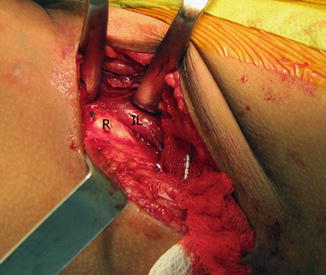
Fig. 1
Medial skin incision for ischial cut (Reproduced with permission from the Division of Orthopaedic Surgery, Children’s Hospital of Philadelphia)
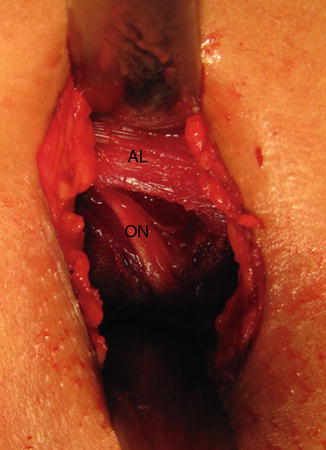
Fig. 2
The adductor longus tendon (AL) is identified and retracted proximally to reveal the underlying anterior branch of the obturator nerve (ON) (Reproduced with permission from the Division of Orthopaedic Surgery, Children’s Hospital of Philadelphia)

Fig. 3
The lane retractor is slid just lateral to the nerve through the obturator foramen along the quadrilateral plate until it “hooks” on the ischial spine (Reproduced with permission from the Division of Orthopaedic Surgery, Children’s Hospital of Philadelphia)
The correct starting point for the ischial cut is just inferior to the lip of the acetabulum; this can both be palpated and confirmed with the false profile view [6]. The cut should be aimed toward the proximal aspect of the ischial spine, as this negates the ability of the sacrospinous ligament to alter the mobility of the acetabular fragment (Fig. 4). A straight Ganz osteotome is used to make the osteotomy, starting on the medial side of the ischium followed by a second pass to cut the lateral side (Fig. 5). The position and depth of the cut can be periodically confirmed on the false profile view; throughout, the osteotome should be externally rotated such that the blade is on the “edge” on the image intensifier (Fig. 6). This results in a cut that is somewhat oblique in the coronal plane, angling from proximal medial to distal lateral. It is important that the medial lane retractor be kept in place during the medial cut to protect the contents of the sciatic notch. Similarly, the lateral lane retractor should be in place when cutting the lateral aspect of the ischium. Although use of these retractors obscures visualization on the image intensifier, the position of the osteotome can be confirmed by periodically withdrawing the lane (Fig. 7). Completion of the cut is confirmed by placing a Cobb in the osteotomy site and twisting to confirm fragment mobility. The wound is packed with a moist sponge in the event that the cut needs to be revisited.





Fig. 4
The ischial cut is aimed toward the proximal aspect of the ischial spine (Reproduced with permission from the Division of Orthopaedic Surgery, Children’s Hospital of Philadelphia)

Fig. 5
A straight Ganz osteotome is used to make the ischial osteotomy, starting on the medial side of the ischium followed by a second pass to cut the lateral side. A lane is used for protection (Reproduced with permission from the Division of Orthopaedic Surgery, Children’s Hospital of Philadelphia)

Fig. 6
The position and depth of the cut can be periodically confirmed on the false profile view. The osteotome should be externally rotated such that the blade is on the “edge” on the fluoroscopic image (Reproduced with permission from the Division of Orthopaedic Surgery, Children’s Hospital of Philadelphia)

Fig. 7
Retractors are needed for protection but obscure visualization. The position of the osteotome can be confirmed by periodically withdrawing the lane (Reproduced with permission from the Division of Orthopaedic Surgery, Children’s Hospital of Philadelphia)
Anterior Exposure and Pubis Cut
Similar to the exposure for an open reduction of the hip, an 8 cm incision is made parallel and 1–2 cm distal to the iliac crest, with approximately 3 cm of the incision extending medial to the anterior superior iliac spine (ASIS) (Fig. 8). The subcutaneous tissues are divided in line with the incision to expose the ilium; the overhanging external oblique muscle is feathered up and over the crest using bovie cautery.


Fig. 8
Skin incision for the anterior exposure (Reproduced with permission from the Division of Orthopaedic Surgery, Children’s Hospital of Philadelphia)
Next, the Smith-Peterson interval is entered indirectly by incising the fascia overlying the tensor fascia lata muscle belly at approximately a 30° angle to the ASIS. The muscle can be separated from the medial compartment fascia and retracted laterally. One can then bluntly dissect down through the interval to the level of the rectus tendon. This indirect approach to the interval helps minimize risk of injury to the lateral femoral cutaneous nerve. Visualization of the direct head of the rectus itself can be improved by incising the thin fascia overlying the tendon.
Using a no. 15 blade scalpel, the iliac crest apophysis is then split down its midline from the ASIS to the point at which the crest begins to swing back medially (Fig. 9). Only the medial half of the apophysis is elevated with a Cobb or Freer elevator in a subperiosteal fashion down the inner table of the iliac wing. Minimizing exposure of the outer table helps preserve abductor function postoperatively. The iliac exposure and the Smith-Peterson interval are now connected by sharply dissecting along the prow of the ilium connecting the ASIS and the anterior inferior iliac spine (AIIS). In spite of the indirect access to the interval, care should still be taken at this point to protect the lateral femoral cutaneous nerve, which can cross the surgical field from medial proximal to distal lateral. If identified, the nerve should be mobilized and retracted medially.
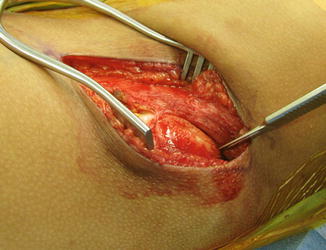
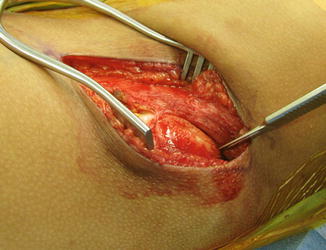
Fig. 9
Splitting of the apophysis (Reproduced with permission from the Division of Orthopaedic Surgery, Children’s Hospital of Philadelphia)
The most bloodless interval with which to access the pubis is between the medial edge of the rectus tendon and the iliacus muscle (Fig. 10). The iliacus can sometimes adhere to the underlying periosteum, but lifting up and away with a Hibbs or Aufranc retractor can help clearly define the surgical plane. Sharp extraperiosteal dissection with a scalpel can release any remaining muscle fibers. The psoas can then be retracted to reveal the pubic eminence, an important landmark that constitutes the next “bump” medial to the AIIS. In order to avoid injury to the triradiate cartilage and the acetabulum, the pubis cut must stay medial to this structure (Fig. 11). The iliopectineal fascia is first opened cephalad to the pubic ramus using a right-angle clamp. A lane retractor can then be passed around the superior edge of the ramus in an extraperiosteal fashion. The inferior edge of the ramus is slightly more difficult to define, but similar use of a Crego elevator followed by a lane can help create this channel. A Statinski vessel clamp can then be passed extraperiosteally from distal to proximal through the obturator foramen; a long Schnitt can be used to transfer a suture loop to the Statinski which can in turn be used to shuttle a Gigli saw around the pubic ramus (Fig. 12). Before the saw is passed, the shuttle suture is pulled taut to be sure that the adductor musculature does not contract which would indicate entrapment of the obturator nerve. While the pubis can be cut with other techniques (e.g., osteotome), use of a Gigli saw ensures a complete cut including the overlying and often thick periosteum.