Fig. 1
Surgically dislocated hip demonstrating CAM lesion (inset-bottom) with preoperative anteroposterior radiograph with Dunn view (inset-top) and of a 24-year-old male
The amount of acetabular rim resection is determined on the basis of the magnitude of the damage to the acetabular cartilage and/or the degree of overcoverage, but resection should be less rather than more in order to avoid any instability of the hip joint. Currently, the senior author will perform rim resection for exposed subchondral bone secondary to acetabular cartilage delamination if associated with acetabular retroversion and >3 mm in depth. In the absence of cartilage delamination, acetabular rim trimming with labral refixation will be performed if the crossover sign extends more than 5 mm from acetabular roof. The labrum is taken down using an 11 blade and then retracted using a blunt probe.
The resection is performed with use of a curved 10-mm osteotome or high-speed burr, normally with exposure of the well-bleeding cancellous bone of the acetabular rim. If an area of acetabular cartilage damage persists, microfracture can be performed. Most acetabular rim lesions are located anterosuperiorly and require two to four bone anchors to reattach the labrum. It is important to note that the refixation of the tip of the labrum (not labral repair) requires a base of bleeding cancellous bone. Positioning of the anchors is performed under direct vision, about 2 mm away from the bone-cartilage interface. Knots are tied on the outer surface, with the suture being passed through the base of the labrum (Fig. 2). After acetabular rim trimming and labral refixation , the acetabulum is carefully irrigated to remove all osseous and fibrous debris. The nonspherical portion of the femoral head is assessed with the use of transparent spherical templates and usually is located anterosuperiorly and with a reddish appearance of the cartilage. Gentle removal of excess bone and recreation of a smooth femoral neck are performed with small curved chisels and repetitive assessment with templates. Excessive bone removal during the offset procedure should be avoided, although a resection of <30 % of the neck diameter has been reported to not weaken the femoral neck [42]. Furthermore, excessive resection may compromise the sealing function of the labrum. To address cam lesions extending superiorly or posterosuperiorly, the penetrating retinacular vessels were elevated and protected under direct visualization during the resection. Perfusion of the femoral head is checked by observation of the bleeding coming from the foveolar artery or the resection surface, and laser Doppler flowmetry is also possible [43]. Although in the initial experience of surgical dislocation a thin layer of bone wax was placed over the bleeding cancellous bone to avoid adhesions to the capsule, a recent report on allergic reaction has led to the abandonment of this technique [44].
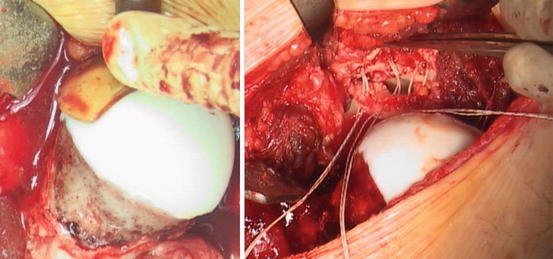
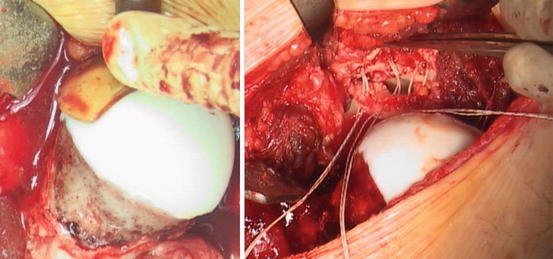
Fig. 2
Surgically corrected CAM lesion with suture anchors has been placed after acetabular rim trimming
Following reduction, the hip should once again be taken through a full range of motion paying special attention to those positions that were noted to cause impingement prior to dislocation [45]. If adequate resection of the offending lesions has been performed, the hip should be able to be taken through a full range of motion with no further impingement. The capsule is closed avoiding any tension because this may stretch the retinaculum and adversely influence the perfusion of the femoral head. The trochanteric fragment is anatomically reduced and fixed with two or three 4.5-mm cortical screws; the screws are best aimed toward the lesser trochanter. An intraoperative radiograph is used to confirm proper screw length/position and trochanteric reduction. Thereafter, the various soft tissue layers are closed with running or single sutures. Potential complications include trochanteric nonunion, heterotopic ossification, trochanteric bursitis, sciatic nerve palsy, osteonecrosis of the femoral head, femoral neck fractures, as well as intra-articular adhesions [22, 46, 47].
Postoperatively the patient should be restricted to toe-touch weight bearing on the operative extremity for 6–8 weeks until there is solid union of the trochanteric osteotomy site. During the same period, the patient receives deep vein thrombosis prophylaxis. Nonsteroidal anti-inflammatory drugs were given for 2 weeks postoperatively as heterotopic ossification prophylaxis. Physical therapy may be started immediately using passive range of motion for the first and second weeks postoperatively. At 10–14 days active motion may begin; however, flexion should be limited 70° for the first 6–8 weeks. Early range of motion will help prevent the formation of adhesions. Return to competitive sports depended on recovery of muscle function and strength, especially of the abductors. Typically, patients returned to competitive sports after 4–6 months [26, 48].
Summary
Surgical dislocation is a safe and powerful tool that allows open acetabular rim trimming, labral refixation, and femoral osteochondroplasty. One should not underestimate the technical demands of this surgical technique. Favorable good to excellent midterm clinical outcomes of 70–80% have been reported in the literature.
References
1.
Ganz R, Parvizi J, Leunig M, Siebenrock KA. Femoroacetabular Impingement: a cause for osteoarthritis of the hip. Clin Orthop. 2003;417(417):112–20.PubMed
2.
Mei-Dan O, McConkey MO, Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: can partial division of ligamentum teres and iliofemoral ligament cause subluxation? Arthrosc. 2012;28(3):440–5.CrossRef
3.
4.
Ayeni OR, Naudie D, Crouch S et al. Surgical indications for treatment for femoroacetabular impingement with surgical hip dislocation. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1676–83.
5.
6.
7.
8.
9.
Hack K, Diprimio G, Rakhra K, Beaule PE. Prevalence of CAM type femoroacetabular impingement in asymptomatic volunteers. J Bone Joint Surg. 2010;92A(14):2436–44.CrossRef
10.
Khannas V, Caragianis A, DiPrimio G et al. Incidence of hip pain in a prospective cohort of asymptomatic volunteers: is the cam deformity a risk factor for hip pain? Am J Sports Med. 2014;42(4):793–7, http://www.ncbi.nlm.nih.gov/pubmed/24481825
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








