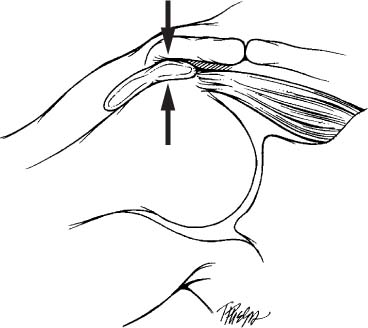
FIGURE 6-18 Subacromial impingement occurs when the arm is elevated and the greater tuberosity makes contact with the acromion.
Biceps Tendon Instability
Instability of the biceps tendon has received increasing attention due to the ability to evaluate arthroscopically the biceps and its pulley system. The most comprehensive evaluation of the spectrum of biceps instabilities was by Walch et al.49 They described three distinct clinical presentations that included biceps subluxations out of the bicipital groove, dislocations of the tendon out of the groove, and intra-articular dislocations of the biceps tendon.
Frank subluxation of the biceps tendon out of the bicipital groove has been reported by many authors, including Meyer.3 It is now known that full subluxation of the biceps tendon out of the bicipital groove is most commonly associated with partial or complete subscapularis tendon ruptures.50 In their study, which included 25 patients who averaged 54 years of age, Walch et al49 found that subluxations were almost always associated with supraspinatus tears and tears of the upper subscapularis.
Walch et al also found that dislocations of the tendon over the lesser tuberosity but not into the joint were associated with tears of the supraspinatus and infraspinatus tendons, and the average age of the patients with this pathology was 63 years of age. Complete intra-articular dislocations of the biceps tendon into the shoulder joint were found in patients with an average age of 56 years, and the pathology included extensive and massive rotator cuff tears. The symptoms of biceps subluxations or dislocations have been postulated to include shoulder pain and perhaps a clicking about the shoulder.51
Several physical examination methods of producing biceps tendon instability in the intertubercular groove have been described. All involve circumduction of the arm with rotation, which produces a painful click or pop along the anterior shoulder. The accuracy of these examinations unfortunately has never been evaluated. Walch et al49 in their 71 cases of biceps subluxation or dislocation noted that they never saw classical signs of biceps instability such as clicking or jerking. Because all of their patients had some coexisting rotator cuff pathology, they found that their patients had symptoms more consistent with rotator cuff disease than with instability of the biceps tendon. Finally, clicks around the shoulder are nonspecific, and it is difficult to ascribe a click to a specific pathology such as biceps instability.28
The Challenge of Diagnosing SLAP Lesions
The last area of controversy involves the diagnosis of SLAP lesions upon physical examination. The accuracy of the physical examination findings for SLAP lesions is an important issue not only for making the diagnosis of these lesions but also for following the results of treatment, whether it is medical or surgical.
There are several reasons the examination of SLAP lesions is difficult. First, there has been a controversy about how the labrum functions and how it produces symptoms. Many physicians have proposed that the labrum functions much like the meniscus in the knee, and that it would produce symptoms similar to the meniscus, specifically pain, locking, a click, or any combination of these symptoms. As a result, many physical examination tests or signs are meant to provoke either pain or a click with motion.
Studies have shown, however, that a click in the shoulder is nonspecific and can be due to a variety of pathologies.28,52 In our study of SLAP lesions, there was no difference in the incidence of clicks between patients who had SLAP lesions versus those who did not have SLAP lesions, which means that a click does not distinguish a patient with a SLAP lesion from one who does not have a SLAP lesion.
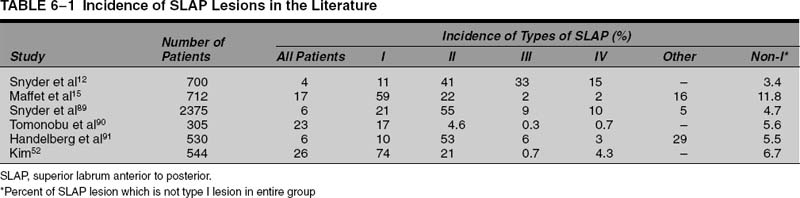
Another misconception is that the labrum can becomes trapped within the shoulder joint like a bucket handle tear of the meniscus in the knee. In our experience, a “trapped” labrum tear is rare, and when it is seen in a patient, it is typically due to a type III or IV labrum tear. Type III and IV labrum lesions are a minority of SLAP lesions in most series (Table 6-1).
The second reason SLAP lesions are difficult to diagnose is that there are many mechanisms that can produce SLAP lesions, so the patient’s history may not be helpful in making the diagnosis. These mechanisms include a fall upon the extremity with an outstretched arm, work-related injuries, shoulder dislocation, and overuse due to overhead sports or work.
Maffet et al15 reported on the mechanisms of injury to the shoulders in 67 patients diagnosed with SLAP lesions. Sixty-six percent of their patients had traction injuries to their arms (Table 6-2). This was most commonly traction in an inferior direction, such as when two people were lifting an object and one let go suddenly. Maffet et al reported that 13% of their patients had sustained a traumatic shoulder dislocation associated with their SLAP lesion. Snyder et al12 reported that a fall on an outstretched hand was the most common mechanism of SLAP lesions; however, Maffet et al reported that only 8% of their patients’ SLAP lesions were associated with a fall on an outstretched arm (Table 6-2).
One difficulty with many of these studies is that they include patients with other shoulder problems in addition to a SLAP lesion. When there are multiple pathologies present in a patient, it is difficult to ascribe symptoms to just one pathology. There is only one study of “isolated” SLAP lesions with no other shoulder pathologies. Snyder et al12 reported on 23 patients diagnosed arthroscopically to have an isolated SLAP lesion with no other shoulder pathology. In that cohort of patients they found that a compression force applied to the shoulder as a result of a fall onto an outstretched hand was the most common mechanism of isolated SLAP lesions.
| Mechanisms | % |
| Fall onto shoulder | 15 |
| Lifting heavy object | 13 |
| Traumatic dislocation | 13 |
| Insidious onset | 9 |
| Sudden anterior traction | 8 |
| Abduction and external rotation | 8 |
| Fall onto outstretched arm | 8 |
| Gradual with repetitive lifting | 6 |
| Motor vehicle accident | 6 |
| Sudden upward traction | 3 |
| Unknown mechanism during sports | 1 |
| Lateral traction | 1 |
Source: Adapted with permission from Maffet MW, Gartsman GM, Moseley B. Superior labrum-biceps tendon complex lesions of the shoulder. Am J Sports Med 1995;23(1):93–98.
SLAP, superior labrum anterior and posterior.
In their group with isolated SLAP lesions, the second most common mechanism of injury was a traction on the arm.12 This mechanism was seen as a result of sudden pull on the arm or as a result of repetitive motion due to overhead sports activity. The authors concluded that SLAP lesions could be caused by a compression force on the superior joint surface or by traction forces.
The last mechanism of injury postulated to produce SLAP lesions is that they are due to impingement or “internal contact” of the greater tuberosity upon the superior glenoid and labrum when the arm is in an abducted and externally rotated position.12,36,53–55 The association between SLAP lesions and repetitive overhead activities has been described in many studies,14,56,57 but the exact mechanism whereby this motion creates SLAP lesions is not entirely known.
Walch et al55 first reported this “internal impingement” phenomenon in a cohort of patients who had undergone arthroscopy of the shoulder. None of the patients had a history of trauma, and 12 of the 17 patients involved in overhead sports had a SLAP lesion. They suggested that the contact or impingement of the greater tuberosity upon the posterior and superior glenoid caused the labrum to tear in this area; however, in a study of patients undergoing arthroscopy with a variety of shoulder conditions, we found that contact occurred in 74% of patients.58 This is in agreement with Walch and colleagues, who speculated that this “internal contact” was physiological, and that it produced symptoms due to other factors such as repetitive motion or laxity.
Biomechanical studies seem to support that SLAP lesions can occur as a result of a variety of mechanisms. Bey et al27 studied the etiology of superior labrum detachments using a cadaver model. They found that inferior subluxation of the shoulder resulted in type II SLAP lesions in seven of eight specimens, and they concluded that traction on the biceps as seen with anterior and inferior instability could result in biceps tendon detachments.
In contrast, a cadaver model was used by Clavert et al59 to demonstrate that a fall on an outstretched arm can result in SLAP lesions. In this model the humerus was elevated and an axial load applied so that the greater tuberosity contacted the superior glenoid rim. The axial load was applied so that it simulated a forward fall or a fall with the hand behind the body (or backward fall). The forward fall position of the humerus resulted in five SLAP lesions in five shoulders, whereas the posterior fall position resulted in only two SLAP lesions in five specimens.
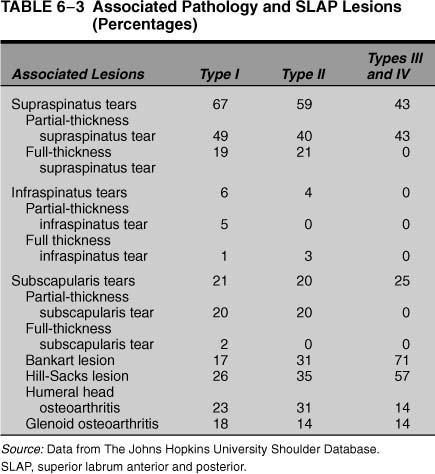
The third reason that SLAP lesions are difficult to diagnose is that they typically occur with other shoulder pathologies. In most series in the literature, isolated SLAP lesions with no other pathology typically varied from 160 to 12%52 of all SLAP lesions. Of 139 patients diagnosed with a SLAP lesion at our institution between 1992 and 2000, 123 patients (88%) were found to have associated intra-articular pathology (Table 6-3).
As a result, a large part of the difficulty in studying SLAP lesions is that they rarely occur without other shoulder pathology, and this coexisting shoulder problem could be the cause of the symptoms ascribed to the SLAP lesion. Because isolated SLAP lesions are uncommon as an isolated finding at the time of arthroscopy, it is difficult to say convincingly that the symptoms can be ascribed to the SLAP lesion. When coexisting pathology has been surgically treated along with a SLAP lesion, it is difficult to know which operation solved the problem; likewise, if the procedure fails, it is important to know whether it was the SLAP repair that failed or not.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree