Tailor’s Bunion Deformity
Sean Patrick Dunn
Jane Pontious
Tailor’s bunion, sometimes called the bunionette, is an often painful condition affecting the lateral aspect of the fifth metatarsal head. Painful symptoms often occur due to the constricting shoe gear more commonly worn by women. In some instances, an inflammatory bursa can form.
The name, tailor’s bunion, was derived from tailors who sat in a crossed-legged fashion on the floor when performing their work with resultant pressure on the lateral side of the forefoot, particularly the fifth metatarsal head.
ETIOLOGY
The reported etiology of the tailor’s bunion has varied greatly over the past 60 years. While it is evident that there is not a specific cause of tailor’s bunions, the etiology may be split into two broad categories, structural and biomechanical.
The structural causes of the tailor’s bunion deformity range from embryonic splaying of the fifth metatarsal to a supernumerary bone lateral to the fourth metatarsal head (1,2 and 3). Some authors contend that the wide intermetatarsal angle between metatarsals 4 and 5 is the true cause, while others attribute the symptoms to the shape of the fifth metatarsal head (3,4,5,6,7,8,9 and 10).
The biomechanical causes of the tailor’s bunion deformity are equally varied. Rotation of the fifth metatarsal occurs with pronation resulting in a lateral bowing. There is also a plantar grade displacement of the abductor digiti quinti muscle. This causes an altered axis of muscle pull, leading to adductovarus rotation of the fifth toe. The retrograde pressure of the digit increases the intermetatarsal angle (11,12,13 and 14).
CLINICAL PRESENTATION
The patient who presents with a symptomatic tailor’s bunion deformity will most often have pain dorsolaterally, laterally, and/or plantar to the fifth metatarsal head, which is prominent. An inflammatory bursa may be present.
There may be a secondary callus over the prominence. This hyperkeratotic lesion is most commonly located laterally, followed by plantar, then by the combination of plantar and lateral lesions (7). A heloma molle may be present between the fourth and fifth toes. The fifth toe is often in an adductovarus position (15). There may be a hyperkeratotic lesion overlying the proximal interphalangeal joint or distally in the digit lateral to the nail border (Lister’s corn). The reported sex predominance ranges from 1:1 to 5.7:1 female to male, with presentation for treatment occurring most often in the fourth to fifth decades of life (6,14,15,16,17,18 and 19).
RADIOGRAPHIC PRESENTATION
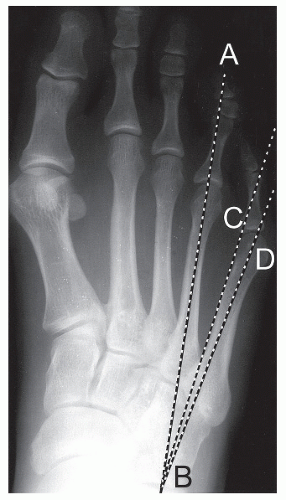
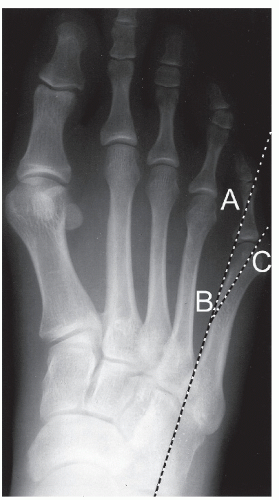
Standard dorsoplantar and lateral weight-bearing radiographs should be obtained. Medial oblique and lateral oblique views may be obtained to evaluate the plantar lateral and plantar medial condyles, respectively. The average intermetatarsal angle (IMA) between metatarsals four and five (IM4) in normal patients has been reported to be 6.4 to 9.1 degrees and 8.7 to 10.8 degrees in symptomatic bunionettes (19,20,21,22 and 23). The traditional method to calculate this angle is to measure the medial proximal portion of the fifth metatarsal shaft in respect to the bisection of the fourth metatarsal, as described by Fallat and Buckholz (22) (Fig. 23.1).
Fallat and Buckholz also recognized that the lateral bowing angle is a significant cause of tailor’s bunions and developed a method with which to measure it. This method involves a bisection of the articular surface of the head and a bisection of the neck of the fifth metatarsal. A line drawn from these bisections will intersect the line drawn parallel to the proximal medial portion of the fifth metatarsal. They determined this angle was normally 2.64 degrees, with a range of 0 to 7 degrees. In the presence of a bunionette deformity, this angle increased to an average of 8.05 degrees (22) (Fig. 23.2).
Nestor also measured the fifth metatarsophalangeal joint (MTPJ) deviation angle by determining the angle formed by the bisection of the fifth metatarsal and the proximal phalanx. They determined this angle was 10.2 degrees varus in normal feet and 16.6 degrees varus in symptomatic feet with tailor’s bunions (19). Coughlin (23) reported that his average MTPJ angle was 16 degrees in his preoperative tailor’s bunion patients. This value was reduced to 0.5 degrees postoperatively.
Crawford described a method to determine where the apex of the deformity is located within the fifth metatarsal. A bisection of the fifth metatarsal base and the fifth metatarsal head is drawn. Next a line is drawn perpendicular to the bisections. The site where the lines meet indicates the point of greatest deformity of the fifth metatarsal (24).
