Fig. 1
Typical deformity of severe Perthes disease with a mushroom deformity and an area of central necrosis. Frequently, the deformity in the medial to lateral plane is greater than the deformity in the anterior to posterior plane. The planned osteotomies are shown by the dotted lines. The blood supply to the mobile fragment is maintained by retinacular terminal branches of the medial femoral circumflex artery
The following section describes the technique for femoral head reduction osteotomy in a skeletally immature patient with LCPD (Fig. 2). There is a tremendous learning curve for such a procedure and the authors advise against performing this procedure for surgeons early in their practice of hip surgery.
Fig. 2
The final construct after completion of the femoral head reduction osteotomy. The mobile and stable fragments are joined with headless compression screws. The trochanter is advanced distally and a relative neck lengthening is achieved by resecting excess bone to recontour the superior femoral neck while carefully preserving the blood supply in the retinacular flap
Patient Selection
Patient selection is extremely important for this osteotomy and compliance is important as well.
Indications
Healed LCPD hip . This procedure should not be performed in active stage of the disease.
Central head necrosis with well-maintained articular cartilage over the rest of the femoral head. Oblong femoral head with greater medial-lateral diameter than anteroposterior diameter is ideal for this procedure.
Acetabular cartilage damage must be absent or minimal for optimal results.
Full strength should be present in major muscle groups about the hip. The procedure is not a good option for patients with neuromuscular disease conditions that cause weakness.
Patient is toe-touch weight bearing for about 10–12 weeks and compliance is paramount and should be discussed preoperatively with the patient and caregivers.
Relative Contraindications
Advanced articular degeneration of the femoral head or acetabulum
Extremely misshapen femoral head not amenable to any symmetric head reduction osteotomy
Noncompliant patient
Extreme obesity
Neuromuscular disease etiology for hip instability, subluxation, and deformity
Preoperative Imaging
Full-length standing alignment radiographs of the lower extremities
MR arthrogram with radial neck sequencing to study the cartilage and labral status in detail, as well as to rule out changes of AVN preoperatively (Fig. 5)
CT with 3D reconstruction to analyze the complete nature of the femoral head shape for purposes of planning of the osteotomy

Fig. 3
Legg-Calvé-Perthes disease of the right hip in a 13-year-old male. Lateral pillar classification C and has several “head at risk” signs including lateral calcification, Gage’s sign, and head extrusion

Fig. 4
Frog lateral radiograph of LCP hip with mushroom deformity
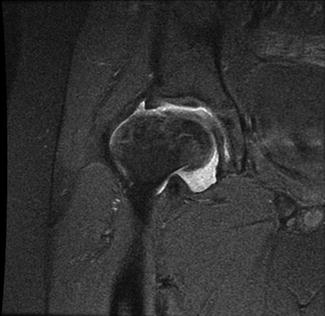
Fig. 5
Coronal MR image of LCP hip demonstrating maintained vascularity to medial portion of epiphysis
Procedure
Room and Equipment Setup
Neuromonitoring is preferred for this operation since the hip stays dislocated for a longer period in this case as compared to a safe surgical dislocation for a routine case of FAI. The leads on the opposite leg are placed prior to prepping and on the operative leg are placed in a sterile manner.
Fluoroscopic examination may be valuable in the placement of the trochanteric fixation at the conclusion of the procedure, but is not required as the remainder of the procedure is completed under direct visualization.
In cases when the procedure is being performed with a concomitant acetabular osteotomy, a cell-saver may be valuable.
Patient Positioning
Patient is positioned in a lateral decubitus position. Additionally, the procedure can be carried out on a regular table or radiolucent flat-top table. The use of a radiolucent flat-top table offers the advantage of easier and faster setup, ease of imaging, and the potential for multiple surgeries to be performed simultaneously (e.g., concomitant proximal femoral osteotomy and acetabular osteotomy in complex cases).
Standard hip positioners for lateral positioning are preferred over a beanbag to allow free manipulation of the operative limb. Commercial hip positioners more securely stabilize the pelvis than a beanbag in preparation for surgical hip dislocation.
The entire limb is then prepped in a standard fashion from the iliac crest to the toes. Neuromonitoring wires are placed in a sterile manner and baseline readings are obtained.
A 15 cm incision is obtained centered over the trochanter and curving a bit anteriorly in the proximal part. After superficial dissection, the tensor fascia lata is split in the line of the mid-trochanter (distal to trochanteric tip) and along the mid-femur in the distal part of the incision. Proximally it is split in line with the zone between tensor fascia lata and gluteus maximus fascia.
The anterior and posterior margins of the trochanter are palpated and care is taken to protect the posterior vessels. A trochanteric flip osteotomy is now performed taking care to keep the gluteus medius, gluteus minimus, and vastus lateralis attached to the greater trochanteric fragment. Gluteus minimus tendon is released from its insertion over the trochanter and the trochanteric osteotomy is flipped anteriorly with the digastric attachment.
A “z” capsulotomy (right hip) is now performed as the standard technique of safe hip dislocation and the femoral head is dislocated anterosuperiorly with adduction and external rotation. The ligamentum teres (which is almost always hypertrophied in these cases) is divided to facilitate a gentle dislocation.
The femoral head is carefully examined and using the head-sizing jigs, the central femoral osteotomy is outlined (Fig. 6).
The “soft spot” with the retinacular vessels is carefully protected in the superior fragment. The central fragment with the necrotic area of femoral head, in the saddle-shaped area, is now completely osteotomized with two osteotomies made parallel to the neck (Fig. 7).
The deformed femoral head is usually saddle shaped on the surface and an ellipse in its circumference with the medial-lateral dimension larger than the anteroposterior dimension. Determination of the correct wedge resection is a combination of geometric resection and direct visualization. The goal is to restore the long-axis measure to as close to the shorter anteroposterior width (with a 10 % maximum difference between the medial-lateral and anteroposterior widths). For example, if the width is 5.5 cm and the long axis is 7.5 cm, the wedge should be at least 1.5 cm to bring the length to 6 cm and have an approximate 10 % maximum difference. In our experience, all osteotomy resections have included the fovea or the attachment of the ligamentum teres.
The intraoperative templates (head sizers) are invaluable in determining the sphericity as determination of the adequacy of the resection by direct visualization obviously comes with experience.
The initial superior osteotomy is made with an oscillating saw and finished with an osteotome to prevent damage to the posterior retinacular vessels. This creates the superior mobile fragment with blood supplied by the posterior retinacular vessels [4].
The second osteotomy is inferior to the initial cut and is made in similar fashion to above. This creates the stable fragment which is still in continuity with the metaphysis and blood supply is provided by a constant posteromedial branch of the medial femoral circumflex artery that travels in the ligament of Weitbrecht [4].
The superior (mobile) fragment with the attached retinacular blood vessels is now approximated to the inferior (stable) fragment and contour matched. Three or four headless cannulated screws are placed to achieve compression. The overhang (should be minimal) is carefully shaved off (Fig. 8).
Femoral head-neck osteochondroplasty is performed in the anterior zone as necessary (between 12 and 6 o’ clock).
Acetabulum is inspected and labral pathology is treated, if present. Concomitant acetabular osteotomy, if required, is performed at this point (Figs. 9, 10, and 11).
Relative neck lengthening is performed by appropriately distalizing and lateralizing the greater trochanteric fragment to restore the anatomy and proper biomechanics. LCP hips frequently have high trochanters and need to have the trochanter distalized such that the tip of the trochanter is equal with the approximate center of the femoral head. The trochanteric fragment is fixed using two screws (3.5 cortical fully threaded). Wound is closed in layers.
After sterile dressings and a compression wrap are applied, the limb is placed in a knee immobilizer and a small abduction pillow is placed between the legs. Cast immobilization is discouraged for these cases (patients are typically above 12 years of age). Final AP pelvis and lateral radiographs of the affected hip are obtained in the OR prior to transporting the patient to PACU (Figs. 12 and 13).
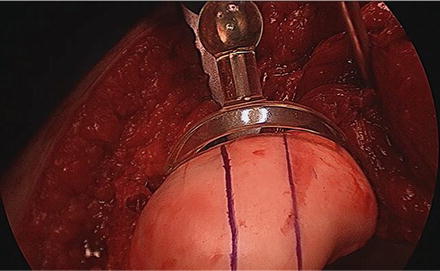
Fig. 6
Intraoperative photograph of femoral head sizing and planning for femoral head reduction osteotomy (FHRO)
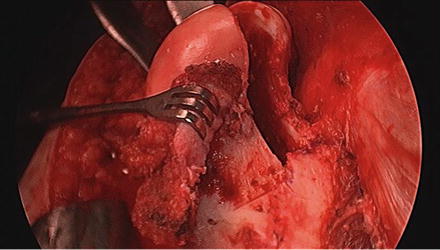
Fig. 7
Clinical photograph of FHRO with superior retinacular flap maintaining perfusion to the mobile, superior segment
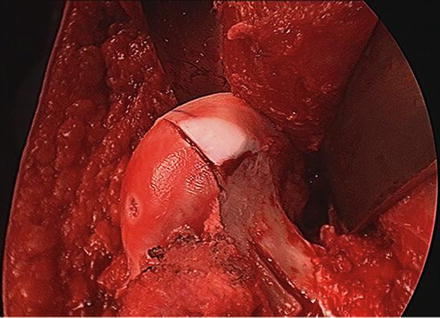
Fig. 8
Clinical photograph of FHRO following resection of central portion and matching of the superior mobile fragment and the inferior stable fragment to create a spherical femoral head
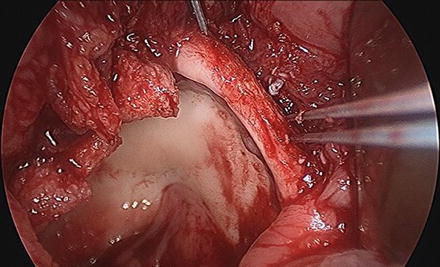
Fig. 9
Clinical photograph of acetabular rim resection and labral reattachment with suture anchors following FHRO
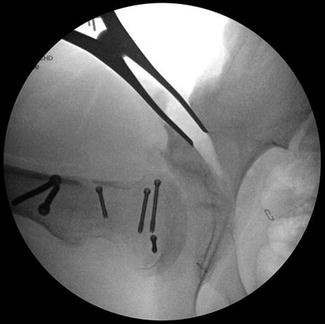
Fig. 10
Intraoperative fluoroscopy demonstrated inadequate acetabular coverage following FHRO. The acetabulum had remodeled to the deformed, mushroom-shaped LCP head and was too capacious following FHRO. A Pemberton pelvic osteotomy was performed to improve congruity of the hip. The authors recommend a volume reducing pelvic osteotomy when combined with a FHRO

Fig. 11
Intraoperative fluoroscopy demonstrating improved lateral hip coverage following Pemberton osteotomy

Fig. 12
Early postoperative radiographs. The FHRO was stabilized with four subchondral compression screws

Fig. 13
Early postoperative radiograph. The trochanteric slide osteotomy was secured with two 4.5 mm cortical screws
Complications
Sectoral avascular necrosis of the femoral head related to damage during dissection or moving the superior fragment.
Nerve palsy due to prolonged position of dislocation.
Distraction at the osteotomy leading to delayed union or nonunion.
The femoral head reduction osteotomy requires a surgical hip dislocation that has its own specific complication profile which may include:
Osteonecrosis
Trochanteric nonunion
Infection/osteomyelitis
Damage to trochanteric physis symptoms/painful hardware
Chondrolysis
Postoperative Care and Rehabilitation
Knee immobilizer for 2 weeks to limit hip flexion from 0 to 40° to limit stress against the capsular repair. Excessive flexion of the hip joint is nearly impossible in the early postoperative period with the knee in extension.
Toe-touch weight bearing for 10–12 weeks with crutches for assistance.
Progressive advancement of weight bearing for the next 4 weeks, followed by weight bearing as tolerated.

Fig. 14
AP hip radiograph 30 months following FHRO and Pemberton pelvic osteotomy demonstrating healed osteotomy with no evidence of avascular necrosis. Patient had returned to sporting activities and underwent trochanteric screw removal due to symptomatic bursitis

