CHAPTER 15 Targeting Pain Generators
Spinal pain is very common and exacts a significant toll for the individual and society. Low back pain has a lifetime prevalence from 54% to 80%, an annual prevalence of 15% to 45%, and a point prevalence of 30%.1 Low back pain is the second most common reason for disability among adults in the United States with approximately 150 million work days lost per year.2,3 Spinal pain is the second most common reason for outpatient generalist physician visits, the third most common reason for surgical interventions, and the fifth most common reason for hospitalization.4,5 The cost to care for patients with low back pain is more than $100 billion per year.6 The prevalence of individuals seeking care for low back pain also seems to be increasing significantly. From 1992-2006, the prevalence of patients presenting with chronic impairing low back pain increased from 4% to 10%.7 Cervical pain exacts a significant toll in terms of individual morbidity and socioeconomic burden. Targeting pain generators through precision diagnostic methods is the first step toward appropriate and effective treatments for chronic spinal pain.
Much of the epidemiologic data on low back pain are nonspecific, meaning that a cause cannot be found in most cases. Despite evidence to the contrary in the 21st century, these older, inaccurate epidemiologic studies continue to be quoted by current authors. One of the oldest epidemiologic studies commonly quoted was published more than 40 years ago by Dillane and colleagues8 and was based on a retrospective practice audit of data gathered more than 50 years ago. Dillane and colleagues8 reported that they could not detect a cause for low back pain in approximately 80% of female and 90% of male patients with acute back syndrome. These authors did not report the use of any x-ray studies and apparently relied solely on history and physical examination.8 They diagnosed approximately 11% of male patients and approximately 4% of female patients with low back “strain.” Until more recently, the only tools to diagnose the etiology of low back pain have been history, physical examination, and sometimes x-ray or computed tomography (CT) scan.
In 1982, Nachemson9 reviewed the literature on chronic low back pain. In perhaps the most frequently quoted epidemiologic study on the cause of chronic low back pain, Nachemson9 reported that in only 15% of cases could a pathoanatomic explanation be found for patients with chronic low back pain (>3 months). Nachemson9 stated, “probably very little can be done at our present state of ignorance to treat these patients and to improve their natural histories.” Low back pain is a symptom, not a diagnosis, in the same way that abdominal pain is a symptom and not a diagnosis. In acute cases of low back pain, this nonspecific diagnosis usually suffices because most cases of acute, first-time low back pain resolve with minimal intervention; however, when low back pain becomes chronic, recurrent, and disabling, the clinician must diagnose the source of the pain so that an appropriate treatment plan may be devised.
When a source of pain is not obvious, diagnosis often depends on who makes the diagnosis and sets the reference standards by which the diagnosis is “proven.” Who is right? For that matter, can anyone reliably diagnose the cause of chronic benign spinal pain? Many authors argue that chronic benign spinal pain is largely due to exaggerated functional complaints and irreversible central nervous system sensitization,10 making pain self-perpetuating and diagnosis all but impossible. These contentions are not often supported by primary studies,11 however, and authors and clinicians question this diagnosis.12,13
Interventionalists developed and refined precision, fluoroscopically guided diagnostic interventional spine procedures in the 1980s and 1990s14 to diagnose and treat nonspecific spinal pain better. Fluoroscopically guided block procedures are now considered the reference standard to confirm a tissue diagnosis. Out of the previous era of “ignorance,” many diagnostic protocols have been validated and standardized.15,16 Using the results of precision-guided diagnostic procedures, surgeons identify spinal segments for fusion at various stages of the degenerative cascade.17 Most surgeons still depend on an accurate diagnosis of a specific pain generator to select appropriate therapy18 because surgical results for chronic benign pain syndromes without a reversible anatomic cause are generally poor.19
The debate continues regarding diagnostic injections as new research emerges, along with better treatment options. Spinal pain is a complex interaction of many biopsychosocial factors. Chronic spinal pain may originate from one or more spinal levels and different anatomic structures in the anterior, middle, and posterior columns. Spinal pain also varies over time. Pain can be caused by abnormal mechanical stress on normal tissue affected by structural deformity, normal mechanical stress on injured tissues, minor stress on chronically inflamed and sensitized tissues, damaged nerves, and a varying combination of all of these. Chronic pain causes a greater or lesser degree of central sensitization and together with a multitude of functional factors, including the requirement for copious amounts of opiates, often makes accurate diagnosis difficult. Nevertheless, it can be argued that most chronic axial spinal pain is due to accumulated repetitive strain or low-grade trauma,20 acute injuries to the major underlying structures and their supporting ligaments, or both. Ongoing stimulation from these peripheral structures to a greater or lesser extent maintains a state of peripheral and central sensitization. In time, adaptive responses within the posterior, middle, and anterior columns may attenuate, exacerbate, or cause new sources of pain.
Despite this complexity, specific tissue pain generators can be hypothesized based on history, physical examination, imaging studies, and response to directed treatment. Interventional procedures are used to test the hypothesis that pain is related to a structural abnormality hypothesized by clinical and imaging findings. (The word hypothesis is used loosely here; arguably one only can confirm a clinical impression using diagnostic blocks. A hypothesis is confirmed using a study protocol that can show approximately <5% probability that the findings are due to chance). Foremost, interventional procedures are perhaps best used to refute one’s hypothesis that a particular structure is painful. That is, diagnosis is made through the process of systematically excluding various tissue causes of axial and extremity pain in the posterior, middle, and anterior columns.19
This chapter presents primarily evidenced-based standards and some expert opinions for confirming or refuting one’s hypothesis that a particular structure, structures, or segments are a source of spinal pain.15 A discussion of pain resulting from “red flag” conditions, such as fracture, tumor, infection, systemic diseases, or referred from nonspinal structures, is not included; likewise, “yellow flag” conditions (psychosocial factors) are not discussed in detail. Evaluation of the anterior column using provocative discography is discussed elsewhere, so the discussion in this chapter is focused on diagnosis of pain originating from the posterior and middle columns, in particular, pain originating from the zygapophyseal joint and sacroiliac joint in the posterior column and from the nerve root, dorsal root ganglion, and dura in the middle column. The diagnostic use of injection procedures is explored and not their therapeutic value other than the diagnostic value of response or nonresponse to treatment. Finally and most importantly, this chapter is not a systematic review, and the interested reader is referred to numerous systematic reviews on the diagnostic value of spine injections.1,15,16,20–26
Diagnostic Analgesic Injections as Reference Standard
The belief that chronic benign spinal pain is difficult to diagnose is supported by the low specificity and sensitivity of the history, physical examination, and various imaging modalities as the reference standard for diagnosing chronic benign spinal pain11,27,28 and a bias that chronic pain is to a greater rather than lesser extent a neuropathic process with central sensitization.19 If one uses interventional diagnosis with precision fluoroscopically guided procedures as a reference standard for identifying pain, however, one can arrive at a tissue diagnosis in approximately 70% to 80% of cases.29,30 Which approach is right? Truth usually lies somewhere in between.