In their paper in 1980, Fallat and Buckholz (22) proposed six different pathoanatomical types of tailor’s bunions. These were:
Rotation of the lateral plantar tubercle into a lateral position
An increased IM angle
An increased lateral deviation angle
A large round dumbbell-shaped fifth metatarsal head
Arthritic changes with exostosis formation at the fifth MTPJ
Any combination of the above conditions, with the first three being the most common
Coughlin (23) also proposed a classification system based on weight-bearing radiographic findings. He described three types defined as: (a) large head, (b) metaphyseal-diaphyseal flare or deviation, (c) enlarged 4 to 5 intermetatarsal angle.
SURGICAL TECHNIQUE
The patient is placed supine on the operating table with a bump under the ipsilateral hip. A longitudinal dorsolateral incision is made through the skin (Fig. 23.3A). The incision is deepened through the subcutaneous tissue to the level of the deep fascia. An incision is then made in line with the skin incision directly onto the fifth metatarsal through the deep fascia, periosteum, and dorsal capsule (Fig. 23.3B). Dissection is continued subperiosteally with a Freer elevator beginning on the fifth metatarsal shaft, where the periosteum is less firmly adhered to the bone (Fig. 23.3C). A scalpel is used to reflect capsule from the metatarsal head. If an osteotomy is to be performed, care must be taken to only reflect enough periosteal tissue to ensure adequate space to perform the bone cut and allow for the shifting of the fragment. If too much periosteum is reflected, delayed healing may result. Alternatively, an osteotomy can be performed through intact periosteum with none reflected.
In a manner analogous to a bunionectomy, the lateral prominence is then resected parallel to the lateral border of the foot (Fig. 23.3D). Care should be exercised not to remove an excessive amount of bone, as fifth MTPJ subluxation may occur postoperatively. An alternative method is to perform the removal of the lateral prominence after the desired osteotomy is performed. This will ensure adequate bone stock to perform an osteotomy. The desired osteotomy and fixation are then performed (Fig. 23.3E and F). Fixation is based on surgeon’s preference and is selected based on inherent stability of the osteotomy and postoperative management. If an exostectomy is not performed, the fifth metatarsal phalangeal joint capsule may be left intact, minimizing postoperative fibrosis of the joint. Layered closure is performed with absorbable suture and a compressive dressing is applied.
Although certain radiographic and clinical criteria are described, these are not to be looked at as absolute, but only as guidelines. The final procedural choice is based upon the surgeon’s experience and what procedure is in the patient’s best interest.
CONDYLECTOMY
This procedure is indicated when the patient’s main concern is bump pain with or without a radiographically significant IM angle, though the procedure is more effective with smaller splaying of the metatarsals. The condylectomy procedure is accomplished by resecting the lateral one-fourth to one-third of the metatarsal head using a power saw or osteotome. Postoperative care includes weight-bearing in a surgical shoe, then transitioning into a soft shoe with a wide toe-box, to patient tolerance.
METATARSAL HEAD RESECTIONS
It is generally indicated in a severe tailor’s bunion that would need a significant osteotomy for correction. The metatarsal head resection can also be a valuable procedure in the
treatment of recurrent lateral or plantar ulcerations in diabetic patients. In 1977, Addante proposed the resection of the fifth metatarsal head with insertion of a Silastic sphere as a spacer. The size of the sphere was determined based on preoperative radiographs. The resection of the fifth metatarsal head was performed from dorsal-distal-lateral to plantar-proximal-medial, which the authors claimed “helped to position the sphere in a ball and socket fashion” (24). Transfer lesions from this procedure are surprisingly uncommon.
treatment of recurrent lateral or plantar ulcerations in diabetic patients. In 1977, Addante proposed the resection of the fifth metatarsal head with insertion of a Silastic sphere as a spacer. The size of the sphere was determined based on preoperative radiographs. The resection of the fifth metatarsal head was performed from dorsal-distal-lateral to plantar-proximal-medial, which the authors claimed “helped to position the sphere in a ball and socket fashion” (24). Transfer lesions from this procedure are surprisingly uncommon.
Generally, the metatarsal head is resected at the junction of the metatarsal head and neck (Figs. 23.4 and 23.5). The postoperative care of the metatarsal head resection is identical to the condylectomy.
DISTAL OSTEOTOMIES
Distal osteotomies are characterized by beginning the osteotomy within the metaphyseal-diaphyseal junction. This placement is beneficial because of the predominance of cancellous bone in this anatomical location. Due to the bone architecture, these osteotomies are at a decreased risk of delayed and/or
nonunion owing to the increased blood supply at this location. There have been numerous procedures described in the distal aspect of the fifth metatarsal. Many of these procedures are analogous to the procedures that are performed in the first metatarsal in the correction of a bunion deformity (Figs. 23.4,23.5,23.6,23.7,23.8 and 23.9) (25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50 and 51).
nonunion owing to the increased blood supply at this location. There have been numerous procedures described in the distal aspect of the fifth metatarsal. Many of these procedures are analogous to the procedures that are performed in the first metatarsal in the correction of a bunion deformity (Figs. 23.4,23.5,23.6,23.7,23.8 and 23.9) (25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50 and 51).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree