Fig. 1
Stulberg IV hip that is not amenable to arthroscopic intervention. Clinical symptoms of greater trochanteric impingement. Note the amount of bone that would need to be removed to make the femoral head truly spherical (dotted circle). The patient was scheduled for an open surgical dislocation with osteochondroplasty and trochanteric transfer for a relative head-neck lengthening
Other sources of pain and dysfunction in patients with Perthes disease include extra-articular impingement and version problems in both the femur and acetabulum. Perthes patients may develop a relatively high-riding greater trochanter as a consequence of the proximal femoral physis arrest and collapse. This extra-articular impingement can be a cause of limited range of motion and dysfunction. Arthroscopy has little role in this instance and would better be treated by an open procedure, such as a trochanteric advancement with relative neck lengthening.
Perthes patients, historically, have had higher than normal femoral anteversion when compared with normal controls [23]. It has been suggested that this is a secondary deformation which may predispose the hip to further instability and pain. Additionally, there have been studies that have shown an increase in acetabular retroversion, while other studies have refuted this [24–26]. “Functional retroversion” of the femoral head has also been described when the posteromedial portion of the femoral head has remodeled in a retroverted position in relation to the anterolateral portion. This may help explain the paradox of why a Perthes patient walks with an externally rotated gait [27]. Arthroscopy would not have a role in these cases and open osteotomies would be recommended to correct significant version deformities.
Surgical Technique
Standard portals may need to be modified in LCPD patients secondary to trochanteric overgrowth, coxa magna, and surgical reconstruction of the acetabulum [22]. The anterolateral peritrochanteric portal may be more proximal than normal, and the use of accessory portals may be more common. The use of fluoroscopy is recommended to avoid iatrogenic damage to the hip joint. Occasionally, an outside-in technique may need to be utilized to gain access to the peripheral compartment first before entry into the central compartment particularly in cases in which acetabular reorientation has already been performed [28].
After access to the central compartment, inspection of the joint can be conducted. Commonly, loose bodies may be encountered, most times originating from the femoral head. They should be removed with arthroscopic graspers, shavers, or suction (Fig. 2). The chondral surfaces can be inspected and chondroplasty or microfracture can be performed on the acetabulum, femoral head, or both. Labral pathology is also commonly found and may be addressed by either labral debridement in the cases of a hypertrophied labrum, an infolded labrum, or labral fraying or, more commonly, repair of the labrum with suture anchors (Fig. 3).
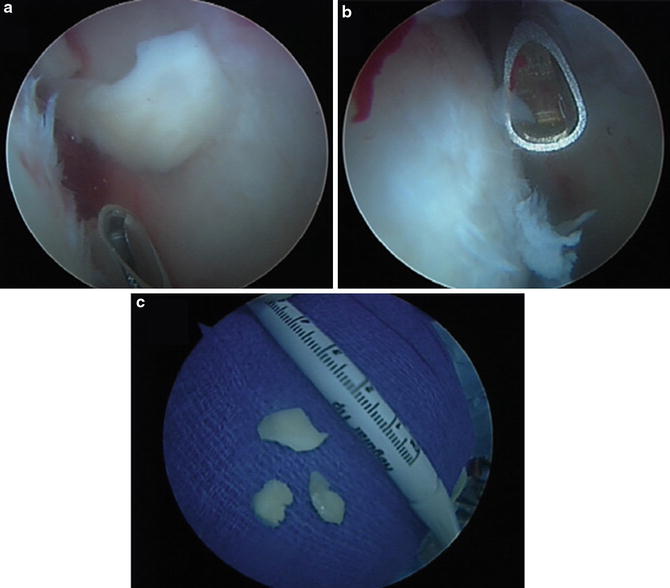

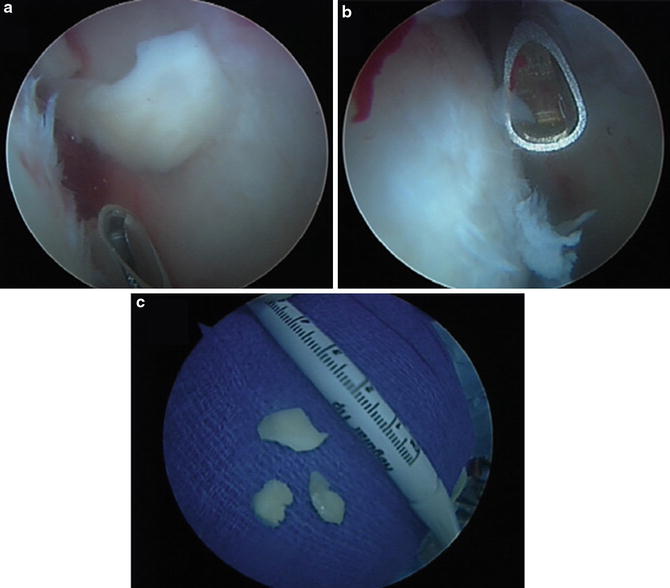
Fig. 2
Central compartment access of a Perthes hip. (a) Chondral flap of the acetabulum. (b) Chondral fraying of the femoral head. (c) Removal of loose bodies from the central compartment

Fig. 3
Labral repair in Perthes hip utilizing suture anchors into the acetabulum
Once work is completed in the central compartment, the peripheral compartment work can be addressed. A generous capsulotomy is helpful with the increased in the femoral head-neck size. Any loose bodies in the peripheral compartment should be removed at this time (Fig. 4). Recontouring of the femoral head-neck junction will depend on the Stulberg classification, with Stulberg I/II hips more amenable to a suitable osteochondroplasty (Fig. 5). With the Perthes hip, the amount of recontouring that is able to be conducted will depend upon preoperative templating and how ovoid the femoral head-neck junction is. The use of liberal fluoroscopy and dynamic examination will guide the osteochondroplasty. It is very rare that a Perthes head can be actually made truly spherical, particularly a Stulberg III–V femoral head (Fig. 6). A dynamic and fluoroscopic examination should be conducted to ensure adequate bony resection. A capsule closure can be performed, particularly in patients who are ligamentously lax or have complaints of instability.

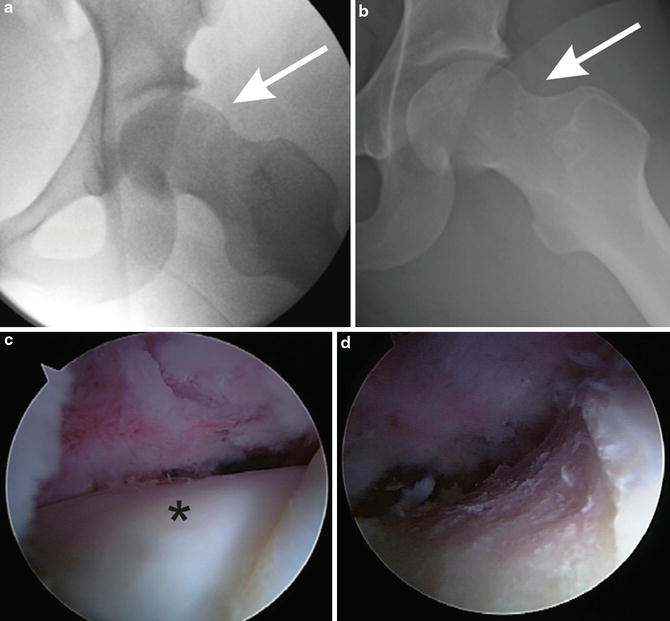


Fig. 4
Removal of loose bodies in the peripheral compartment. Osteochondroplasty has already been performed of the femoral head-neck junction
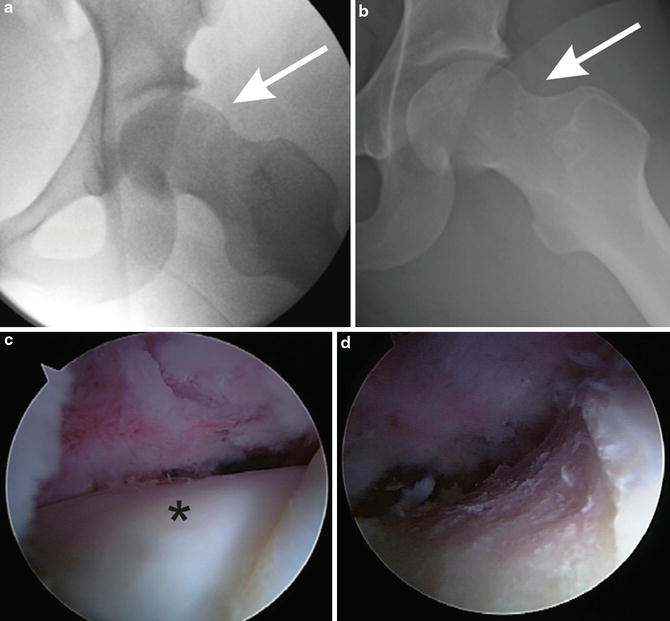
Fig. 5
Osteochondroplasty of a Stulberg I hip with only minimal femoral head-neck deformity. (a) Preoperative head-neck junction showing decreased head-neck offset with no acetabular deformity. (b) Postoperative head-neck junction after osteochondroplasty. (c) Intraoperative photo of preoperative head-neck junction prior to osteochondroplasty (asterisk). (d) Intraoperative photo following osteochondroplasty

Fig. 6
Osteochondroplasty of a Stulberg IV Hip. (a) Preoperative Dunn-lateral radiograph (arrow depicts the osseous bump at the femoral head-neck junction). (b) Postoperative Dunn-lateral radiograph after osteochondroplasty of the femoral head-neck junction
Postoperative management is similar to that of patients treated with idiopathic FAI, with foot-flat weight bearing for 2–4 weeks followed by a rigorous physical therapy regimen [29]. A continuous passive motion machine is used for 2–3 weeks unless a microfracture was done in which case the CPM is used for 6 weeks. Generally, return to activity occurs at 4–6 months.
Pearls and Pitfalls
Proper preoperative planning is paramount. Identification of the Stulberg classification of the LCPD is used to decide upon open vs. arthroscopic procedures.
Removal of all loose bodies is critical and thorough examination of the central and peripheral compartment is necessary.
A generous capsulotomy or “T-shaped” capsulotomy can be used because of the enlarged femoral head-neck junction. Consideration can be made to close the capsulotomy.
Liberal use of fluoroscopy to identify the exact areas of resection and prevent under- or over-resection.
Outcomes
Despite multiple studies, an optimal treatment for LCPD has yet to be found. Historically, outcomes from LCPD demonstrated overall good results especially for Stulberg I and II hips with variable results for Stulberg III and poor results for IV and V [1, 12, 30]. In a recent multicenter prospective study, Larson et al. reported on 20 years of follow-up for 56 LCPD patients in their third decade of life that were treated nonoperatively [31]. They showed that at least half of these young patients had poor or fair outcomes and that hip pain was associated with positive impingement signs on physical exam. The study also showed that 60 % of Stulberg III, IV, and V hips had evidence of osteoarthritis, similar to Stulberg’s initial study, but at a much younger age.
With the femoral head-neck “bump” being recognized as a source of impingement and resultant dysfunction in late LCPD, initial studies reported on performing “cheilectomies” with highly satisfactory results 2–3 years postoperatively [32]. However, in a 25-year follow-up of five LCPD patients who underwent cheilectomy, all patients had developed osteoarthritis and three of the five had poor results, while the other two had fair or good results [33].
Several studies have looked at results of arthroscopic management of patients with LCPD. Roy et al. performed nine hip arthroscopies on LCPD patients with one being a Stulberg II, one a Stulberg IV, and the rest Stulberg III [22]. The surgery was conducted during adolescence following a pain-free interval. Eight of the nine patients had abnormalities noted on arthroscopy and seven of these eight improved their symptoms enough to play sports. The one patient that experienced no improvement had osteoarthritis, had significant femoral head deformity, and was classified as a Stulberg IV. Within 2 years, two of the seven underwent repeat arthroscopy due to recurrence of symptoms (one at 18 months, one at 2 years). A third patient underwent total hip arthroplasty after 2 years of no symptoms. Kocher et al. reported on 54 hip arthroscopies in children and adolescents, including eight LCPD patients [34]. Their mean mHHS improved by a mean of over 30 points, which was statistically significant. Bowen et al. reported on their experience of hip arthroscopy for OCD after LCPD [35]. The three patients who had the OCD fragment removed were asymptomatic at 1 year, while the two without removal had severe degeneration of the femoral head. O’Leary et al.’s series of 84 patients included 9 who had LCPD. Eighty-eight percent of the LCPD had improvement postoperatively [36]. More recently, Freeman et al. reported on 22 patients ranging from Stulberg I-IV with a median age of 27. Eighteen labral tears were identified, along with 17 torn ligamentum teres, 17 chondral lesions, 5 loose bodies, 3 osteochondral defects, and 2 cam lesions. All patients improved with a modified Harris hip score of 82 postoperatively compared to 56.7 preoperatively which did not correlate with the Stulberg classification. Two patients underwent repeat arthroscopy for failure of pain relief [37].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