The rationale for facet blocks is based on the anatomic fact that the innervation of facet joints (medial branches) is known and that zygapophyseal joints are capable of causing pain.15 Local anesthetic blocks rely on the specificity of anesthetizing a single or limited number of structures or nerves and on the patient’s capacity to distinguish clearly a reduction in preblock pain after anesthetizing one or more structures. Injection of a limited volume of local anesthetic into a zygapophyseal joint or its nerve supply is relatively specific for anesthetizing a joint and its capsule. Similarly, local anesthetic injected into the disc should anesthetize nociceptors within radial annular fissures that communicate with the nucleus. When anesthetizing the nerve root within the middle column, the block is less specific for axial pain relief because several structures may be partially blocked (e.g., dorsal root ganglion, ventral rami, sinuvertebral nerve, posterior longitudinal ligament).
Anesthetizing a structure does not reveal the cause of pain; anesthetizing the nerve supply simply relieves pain. This is an important concept. The cause of pain should dictate the type of treatment, and the treatment is only as good or bad as its success in eliminating or modulating the cause. If the cause of pain in the case of a specific zygapophyseal joint is synovial inflammation, one would expect short-term to intermediate pain relief after the intra-articular injection of corticosteroids. If a patient’s pain is due to mechanical or neuropathic causes, there is no reason that corticosteroids would be effective other than the expected duration of the local anesthetic. There is no reason that there should be longer term pain relief except for the expected rate of placebo response or reported pain relief secondary to spontaneous pain regression.31 That is, relief of pain during the local anesthetic phase does not distinguish irreversible neuropathic pain from reversible nociceptive pain. In the case of chronic radicular pain, significant relief of pain for several weeks after the injection of corticosteroids would suggest that there is a reversible structural cause.32
Testing Protocols for Diagnostic Injections
As essential as precision technique is in the performance of diagnostic blocks, so is standardized assessment. Standardized diagnostic block evaluation sheets should be filled out for each patient; detailed postprocedure assessment protocols and sample evaluation instruments are available in the International Spine Intervention Society Practice Guidelines.15 Preprocedural and postprocedural evaluation should be performed by unbiased personnel and checked by the physician. It is recommended that the patient fill out a body pain diagram with pain scores (visual analog scale [VAS]) before and after the procedure. Additionally, the patient should rate current pain levels with various movements (e.g., lumbar flexion, extension, side-bending, sitting, and standing).
Confounding Factors
Sedation
An important, potentially confounding factor when performing diagnostic blocks concerns the use of sedation. Logically, one would assume that administration of opiates and sedatives before a diagnostic block would increase the false-positive rate; however, Manchikanti and colleagues33 found that this proportion of patients was relatively small, and there was no difference with use of saline, opiate, or sedative. In a randomized study of 60 patients, Manchikanti and colleagues33 titrated medication to relaxation using saline, midazolam, or fentanyl. They found that only 50% of patients receiving sodium were relaxed, whereas 100% of patients receiving either fentanyl or midazolam were relaxed. In all groups, 10% of the patients reported greater than 80% pain relief with active motion testing. Even so, typically, one limits or omits sedation before a diagnostic injection, however.
Biopsychosocial Factors
More recently, authors have reiterated the importance of shifting the concept of “backache.” Kikuchi34 recommended changing the term spinal disorder to biopsychosocial pain syndrome and the term morphologic abnormality to mechanical, functional disorder. According to Kikuchi,34 morphologic and structural abnormalities do not always explain all of a patient’s pain, and chronic backache should not be seen as an isolated spinal disease. A significant amount of scholarship has been devoted to enumerating the psychosocial factors associated with spinal pain. In a classic study comparing workers with symptomatic disc herniation (requiring surgery) versus asymptomatic workers, significant differences were found in three areas: presence of nerve root compromise, psychosocial factors (depression, anxiety, marital status, self-control), and work perception (satisfaction, job loss, occupational stress, intensity of concentration).35 Of the risk factors, two of three were functional, not morphologic.
Although the long-term results of treatment for chronic axial back pain may be influenced by various psychosocial factors,36,37 the possible effect of psychosocial factors in determining the patient’s tested perception of pain and functional improvement with treatment does not indicate that the diagnosis was incorrect. In many cases, when a “biologic” pain generator can be correctly identified and treated, the psychosocial distress resolves. If it is true that psychological variables determine whether a patient admits relief on various testing instruments, does the evidence of physiologic distress noted on test scores reverse when the patient’s chronic pain is relieved?
Wallis and colleagues38 studied 17 patients after whiplash injury with a single symptomatic cervical zygapophyseal joint who were enrolled in a randomized controlled trial of percutaneous radiofrequency neurotomy. At 3 months after the procedure, all patients whose pain was relieved had complete resolution of preoperative psychological distress; in contrast, all but one of the patients who did not experience pain relief continued to experience psychological distress. Manchikanti and colleagues39 found no correlation between somatization disorder and inappropriate Waddell signs and symptoms to response in pain relief after a comparative double block protocol for diagnosing facet pain. Derby and colleagues40 found no difference in response to pressure-controlled disc stimulation between patients with abnormal psychometric Distress Risk Assessment Method scores and asymptomatic volunteers.
Posterior Compartment: Zygapophyseal Joint and Sacroiliac Joint
Zygapophyseal Joint
Each spinal segment is composed of a three-joint complex: the intervertebral discs and two posterolateral facet joints.41 Facet joints can also be called zygapophyseal joints. The word apophysis is Greek, meaning an “offshoot” or a “bony protruberance.”42 Anatomically, the zygapophyseal joint is an outgrowth of the vertebral body. The zygapophyseal or facet joints are formed by the articulation of the inferior articular process of one vertebra with the superior articular process of the adjoining vertebra. Zygapophyseal joints have classic synovial joint features: hyaline cartilage surfaces, a synovial membrane, and a surrounding joint capsule.43 Facet joints have varied morphology and function based on their location within the spine. Although the intervertebral disc is loaded primarily in flexion, the zygapophyseal joints are loaded in extension and lumbar rotation.44,45 The orientation of the facet joint varies based on the requirements of regional spine function. Lumbar facets are situated sagittally to limit axial rotation and loading, whereas the cervical and thoracic facets are oriented coronally to limit shearing forces on the disc. Innervation is via the medial branches of the dorsal ramus in most locations.
Pathophysiology of Facet Pain
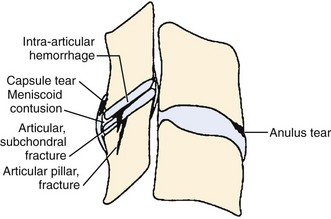
Traumatic injury to lumbar and cervical zygapophyseal joints is common and probably occurs to a lesser extent to the thoracic joints. In the setting of trauma, there is a clear pathophysiologic difference between facet joints and nontraumatic controls. Zygapophyseal joint sections from autopsy specimens of individuals with a past history of trauma but dying of natural causes show significant age-related, gender-related, and trauma-related changes in the bone, cartilage, and soft tissues, including subchondral sclerosis, fibrillation and splitting of cartilage, and cartilage length differences, versus subjects with no history of trauma.46 Histologic sections of the lumbar zygapophyseal joints of mostly motor vehicle accident victims revealed fractures of the superior articular process, central infarctions of the subchondral bone plate, and capsule tears including the ligamentum flavum.47,48 Most tissue sections (77%) show soft tissue injuries, and approximately 30% (11 of 33) show fractures and infarctions. Sections from the cervical spine in trauma victims show similar injuries to the zygapophyseal joint articular cartilage and annular lesions in the intervertebral discs and cartilaginous endplates (Fig. 15–1).49 In the lumbar and cervical spines, lesions were found exclusively in the trauma patients and in none of the patients in the control group.46,49,50
Many of these pathoanatomic findings are occult on routine x-ray, CT scan, and magnetic resonance imaging (MRI) but may be the cause of ongoing neck pain in survivors of motor vehicle accidents or other significant trauma. In a small study with short-term follow-up (approximately 3 months), Eisenstein and Parry51 examined zygapophyseal joints in 12 patients who underwent successful fusion for zygapophyseal joint mediated pain (diagnosed by provocation arthrography, intra-articular blocks, and negative discography) versus controls and found histologic changes similar to changes of chondromalacia patellae and osteoarthritis of large joints. The most frequent finding was focal full-thickness cartilage necrosis or loss of cartilage with exposure of subchondral bone; osteophyte formation was absent in all specimens.51 Degenerative histologic findings alone do not make a definitive diagnosis of facet syndrome, however. Ziv and colleagues52 reported a high proportion of coarsely fibrillated or ulcerated (or both) facets in fresh cadaveric spines from young adults (30 to 50 years old); such degeneration remains constant throughout adulthood.
Traumatic and repetitive injury leading to painful “facet arthritis”48 may cause pain because zygapophyseal joints and their capsules are heavily innervated structures subject to high stress and strain during spinal loading.53 Joints comprise free and encapsulated nerve endings containing substance P and calcitonin gene-related peptide.54–56 Substance P, calcitonin gene-related peptide, and immunoreactive sensory and autonomic nerves are found in zygapophyseal joint synovial membranes.57 Facet capsules contain low-threshold mechanoreceptors, mechanically sensitive nociceptors, and silent nociceptors.58 These low-threshold and high-threshold mechanoreceptors fire when the joint capsule is stretched or compressed, and their firing can be suppressed by injected lidocaine and hydrocortisone.59 In animal models, induced inflammation decreases the threshold of nerves within the joint capsules and causes elevated baseline discharge rates.59 In animal models of knee arthritis, acute inflammation sensitizes fine articular afferents, which become active at rest and respond more vigorously to routine painless joint range of motion.60
Excessive stretching damages the zygapophyseal joint capsules and causes axonal swelling, retraction balls, and inflammation.58 The result is hyperexcitability and spontaneous firing, which are synonymous with neuropathic pain. Capsular injury during a whiplash injury may cause persistent neck pain secondary to chronic capsular overstretching. Animal studies suggest that facet capsule strains comparable to strains previously reported for whiplash kinematics and subcatastrophic failures of this ligament activate nociceptors within the capsule.61–65 In addition, chronic capsular loading in animals may cause central inflammation resulting in mechanical hyperalgesia and in some cases centrally maintained pain.56,63,66,67
Animal studies showing central sensitization are consistent with the widespread hypersensitivity documented in whiplash patients. Although focal sensitization to mechanical stimuli may be found 3 months after whiplash injury, which mostly resolves by 6 months, some patients develop persistent pain with symptoms that are consistent with chronic neuropathic pain.68 Patients with persistent pain at approximately 6 months show signs of more widespread hyperalgesia69 and hypersensitivity to cutaneous and muscular stimulation in neck and lower limb consistent with central hypersensitivity.10,70
If chronic pain originating from injury to the zygapophyseal joints is due to capsular stretch and maintained by central hypersensitivity, local anesthetic with or without corticosteroid should suppress nociceptive input for the duration of the local anesthetic effect and in some cases (e.g., similar to a sympathetically maintained pain state) for days to weeks.71 If most of a patient’s pain is due to mechanical and central causes, there would be no reason why local anesthetic and corticosteroid would be more effective than local anesthetic alone.72–74 Former and latter logical outcomes are supported in prospective and randomized controlled trials,74 although alleviating pain with medial branch blocks was shown in one study to relieve pain for an average of several months.75,76
Decreasing peripheral input 6 months or longer by heat ablation of medial branches relieves pain77; the pain typically returns within the expected time it takes for the medial branches to regenerate. Such prolonged relief of pain, if accompanied by resolution of widespread hypersensitivity, would imply that central hypersensitivity is reversible when the peripheral source of input is interrupted. That is, if there is a concern that persistent central hypersensitivity would lead to failure of a proposed localized or segmental stabilization procedure, resolution of widespread and local hypersensitivity after medial branch neurotomy might predict that decrease in nociceptive input by surgical stabilization would be successful. Zygapophyseal joint pain often occurs at more than one segment, however, and one must identify adjacent or skipped level sources of zygapophyseal joint pain, especially if one is considering surgical fusion or arthroplasty.
When cadaveric lumbar spines are anteriorly fixated at one level, motion is transferred to adjacent segments causing increased capsular stretch in the adjacent facet joints.78 In extension, cervical arthroplasty models exhibit significant increases of facet force at the treated level. In the fusion model, the facet forces decrease at the treated segment and increase at the adjacent segment.79 Failure to recognize symptomatic pathology at an adjacent level or the same level may lead to early or late return of pain. This is not a failure of the diagnostic blocks; it is a failure to obtain a thorough diagnosis.
Rationale for Control Blocks in Diagnostic Facet Intra-articular and Medial Branch Blocks
Can a diagnosis of facet syndrome be made without injections? The diagnosis of zygapophyseal joint pain is typically hypothesized based on clinical findings and imaging studies. Most clinicians rely on a variety of favorite criteria, such as localized unilateral pain that is worse in extension, pain worse in the morning and better with gentle movement, concordant pain provoked with palpation approximately 1 cm lateral to the midline over the zygapophyseal joints, and imaging studies showing signs of facet degeneration. A “facet syndrome”80 diagnosed by clinical findings has not been substantiated, however, if one uses as a reference standard the relief of pain after placebo-controlled anesthetic blocks.23,27,81 The current best evidence has not found any individual clinical finding or cluster of findings that can predict response to the reference standard of pain relief after local anesthetic block of the medial branches or intra-articular zygapophyseal joint block.
The purpose of diagnostic facet blocks is to establish the diagnosis or rule it out, similar to a liver biopsy of a suspicious lesion. Diagnostic facet blocks are a tertiary intervention in patients with chronic pain that has not resolved with time and conservative care. The current standard for the diagnosis of facet mediated pain is the use of controlled differential (double) blocks to confirm or refute one’s hypothesis that the facet joint is a pain generator. Because of the high false-positive rates of single diagnostic blocks, a single block does not constitute a diagnosis, and control blocks are essential to decrease the incidence of false-positive responses.82 The reported false-positive rate of a single diagnostic block ranges from 17% to 63%.83 In a retrospective review of 438 patients using a double block paradigm requiring 80% relief, the false-positive rates for a single diagnostic block were 45%, 42%, and 45% for the cervical, thoracic, and lumbar regions.83
Although Cohen and colleagues84 showed that treatment results after medial branch neurotomies were not changed by requiring a placebo control, the current published standard of interventional societies requires a confirmatory block before making a diagnosis of zygapophyseal joint mediated pain. The best-studied double block protocol requires a difference in pain relief duration based on a shorter or longer acting medication—typically, greater than 1 hour for lidocaine and greater than 2 hours for bupivacaine.85,86 Because the goal is to have a placebo control and because consent and patient compliance issues hinder using a saline block control, one may argue that any prior diagnostic injection in which the patient reports no relief is a valid control block, especially because the patient and the physician were anticipating relief. Because many insurance companies in the United States no longer authorize or consider double blocks medically necessary, the occurrence of a previous “negative” block evaluation could be the negative control.
When the treatment is relatively benign, convincing relief with physician and staff testing after facet or medial branch injections in an older patient with clinical symptoms consistent with zygapophyseal joint pain may not justify confirmatory injections.84 A young patient who has little or no facet abnormalities, who is on a significant dose of narcotics, and who reports less than convincing approximately 80% relief should undergo a second confirmatory injection before considering interventional or surgical treatment based on the block results.
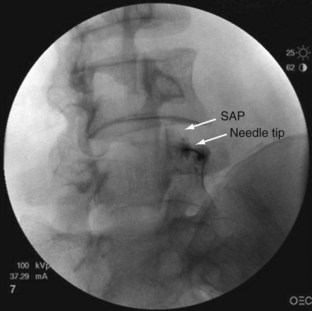
The rationale for how many and which levels to test is debated. Levels are typically chosen based on known pain referral patterns, prevalence studies, and localized manual palpation. Using a comparative double block control, Manchukonda and colleagues83 found that most often two joints were symptomatic in the lumbar spine and three adjacent joints were symptomatic in the thoracic and cervical spine. The most logistically efficient and least costly method is to rule out facet pain globally on the side or sides of the patient’s pain and at the proximity of approximately two to three adjacent levels. One would inject (in the case of lumbar spine) the L2-5 medial branches to block the L3-4, L4-5, and L5-S1 zygapophyseal joints (Fig. 15–2 shows medial branch anatomy of the lumbar spine; Fig. 15–3 shows a lumbar medial branch block). If no relief occurred and there was no evidence that the higher joints were involved, and if one is confident that the facets were denervated, one can eliminate facet pain from the diagnosis. If the result is positive, one can perform more selected denervation on a confirmatory injection. Although this could be argued to be the most efficient method, many third-party payers in the United States limit injections to two levels per session.
Diagnostic Accuracy
Kaplan and colleagues87 reported that medial branch blocks may fail because of venous uptake. Venous uptake occurred in 7 of 20 (35%) medial branch blocks. If venous uptake was encountered, repositioning of the needle resulted in joint anesthesia only 50% of the time. When venous uptake was encountered, the subjects were brought back for a later injection. These findings stress the importance of using contrast medium for medial branch blocks and carefully observing the flow pattern. Kaplan and colleagues87 also found that in 11% of cases they were unable to anesthetize the joint, even in the absence of venous uptake. Medial branch blocks in the lumbar spine would have an 11% false-negative rate; this may have been due to anomalous or collateral facet innervation or insufficient volume of local anesthetic reaching the target nerve.
Rarely discussed is the consistency with which one may expect a longer duration of action of bupivacaine versus lidocaine. Although bupivacaine has a longer duration of action than lidocaine, the mass of drug reaching the nerve is the most important variable, and one cannot guarantee that the same amount will be available on consecutive sessions. In addition, most patients are not kept in the recovery area for the duration of local anesthetic to be evaluated, and the duration depends on a patient’s self-reporting, which may or may not be consistent between injections. Lord and colleagues86 showed that using a double block comparative standard, 65% of patients failed to recognize the difference in duration of pain relief but did accurately distinguish a separate placebo-controlled block with saline.
