CHAPTER 66 Techniques and Complications of Bone Graft Harvesting
Anterior Ilium
Three methods of harvesting autogenous bone graft from the anterior iliac crest are commonly used, each yielding only limited amounts of bone. The first is trephine curettage,1 which is a method of harvesting bone graft from either the anterior or posterior ilium. It usually yields only small curettings of cancellous bone. A small incision is made over either the posterior superior iliac spine or the iliac tubercle. Along the iliac crest, the tubercle is 5 cm posterolateral to the anterior superior iliac spine. The periosteum over the iliac crest is incised, and a small portion of the outer and inner table muscles is stripped slightly over the edge of the iliac crest. A Leksell rongeur or small osteotome is used to make a small rectangular window in the iliac crest by removing the cortex. This allows access to the medullary cavity of the ilium, and curets are used to remove cancellous bone. Because the crest is much thinner anteriorly than posteriorly, the area beneath the iliac tubercle must be used for bone harvest because it is the thickest portion of the anterior iliac wing.
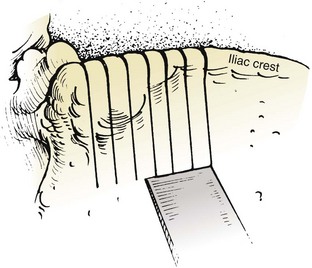
The trapdoor method (Fig. 66–1) of harvesting bone graft allows more extensive access to bone graft and is best suited for the anterior ilium. A skin incision is made over the anterior iliac crest, and an incision is made into the periosteum overlying the outer aspect of the crest. Beginning at the outer periosteal incision, a  -inch straight osteotome is used to make a horizontal cut in the iliac crest through both tables. The periosteum and fascial attachments of the iliacus and abdominal wall muscles (see Fig. 66–1) must remain intact on the inner edge of the horizontal cut to allow the crest to be “hinged back” like a trapdoor. Cancellous bone is then harvested from the medullary cavity, and the gluteal and abdominal wall fasciae are reapproximated after harvest. The normal contour of the iliac crest remains intact and yields cancellous strips and chips of bone.
-inch straight osteotome is used to make a horizontal cut in the iliac crest through both tables. The periosteum and fascial attachments of the iliacus and abdominal wall muscles (see Fig. 66–1) must remain intact on the inner edge of the horizontal cut to allow the crest to be “hinged back” like a trapdoor. Cancellous bone is then harvested from the medullary cavity, and the gluteal and abdominal wall fasciae are reapproximated after harvest. The normal contour of the iliac crest remains intact and yields cancellous strips and chips of bone.
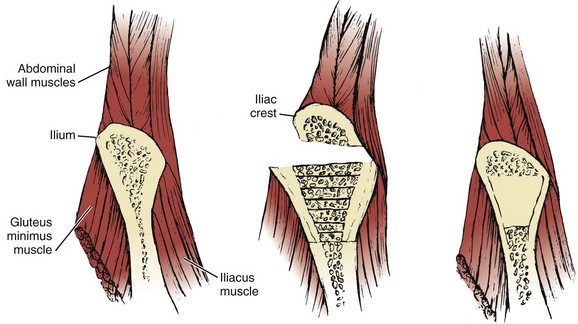
The subcrestal window technique (Fig. 66–2) is performed by making a skin incision over the anterior iliac crest near the iliac tubercle. The outer and inner table muscles are stripped subperiosteally from the ilium, and a small straight osteotome is used to remove the desired shape of bicortical ilium. This bone block can vary in size or shape, depending on that of the ilium itself. Care must be taken with the osteotome not to penetrate through the iliacus muscle medially (see Fig. 66–1).
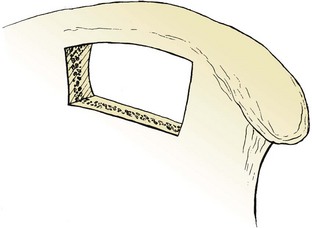
FIGURE 66–2 The subcrestal window technique of harvesting bone grafts. The iliac crest is left completely intact.
Full-thickness tricortical grafts, which include the iliac crest, may also be harvested from the anterior ilium. A skin incision is made just superior or inferior to the anterior iliac crest, and both the inner and outer table muscles must be subperiosteally stripped. Alternatively, if a retroperitoneal or thoracoabdominal approach to the lumbar spine has been performed, subcutaneous dissection over the iliac crest, superficial to the abdominal musculature, obviates the need for a separate skin incision. The periosteum is then incised overlying the anterior iliac crest, thus releasing the abdominal wall muscles from their insertion on the iliac crest itself (Fig. 66–3). Stripping of the outer (tensor fascia lata and gluteus medius) and inner (iliacus) table muscles can be accomplished (see Fig. 66–3), thereby exposing the entire thickness of the ilium for harvest. An oscillating saw or osteotome can then be used to remove full-thickness tricortical grafts.
Posterior Ilium
The ideal method of harvesting bone graft from the posterior ilium should yield sufficient quantity of cancellous and corticocancellous bone for posterior or posterolateral fusion. Methods such as “oblique sectioning of the crest,”2 “cortical subcrestal windows,” and “trapdoors” are usually performed anteriorly and provide only limited amounts and sizes of bone graft, which are usually insufficient for posterior lumbar arthrodesis. Gouges tend to provide uneven corticocancellous strips and chips of bone that may not be suitable to span adjacent transverse processes. Curets provide small chips of bone that are suitable only as “filler” pieces. Osteotomes work well by providing relatively consistent sizes and shapes of bone pieces that can properly bridge adjacent transverse processes. Ideally, the osteotome should yield pieces of bone at least 6 cm in length, 5 to 7 mm in width, and with a cancellous thickness of 5 to 7 mm.
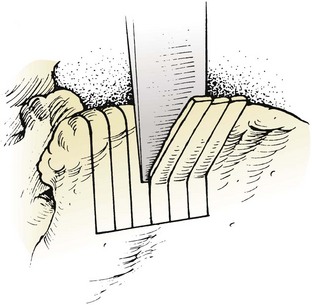
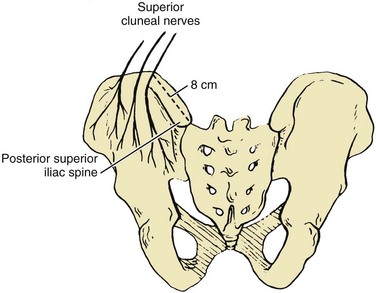
Bone graft harvest is begun by exposing the posterior iliac crest through a separate skin incision (Fig. 66–4). Alternatively, if the laminectomy skin incision allows, subcutaneous dissection may be performed through it, thereby permitting the surgeon to avoid a separate incision in the skin. The periosteum is incised over the iliac crest, and subperiosteal stripping of the outer table muscles of the posterior ilium is performed by using a Cobb periosteal elevator. A Taylor retractor is placed deep in the wound and oriented vertically to avoid penetrating the sciatic notch. A sterile gauze or chain is then hung from the handle of the retractor and a small weight (usually 2 to 5 pounds) is suspended from it, thereby leaving both of the surgeon’s hands free. A  -inch straight osteotome is used to cut parallel strips of bone from the crestal edge in a ventral direction (Fig. 66–5). Care is taken to prevent full-thickness (bicortical) bone cuts. Successive vertical cuts of equal length are made approximately 7 mm apart. A
-inch straight osteotome is used to cut parallel strips of bone from the crestal edge in a ventral direction (Fig. 66–5). Care is taken to prevent full-thickness (bicortical) bone cuts. Successive vertical cuts of equal length are made approximately 7 mm apart. A  -inch curved osteotome is then used to connect the cuts on top (Fig. 66–6) of the crest and distally (Fig. 66–7). The curved osteotome is then gently tapped ventrally between the inner and outer tables of the ilium to connect with the distal cut (Fig. 66–8). The corticocancellous strips are removed, leaving a majority of the cancellous bone of the intramedullary cavity available for removal with gouges, with residual cancellous bone then removed by the curets.
-inch curved osteotome is then used to connect the cuts on top (Fig. 66–6) of the crest and distally (Fig. 66–7). The curved osteotome is then gently tapped ventrally between the inner and outer tables of the ilium to connect with the distal cut (Fig. 66–8). The corticocancellous strips are removed, leaving a majority of the cancellous bone of the intramedullary cavity available for removal with gouges, with residual cancellous bone then removed by the curets.
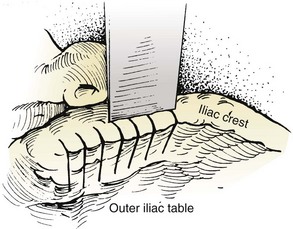
FIGURE 66–6 A straight osteotome is used to elevate the corticocancellous strips off the outer table.