Fig. 15
Lateral hip radiograph demonstrating maintained joint space, contained hip, and well-healed pelvic osteotomy
Rehabilitation
Isometric quads and ankle pump exercises starting POD #0
Knee ROM exercises (with extended hip) starting after 3 weeks
Quadriceps strengthening starting at 4 weeks
Hip abductor strengthening to start at 6 weeks
Hamstring and IT band stretching to begin when patient is FWB
Outcomes
Leunig and Ganz reported their results of femoral head reduction osteotomy (FHRO) and relative neck lengthening for severe Legg-Calvé-Perthes (LCP) disease in 14 patients with a minimum follow-up of 3 years. Eight patients had a concomitant periacetabular osteotomy (PAO) procedure. There were no major complications to include osteonecrosis or implant failure. All patients reported improved range of motion and decreased pain; but no validated outcome measurement was obtained [7].
Paley reported on his series of 21 patients who underwent FHRO secondary to a misshapen femoral head from LCP disease, adolescent avascular necrosis (AVN), and hip dysplasia who were followed for a mean of 2.7 years. The average age at surgery was 14 years and indications included pain, positive Trendelenburg sign and gait, and reduced range of motion. All patients achieved union, although one patient sustained a femoral neck fracture during surgery requiring conversion to total hip arthroplasty. Three additional patients have gone on to conversion to total hip arthroplasty. An additional patient underwent osteonecrosis at 18 months post-FHRO. Five patients had residual instability requiring an articulated external fixator for 6 weeks without recurrent hip instability. Overall 66 % (14/21) patients achieved good to excellent outcomes [4].
A recent series by Burien et al. from the Czech Republic describes the use of an anteromedial wedge reduction osteotomy for the treatment of nonspherical femoral head in seven patients with late LCP or multiple epiphyseal dysplasia. The indications were decreased abduction and limp with saddle deformity and extrusion seen on radiographs (all Stulberg class V hips). At a mean follow-up of 17 months, the Harris hip score had improved significantly (55.4 pre-op to 84.8 post-op). No patients sustained osteonecrosis and all improved in their radiographic Stulberg classification [8].
Proximal Femoral Intertrochanteric Osteotomy for Chronic Healed SCFE
Intertrochanteric osteotomies to treat deformities of the proximal femur have been a workhorse operation for the hip surgeon for many decades. For this reason, the long-term outcomes of these procedures are well described in the literature. Advantages of the intertrochanteric osteotomy included reliable healing and low risk of osteonecrosis. One of the disadvantages of the intertrochanteric osteotomy is that it does not address the pathoanatomy directly; therefore, the correction may be incomplete and may also introduce a new deformity to the proximal femur that can complicate revision or conversion to a total hip arthroplasty if required. The FHRO osteotomy for LCP disease or the modified Dunn procedure for severe SCFE can both be easily converted to a THA if avascular necrosis or end-stage degenerative changes develop. Additionally, intertrochanteric osteotomy is not immune from osteonecrosis of the femoral head.
Chronic healed slipped capital femoral epiphysis leads to a complex three-dimensional deformity of the proximal femur [10]. The main deforming components are posterior, medial, and inferior displacement of the femoral head in relation to the femoral neck, relatively short femoral neck, relative coxa vara, trochanteric overriding, and excessive intorsion of the femur (Figs. 16 and 17). There are components of femoroacetabular impingement (FAI) that need to be identified and addressed as well [11].
Fig. 16
Anterior view of the typical femoral deformity in the healed slipped capital femoral epiphysis (SCFE). The femoral metaphysis displaces superiorly and anteriorly which produces a relative displacement of the epiphysis in a medial, inferior, and posterior direction. This produces the combined deformity of coxa vara and a cam lesion that is centered anterosuperiorly
Fig. 17
Lateral view of the typical femoral deformity in the healed slipped capital femoral epiphysis (SCFE). The anterosuperior cam lesion is the product of the healing callus after separation of the epiphysis and metaphysis. The femoral metaphysis displaces anteriorly which produces the relative posterior displacement of the epiphysis
Many hip surgeons recognize the healed SCFE as an impingement lesion and address both impingement and deformity in the same setting. The following section describes a technique for corrective proximal femoral osteotomy while addressing femoroacetabular impingement in a case of chronic healed SCFE.
Very good indications for intertrochanteric osteotomy in the young patient include congenital coxa vara, limited avascular necrosis of the femoral head, femoral neck fracture nonunion , and limb length discrepancy up to 2.5 cm in length. Good indications for intertrochanteric osteotomy include coxa valga with subluxation, chronic SCFE, excessive version in a child, Perthes disease, spastic cerebral palsy, femoral neck fracture, and abduction deficiency after healed acetabular fracture or posttraumatic avascular necrosis. A salvage procedure for osteoarthritis in a young patient is a questionable indication for intertrochanteric [12].
Patient Selection
Indications
Healed SCFE hip. This procedure should not be performed in acute or unstable slipped epiphysis. The authors’ algorithm for acute SCFE is outlined in a previous publication [13].
Coxa vara.
Partial osteonecrosis of the femoral head.
The surgeon should assess the articular cartilage over the femoral head and acetabulum as minimal damage is optimal for results.
Patient is toe-touch weight bearing for about 4–6 weeks and compliance is important.
Other indications for general intertrochanteric osteotomies include coxa valga, coxa vara, avascular necrosis of the femoral head, femoral neck fracture nonunion or malunion, limb length discrepancy, cerebral palsy, version deformity, Perthes disease, and as treatment for osteoarthritis [12]. However, the technique described below is relatively specific for healed SCFE and has only been used by the senior author for this indication.
Relative Contraindications
Advanced degenerative articular changes of the femoral head and/or acetabulum
Noncooperative patient
Extreme obesity
Neuromuscular involvement leading to instability and subluxation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