The crucial factors for specificity of the diagnosis of zygapophyseal joint pain are accurate targeting of the intended structure under fluoroscopy, confirmed by contrast medium, and the delivery of the appropriate volume of local anesthetic. Intra-articular joint blocks are specific, unless there is a medial capsular tear or injection of excessive volumes (>1 mL injected into a lumbar zygapophyseal joint or 0.3 mL injected into a cervical zygapophyseal joint), which may rupture the capsule and spread medially into the epidural space.88,89 Many early studies of facet intra-articular blocks used 2 to 8 mL per injection. When reviewing negative studies regarding facet injections and the systematic reviews that still quote these studies, the discerning reader should check the total volume of injectant used.89,90 Destouet and colleagues89 found that volumes of injectant of 0.5 to 1.5 mL commonly ruptured the superior recess of the capsule and extravasated; in later studies, Destouet and Murphy91 aspirated the 0.5 to 1.5 mL of contrast dye before adding local anesthetic and steroid. Cadaveric studies performed with variable volumes of methylene blue injected into facet joint (1 to 4 mL) showed that the dye extended not as expected into the paraspinal tissues but rather into the epidural space and around the spinal nerves.92 Moran and colleagues92 described the facet capsule as thick dorsally, whereas anteriorly the facet synovial membrane is contiguous with the ligamentum flavum, and the adipose tissue in the superior recess is in direct contact with the adipose tissue around the spinal nerve. Randomized controlled studies validate the specificity of medial branch blocks for relief of zygapophyseal joint mediated pain.93
To maintain the specificity of medial branch block, a low volume of local anesthetic is used to anesthetize a specific cervical93 or lumbar medial branch.87,88 If volumes greater than 0.5 mL are used, the close proximity of the lumbar lateral and intermediate branch to the medial branch potentially might increase false-positive rates by blocking paraspinal soft tissues (ligaments or muscles or both).20,94 In addition, volumes greater than 0.5 mL on the superior edge of the lumbar transverse process may spread onto the dorsal and ventral spinal nerves.88 Decreasing input into the central nervous system by anesthetizing any structure or nerve could relieve pain by decreasing or modulating central input. Although this is a probable confounding factor, the reference typically cited is the study by North and colleagues,95 which reported an unacceptably high false-positive rate for diagnostic blocks in patients with low back pain. The conclusion reached by North and colleagues95 was that diagnostic blocks had limited specificity. Their protocol clearly lacked diagnostic specificity, however. They used an excessive 3 mL volume of bupivacaine for the medial branch blocks. Because 0.5 mL of local anesthetic placed too close to the superior edge flows onto the exiting root, the reported decrease in sciatic pain was more likely due to anesthetizing the spinal nerve and not a false-positive effect of neuromodulation.88
Because patients in the study by North and colleagues95 reported an average relief of 75% to 80% after anesthetizing the sciatic nerve, operators must be aware that blocking this nerve anywhere along its course may result in the report of pain relief. As previously mentioned, relief of pain for the duration of the local anesthetic effect cannot distinguish between reversible inflammatory or compressive causes of pain and nonreversible neuropathic causes of pain.
Although North and colleagues95 found that 3 mL of local anesthetic placed into muscles at several levels has relatively minimal effect on sciatic pain, some authors question whether anesthetizing the needle track increases false-positive responses.20 Patients probably report more pain relief when the needle track is anesthetized. Rather than a false-positive response, one would expect better pain relief when patients are not experiencing lingering needle-related pain at the same time as pain relief resulting from anesthetizing the zygapophyseal joints.
Lumbar Spine: Facet Syndrome
History
In 1911, Goldthwait96 reported that facet joint asymmetry could cause lumbago, sciatica, and paraplegia. Ghormley97 first coined the term facet syndrome as a cause of referred pain and the sciatica resulting from direct nerve root compression by the facet. Badgley97a first described the facet joint as an independent source of referred pain in greater detail. Mooney and Robertson80 described “facet syndrome” referral patterns by injection of hypertonic saline into the lumbar facets of patients with positive diagnostic blocks. Subsequently, Mooney and Robertson80 were the first to use x-ray–guided intra-articular injections with local anesthetic and corticosteroid; they reported complete pain relief in approximately one fifth of patients presenting with low back and leg pain. Dreyfuss and colleagues88 were the first to describe an effective lumbar medial branch block technique. Using this technique, Kaplan and colleagues87 showed that pain resulting from facet capsular distention could be successfully blocked in approximately 90% of cases by a medial branch block with 2% lidocaine versus saline.
Lumbar Zygapophyseal Joint Pain
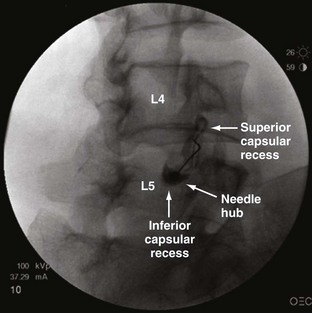
Studies reporting the prevalence of zygapophyseal joint pain report figures ranging from 15% to 52%. In 1994, Schwarzer and colleagues98 established the prevalence of zygapophyseal joint pain using a double block comparative protocol in 96 patients with a mean age of 38 years and mean duration of low back pain of 16 months mostly secondary to work-related injuries and trauma presenting to two tertiary U.S. clinics. (Fig. 15–4 shows a lumbar intra-articular zygapophyseal joint block.) Schwarzer and colleagues98 found that the combination of discogenic pain and zygapophyseal joint pain is uncommon. In a group of 176 patients, 47% had initial relief with a screening lidocaine block, but only 15% had 50% or greater relief with a confirmatory block.
Manchikanti and colleagues,99 also using a double block protocol but requiring 75% pain relief and a differential response, reported an even higher initial response of 81 of 120 (67.5%) to lidocaine medial branch blocks and a much greater percentage (45%) of the total reporting longer 75% relief after confirmatory bupivacaine medial branch blocks. This patient group was older, however, than Schwarzer’s group with a mean age of 47 years and with a longer mean duration of low back pain of 47 months. The false-positive rate for one block was 41%. In a later study, Manchikanti and colleagues100 revised the prevalence of zygapophyseal joint pain downward from 45% to 27% (95% confidence interval 22% to 32%). Schwarzer and colleagues101 studied an older group of patients with a mean age of 57 years referred to an Australian rheumatology clinic with low back pain for an average of 7 years. A diagnosis of zygapophyseal joint pain was made in 40% (95% confidence interval 27% to 53%). Requiring 90% relief of original pain, the prevalence was 32%, and requiring 100% relief, the prevalence was 11%. Manchikanti and colleagues100 reported an even higher prevalence of 52% zygapophyseal joint pain in a group of patients 65 years old or older.
No consistent history, physical examination, or imaging findings correlated to positive block responses have been found. In the early 1980s, uncontrolled single, variable injectant volume, intra-articular zygapophyseal joint injections were used as the reference standard for identifying lumbar zygapophyseal joint pain, and these authors reported correlations with various history or physical examination findings.51,102 Some studies103,104 reported that a cluster of five of seven features (Revel criteria) could predict a 75% decrease in pain after a single intra-articular block. The seven items in the cluster are age older than 65 years, pain well relieved by recumbency, no exacerbation of pain with coughing and sneezing, no exacerbation of pain with forward flexion, no exacerbation of pain with extension, no exacerbation of pain with rising from flexion, and no exacerbation of pain with the extension-rotation test. Subsequent well-conducted studies did not replicate these studies.28,105 As mentioned, most of these earlier studies used single medial branch blocks, which have been reported to have 25% and 38% false-positive rates for the diagnosis of zygapophyseal joint pain.106,107
Newer studies of clinical correlations refined the technique with an appropriate injectant volume and a confirmatory double block paradigm with either a second intra-articular injection or a medial branch confirmatory injection with bupivacaine lasting longer than the pain relief after a prior lidocaine block.28,92,101,106,108,109 These studies did not find any clinical correlates with history or physical examination. In particular, extension and rotation were not predictive of response. A systematic review of all published studies comparing clinical outcome after local anesthetic blocks and clinical signs and symptoms found no consistent clinical features with a high specificity.11 The review found several clinical features with a high sensitivity, however, and these features may be cautiously used to exclude the diagnosis of facet mediated pain. These features include pain not increased with cough, pain not relieved with recumbency, and pain that can be centralized.11 There are no consistent reproducible history or physical examination criteria that predict a positive response to a facet block. History and physical examination are better at ruling out facet mediated pain than diagnosing facet pain.
The current best evidence also shows that radiologic imaging, with a few more recent exceptions, does not correlate with response to zygapophyseal joint blocks. The conflicting evidence that radiologic imaging may predict outcome from uncontrolled lumbar zygapophyseal joint blocks may be partially due to lack of rigor in the reference standard used to define a positive response in earlier studies.20 In 1979, Carrera110 reported that 73% (n = 63) of patients describing pain relief after uncontrolled intra-articular injection of 2 to 4 mL of local anesthetic had CT evidence of lumbar facet disease versus 13% who had no evidence of disease. It is well accepted, however, that injectant volume should not exceed 1 mL; otherwise, the injection loses specificity, with a leak of local anesthetic around the nerve root and along vertebral levels within the epidural space.92
A large study by Jackson and colleagues111 of 390 patients found no relationship between imaging and pain relief after uncontrolled intra-articular lumbar zygapophyseal joint injections. Supporting the findings by Jackson and colleagues,111 Schwarzer and colleagues,112 in the only study using placebo-controlled injection, found no correlation between CT findings and a positive response comparing local anesthetic with saline blocks in 63 patients when more stringent criteria of controlled injections were used as the reference standard. Similarly, Cohen and colleagues113 found no relationship in 192 patients between MRI findings of zygapophyseal joint hypertrophy or degeneration and response to medial branch neurotomies based on positive response to a single medial branch block. Kawaguchi and colleagues114 likewise found no significant relationship between low back pain symptoms and radiographic abnormalities in a group of 106 patients with rheumatoid arthritis.
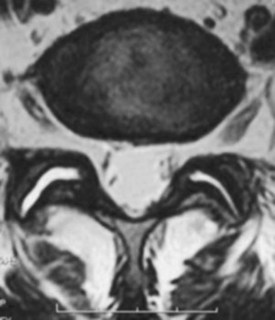
The intriguing bright spot on the horizon is the finding that where MRI or single photon emission computed tomography (SPECT) shows imaging findings consistent with either “inflammation” or “edema,” a stronger correlation emerges (Fig. 15–5). Although not confirming the diagnosis of zygapophyseal joint pain with a reference standard, Friedrich and colleagues115 more recently found that an estimated 14% (21 of 145) of patients with low back pain had MRI evidence of facet joint edema, and follow-up MRI scan showed “almost perfect” agreement between change in pain and a reduction in intensity of edema on sagittal short tau inversion recovery (STIR) images. Radionuclide bone scintigraphy detects bone areas with synovial changes (inflammation or hyperemia) or increased osteoblast activity and degenerative regions with a high degree of remodeling. Osteophytes in process of growing show a high degree of bone scan activity. As mentioned earlier, a positive lumbar SPECT scan predicts a statistically significant reduction in pain after facet blocks.31
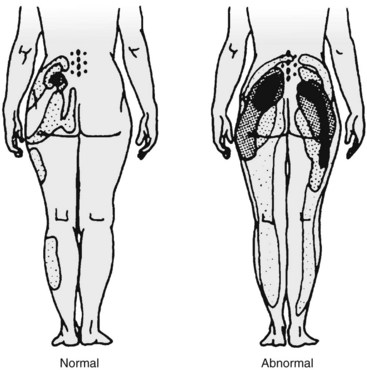
Zygapophyseal Joint Pain Referral Maps
Pain referral patterns have been studied using stimulation of patients during provocative diagnostic injections116 by injection of hypertonic solutions into normal and abnormal subjects80 or by electrical stimulation of medial branches.80,117 Most studies showed distinct but overlapping referral areas; it is likely that the pain referral patterns obtained in normal volunteers are smaller because of less sensitization. There are also limits to the referral maps; Mooney and Robertson80 reported on lumbar facet referral maps in normal volunteers and subjects with a positive diagnostic facet block (Fig. 15–6). Under fluoroscopic guidance, they injected contrast dye (unspecified volume) followed by 3 to 5 mL of hypertonic saline. Some of the distal extremity pain seen in the diagrams may be due to excessive volume of saline with irritation of the sciatic nerve roots. Given the lack of sensitivity and specificity of history, physical examination, and imaging and until more research is performed with finite injectant volumes (in patients with confirmed dual positive blocks), these referral maps can be used as a starting point to guide selection of levels to be injected.