Fibula
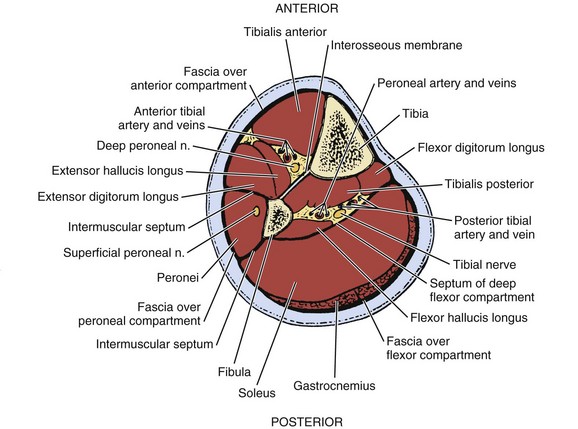
With readily available allograft bone, autogenous fibula is rarely used. Its uses are generally limited to anterior structural support in the cervical spine after corpectomy. In order to minimize problems with ambulation, autogenous fibula must be harvested meticulously. Under tourniquet control, a skin incision is made to parallel to the posterior border of the fibula, centered at the junction of the middle and distal thirds of the fibular shaft. The incision is carried down through the intermuscular septum onto the bone. Subperiosteal dissection is used to elevate the peroneal muscles from the anterolateral surface of the fibula, the extensor digitorum longus muscle from its anterior surface, the tibialis posterior muscle from its anteromedial surface, the flexor hallucis longus muscle from its posteromedial surface, and the soleus from the posterior surface (Fig. 66–9). It is essential to stay subperiosteal when circumferentially stripping the fibula, even though these muscles may not be individually recognizable. After the bone is completely stripped, a graft may be harvested with either an oscillating saw or a Gigli saw.
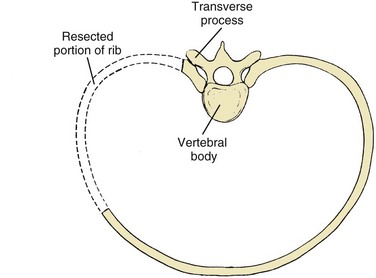
Rib
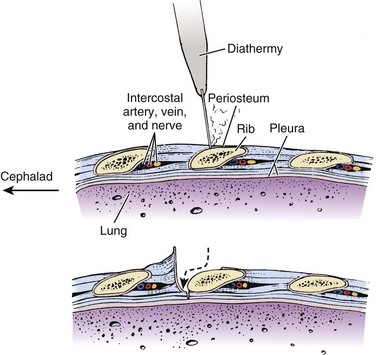
Ribs are harvested almost exclusively for use with thoracoabdominal or transthoracic approaches to the spine, where they are removed to assist exposure. Dissection through the latissimus dorsi and trapezius muscles exposes the rib and assists harvest. Electrocautery or a scalpel is used to incise the periosteum over the rib, and the superficial portion of the rib is subperiosteally stripped with a periosteal elevator (Fig. 66–10). A rib stripper is then used to completely subperiosteally strip the pleural surface of the rib. This maneuver is performed all the way to the vertebral and sternal ends of the ribs. A rib cutter is then used to excise the rib at its costochondral and costovertebral junctions (Fig. 66–11).
Complications of Bone Graft Harvest
Pain
Pain is considered a complication because it is the most common complaint after autogenous iliac bone graft harvest.3,4 Donor site pain may persist long after the arthrodesis site ceases to be a source of discomfort. Several studies5–7 have reported that up to 15% of patients may have persistent pain at the iliac donor site for more than 3 months after harvesting of the bone graft. There are no differences in the incidence and degree of pain between anterior and posterior harvest sites.8 Although it is opined that the pain is due to the extent of periosteal dissection, the rich blood supply and innervation of the site, and the role of weight bearing, none completely explains the persistent pain. However, limiting the degree of dissection and periosteal stripping will diminish the chance of this complication occurring.
Arterial Injury
The superior gluteal artery arises from the internal iliac artery before it exits the pelvis. It then enters the gluteal region, through the proximal portion of the sciatic notch (Fig. 66–12), and supplies the bulk of the gluteal muscle. Formation of an arteriovenous fistula of the superior gluteal vessels has occurred from penetration of the sciatic notch with the sharp tip of a Taylor retractor used to provide exposure during bone harvest.9 I have encountered four cases of massive hemorrhage deep in the sciatic notch from inadvertent penetration of the notch by an osteotome or gouge during the harvesting of bone from the posterior ilium. In every case, the injured superior gluteal artery stump retracted proximally into the pelvis. In two of the four cases, exposure of the retracted injured vessel in the sciatic notch necessitated the use of a Kerrison rongeur to remove bone from the sciatic notch to gain successful control of bleeding. In one case, however, ligation of the vessel could be performed only after it was exposed through a separate retroperitoneal approach.
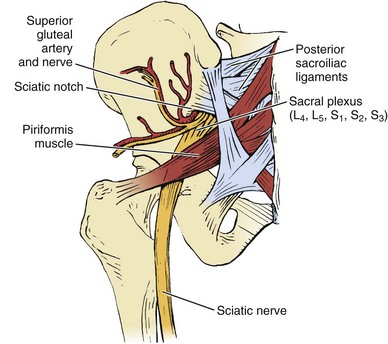
FIGURE 66–12 Posteroanterior view of the pelvis showing the neurovascular structures in the sciatic notch.
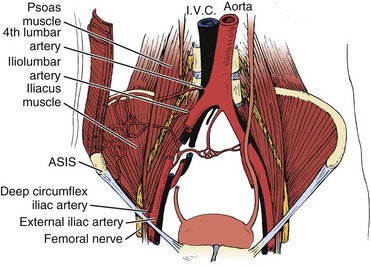
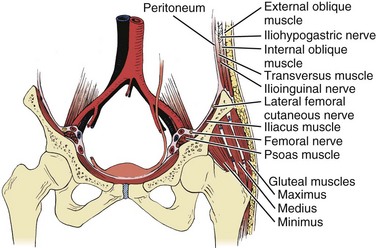
Three major arterial structures (Fig. 66–13) traverse the anterior surface of the iliacus muscle: the fourth lumbar artery, iliolumbar artery, and deep circumflex iliac artery. They provide an extensive blood supply to the iliacus, quadratus lumborum, and psoas muscles and frequently anastomose with each other. Harvesting of bone grafts from the inner table of the anterior ilium can damage this blood supply. Bleeding can be minimized by strict attention to subperiosteal stripping of the iliacus muscle.
Nerve Injury
Ilioinguinal Nerve
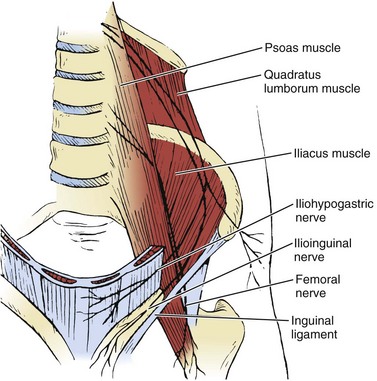
The ilioinguinal nerve is a branch of the first lumbar nerve, which crosses the psoas muscle and subsequently courses laterally over the iliacus and quadratus lumborum muscles (Fig. 66–14). When it reaches the level of the anterior iliac crest, it traverses the internal oblique and transversus abdominis muscles, supplying their lower portions with motor fibers. It then travels under the external oblique muscle, enters the inguinal canal, and descends to supply sensation to parts of the penis, proximal and medial thigh (Fig. 66–15), scrotum, and adjacent abdomen. Vigorous retraction of the abdominal wall and iliacus muscles during bone graft harvest from the inner table of the anterior ilium was reported to have led to ilioinguinal neuralgia.10 Treatment typically consists of local nerve blocks and patience. Because prevention is preferable to treatment, gentle retraction of iliacus and abdominal wall muscles will minimize the risk of injury to this nerve.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


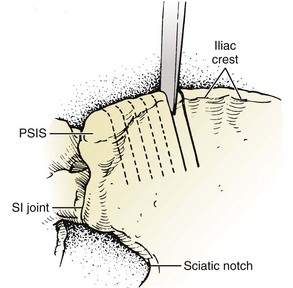
 -inch straight osteotome. PSIS, posterior superior iliac spine; SI, sacroiliac.
-inch straight osteotome. PSIS, posterior superior iliac spine; SI, sacroiliac.