Predictive Value
Historically, lacking robust studies, guideline and systematic review articles have been relegated to quoting studies with methodologic flaws as implied evidence that one need not diagnose facet mediated pain before surgery.22,94 There is no reason that a variable amount of relief after uncontrolled, variable volume, intra-articular zygapophyseal joint blocks should predict fusion outcomes using surgical fusion techniques from the 1980s in a group of patients being operated on for various unknown or unstated reasons. Jackson118 correlated relief after spinal fusion in 36 patients from 1980-1988 to results of a single intra-articular facet injection with 1.5 mL of local anesthetic and an unknown volume of contrast dye. Of patients, 85% had “some improvement” with an average relief after injection of 29%. The authors found no relationship between fusion surgery performed for unstated reasons and a “favorable response” to facet injection. The surgeries were presumably performed not because the authors believed the patients’ symptoms were due to their zygapophyseal joints. The surgical results based on their “mean pain and functional assessment scores” also seemed to improve by significantly less than 50%, suggesting poor patient selection.
An important historical study, published by Esses and Moro in 1993,119 is often quoted to refute the therapeutic utility of zygapophyseal joint blocks; however, it warrants a careful, critical review. Esses and Moro119 concluded that single intra-articular diagnostic facet joint injections “should not be used in determining treatment because they are not predictive of either surgical or nonsurgical success.” This study had significant methodologic shortcomings, which limit the validity of the authors’ conclusions. First, the study was retrospective with patients surveyed by telephone approximately 5 years after surgery. Second, 1.5 mL of local anesthetic was injected into the facets, and no mention is made of the volume of contrast dye needed to confirm needle position; the injections likely were nonspecific because of facet capsule rupture from excessive volume (>1 mL). Third, the patient population was markedly heterogeneous with significant confounding factors: an average duration of back pain of 8 years and approximately 40% of patients with a history of prior surgeries, including failed fusions. More than 50% of patients underwent three-level, four-level, or five-level fusions, which are known to have a poorer outcome than single-level or two-level fusions.
Fourth, of the 82 patients who underwent surgery, 36 (44%) had 0% relief from facet injections. Almost one half of the patients undergoing surgery had no relief from diagnostic blocks. Eight of 19 (42%) of the patients with complete relief after facet injections declined surgery, leaving only 11 of 82 (13%) patients who underwent surgery who had 100% relief from facet blocks. The remaining 35 of 82 patients (43%) had “partial but significant relief” (the exact percentage relief is not reported). Fifth, 30 of 82 (37%) patients had prior surgeries (laminectomy, discectomy, and fusion). It is well known that patients with failed back surgery syndrome often fare poorly with repeat surgery. Also, during the 1980s, diagnosis of the etiology of failed back surgery syndrome was elusive and might not be corrected by a posterior arthrodesis. For failed back surgery syndrome, facet joint pain comprises only 3% of cases; the most common diagnoses are foraminal stenosis (25% to 29%), painful disc (20% to 22%), pseudarthrosis (14%), neuropathic pain (10%), recurrent disc herniation (7% to 12%), and sacroiliac joint pain (2%).120
Next, Esses and Moro119 did not match the surgery to specific facet levels blocked. Patients had either one-level or two-level facet blocks, yet the following posterior fusions were performed: 20, single-level; 3, two-level; 10, three-level; 4, four-level; and 12, five-level or greater, including thoracic spine (wherein facets were never blocked). Finally, significant questions arise regarding the efficacy of the surgical intervention because there was no significant difference between surgical and nonsurgical outcomes. As reported, only approximately one third of patients in either the surgical or the nonsurgical group had a good outcome. Because of methodologic flaws and limitations of the Esses and Moro study,119 facet intra-articular injections cannot be impugned as either predictive or nonpredictive of surgical success.
In another observational study, Lovely and Rastogi121 required a “positive response” to intra-articular injection of greater than 70% relief after bupivacaine facet block for 6 hours and required a confirmatory response on two subsequent injections. Of 28 patients, 23 had a good to excellent outcome after fusion surgery; however, large volumes of 3 to 5 mL were used during the blocks, making interpretation difficult. At present (2008), there is no research regarding the utility of cervical or thoracic facet blocks as presurgical screening tests.
By comparison, when a specific treatment is directed at a cause of pain originating from the zygapophyseal joint, accurate diagnostic testing does matter. In a more recent study, researchers reported that when a putative inflammatory cause of lumbar facet pain was confirmed using a positive SPECT scan, a positive response (a significant reduction in pain) was clearly predicted with intra-articular and pericapsular steroids at 1 and 3 months compared with subjects with negative scans or routine care.31
In regard to the therapeutic utility of double, controlled differential facet blocks, there is a clear and direct relationship between relief of pain after controlled medial branch blocks with a well-validated treatment for zygapophyseal joint pain, medial branch neurotomies. In a study by Dreyfuss and colleagues,122 patients who obtained greater than or equal to 80% relief from medial branch blocks were selected to undergo lumbar radiofrequency neurotomy. At 12 months, 60% of the patients obtained at least 90% relief of pain, and 87% obtained at least 60% relief. Dreyfuss and colleagues122 concluded that lumbar medial branch neurotomy is an effective means of reducing pain in patients carefully selected on the basis of controlled diagnostic blocks. The most recent, high-quality study available on radiofrequency is a randomized controlled trial evaluating radiofrequency neurotomy in patients with chronic low back pain.123 The trial used three positive blocks in the inclusion criteria and a “sham radiofrequency” procedure for comparison; statistically significant reduction in pain and improvement in various quality of life variables were obtained. In another study, when the diagnosis is confirmed by relief of pain for greater than 3 months after medial branch neurotomies, repeat neurotomies are successful in greater than 75% in lumbar and cervical spine.124,125
Cervical Spine Facet Syndrome
History
The cervical facet joints are known to be sources of neck and extremity pain and headache. In 1940, Hadden126 described pain from zygapophyseal joints causing headache. In the 1970s, Macnab127 described pain arising from the facet joints after whiplash injury. Bogduk and Marsland128 devised a technique to block the third occipital nerve, which relieved neck pain and headache stemming from the C2-3 facet joint in 70% of patients. Headache arising from C0-1 or C1-2 joints has also been described.129,130 Bogduk and Marsland131 were also the first to describe medial branch blocks for all cervical spine levels. They studied patients presenting with idiopathic neck pain and reported that medial branch block and intra-articular blocks provided complete, temporary relief of pain for 70% of patients.
Cervical Zygapophyseal Joint Pain
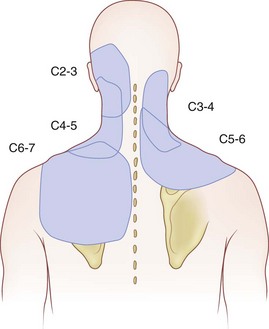
Based on the confirmatory block paradigm, the cervical facet joints are a common source of chronic neck pain; the prevalence of cervical facet syndrome is greater than the prevalence of lumbar facet syndrome. Cervical discogenic pain shares referral patterns with facet pain, but it is far less common.132 Based on comparative blocks of cervical facet joints causing chronic neck pain with either associated headache or shoulder pain, the C2-3 (36%) and C5-6 facet joints (35%) were the most common pain generators.133 After whiplash injury, Level I prospective clinical studies provide evidence that facet joints are the most common source of chronic pain.134,135 Cervicogenic headache stemming from the C2-3 facet after whiplash has a 53% prevalence.134
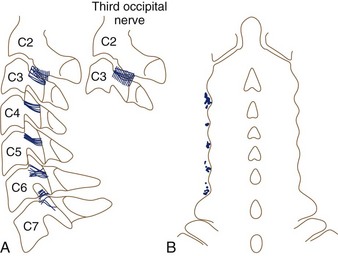
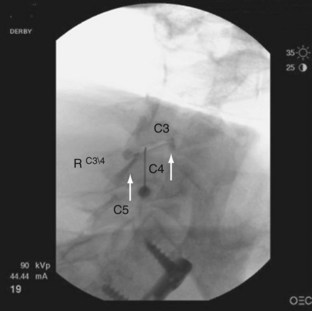
Often neglected are C0-1 and C1-2 joints in evaluation of upper neck pain and headache. Dreyfuss and colleagues129 studied the referral patterns for the atlantoaxial and lateral atlantoaxial joints. In 2002, Aprill and colleagues136 failed to confirm the null hypothesis that lateral atlantoaxial joints are not a common source of occipital headache. These investigators found that of 34 patients presenting with symptoms and signs of atlantoaxial joint pain, 21 obtained complete relief of headache after diagnostic injection of local anesthetic. Pain referral patterns have been defined in C2-3 through C7-T1 facets (Fig. 15–7).15 Innervation of the cervical facet joints is well described (Fig. 15–8).15 The cervical zygapophyseal joints can be blocked either by medial branch blocks or with intra-articular injections (Fig. 15–9).
Prevalence rates for pain originating from cervical facets range from 36% to 60%. The false-positive rate for a single, uncontrolled block is 27% (95% confidence interval 15% to 38%).137 The following prevalence rates (mean [95% confidence interval]) are reported from studies using either a double block or a triple block paradigm (normal saline as a placebo): 54% (40% to 68%),134 36% (27% to 45%),138 60% (33% to 64%),135 and 60% (50% to 70%).139 Manchikanti and colleagues100 restudied the prevalence of cervical zygapophyseal joint pain in a larger group of patients and found a similar 55% (95% confidence interval 49% to 61%) prevalence. The most recent study by Manchikanti’s group in 2007,83 of 438 patients requiring 80% relief of pain for 2 hours’ duration with lidocaine and 3 hours’ duration with bupivacaine, reported a prevalence of 39%. Corroborating the high prevalence of cervical zygapophyseal joint pain, Yin and Bogduk139a in a private practice clinic audit found a 55% prevalence of cervical zygapophyseal joint pain using a strict double comparative block protocol.
Similar to lumbar zygapophyseal joint pain, there are no high-quality studies showing a particular set of clinical features that can predict results of diagnostic cervical facet or medial branch blocks.140 With diagnosis by medial branch blocks, one exceptionally skilled manipulative therapist was able to identify all 15 subjects with diagnostic block–proven symptomatic zygapophyseal joints and specify the correct symptomatic segment. None of the five patients with asymptomatic joints was misdiagnosed as having symptomatic zygapophyseal joints.141 A later follow-up study by the same group failed to confirm the apparent high specificity and sensitivity, however, and reported a high sensitivity but low specificity and concluded that manual examination of the cervical spine lacks validity for the diagnosis of cervical zygapophyseal joint pain. In the study by Aprill and colleagues136 of C1-2 facet pain as a source of occipital headache, only 60% of the patients shared clinical criteria that predicted a positive response to the block.
Advanced imaging has not been correlated with positive responses to diagnostic blocks. Hechelhammer and colleagues142 found no relationship between short-term pain relief after cervical intra-articular and pericapsular injection of local anesthetic and corticosteroid and the degree of osteoarthritis graded on a CT scan.
Thoracic Spine
The prevalence of patients who complain of chronic upper back or mid-back pain ranges from 3% to 22%.30,143,144 One survey study of 35- to 45-year-olds estimated the prevalence of thoracic pain to be 15%.145 Thoracic zygapophyseal joint pain referral patterns have been reported (Fig. 15–10).146,147 Thoracic medial branch anatomy has also been described (Fig. 15–11).148
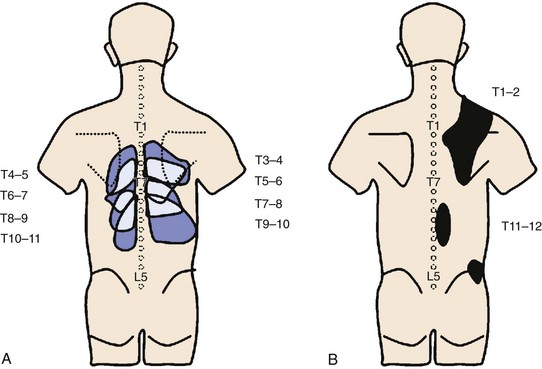
FIGURE 15–10 Maps of referred pain patterns in segments indicated. A, Based on Dreyfuss et al146 in normal volunteers. B, Based on Fukui et al147 in patients with single positive facet block.
(From Bogduk N [ed]: Practice Guidelines for Spinal Diagnostic and Treatment Procedures. San Francisco, International Spine Intervention Society, 2004.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree