Fig. 1
Estimating femoral anteversion
For the surgical procedure, the patient is positioned supine on a radiolucent operating table with a small bump placed under the ipsilateral iliac crest. Split drapes are used to allow access to the entire hemipelvis with care taken to place the posterior limb as posterior as possible to prevent draping out the ilium. Paralysis is avoided to facilitate identification of the femoral nerve if need be.
If the patient has already failed an attempt at closed reduction at a prior date, then preoperative arthrography is typically not performed. If this is not the case, an arthrogram can be performed to determine whether closed treatment is possible or if the open reduction is necessary. In general, the need for an open reduction increases beyond a year of age [1, 3, 5].
Open Reduction
A 6–8 cm incision is made parallel and 1 cm distal to the iliac crest, with approximately 3 cm of the incision extending medial to the anterior superior iliac spine (ASIS) (Fig. 2). The subcutaneous tissues are divided in line with the incision to expose the iliac crest and its overhanging external oblique muscle. Using Bovie cautery, the obliques can be feathered up and off the crest, taking care not to burn too much of the apophyseal cartilage (Fig. 3).



Fig. 2
Incision

Fig. 3
Exposure of iliac crest apophysis
Next, the Smith-Peterson interval is found on a line connecting the ASIS and the patella, usually 1–2 cm distal to the ASIS itself. It is helpful to palpate the muscle bellies of the sartorius and the tensor fascia lata and find the soft depression in between. One can then spread bluntly down through the interval to the level of the rectus tendon (Fig. 4). Alternatively, one can access the interval by opening the sheath of the tensor fascia lata a few millimeters lateral to the interval itself. Once opened, the muscle belly can be retracted laterally allowing entry into interval. This approach is theoretically more protective to the lateral femoral cutaneous nerve and has been described for periacetabular osteotomies. Visualization of the direct head of the rectus itself can be improved by incising the thin fascia overlying the tendon.


Fig. 4
Smith-Peterson interval
Using a 15 blade scalpel, the iliac crest apophysis is then split down its midline from the ASIS to the point at which the crest begins to swing back medially. The medial and lateral halves of the apophysis can then be “popped” off of the boney ilium using fingers or a freer elevator (Fig. 5). Sponges may be packed subperiosteally along both the inner and outer tables.
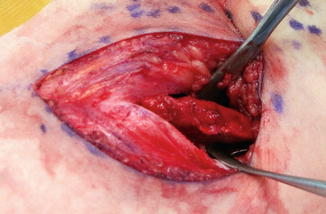
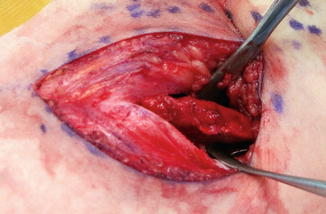
Fig. 5
Splitting of apophysis to reveal underlying iliac crest
The iliac exposure and the Smith-Peterson interval are now connected by sharply dissecting along the prow of the ilium connecting the ASIS and the anterior inferior iliac spine (AIIS). Care should be taken at this point to protect the lateral femoral cutaneous nerve, which passes from medial proximal to distal lateral (Fig. 6). Once identified, the nerve should be mobilized and retracted medially. The direct head of the rectus should be fully defined and then transected just distal to its insertion on the AIIS. It can be tagged for later repair.


Fig. 6
Lateral femoral cutaneous nerve
The anterior capsule most now be exposed using a Cobb elevator or sharp dissection to clear off residual fibers of the iliocapsularis muscle. Proximally and laterally, one must define the interval overlying the capsule but underneath the abductor complex. This is best done with a Crego elevator using it to not only enter the interval but to define it medially all the way to the upper border of the false acetabulum (Fig. 7). The periosteum overlying the outer table of the ilium can now be elevated more distally through the pseudo-acetabulum. The anterior and superior exposure of the capsule is completed by partially releasing the junction of the lateral subperiosteal interval and the pericapsular interval from front to back using a curved Mayo scissor.
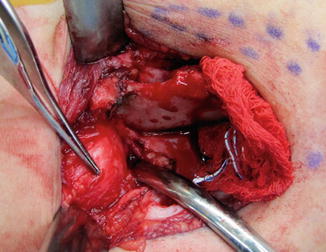
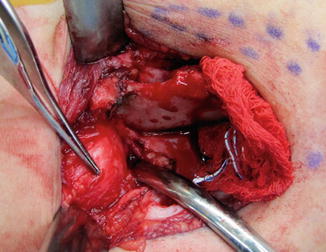
Fig. 7
Developing the pericapsular interval with Crego. Forceps point to anterior capsule overlying femoral head
Working medially, the iliopsoas is identified as it crosses into the pelvis just on the medial size of the periosteum overlying the inner table. The tendon lies distal to the pubis and posterior in relation to the muscle belly itself. It is best exposed by rolling the muscle medially on itself using forceps, and then capturing the tendon with a right angle clamp inserted from medial to lateral (Fig. 8). If there is any confusion, the psoas tendon can be distinguished from the femoral nerve by noting muscle fibers entering the structure, checking that it tightens with internal rotation of the hip, and confirming that there is no reaction to light touch with Bovie cautery (assuming that the patient is not paralyzed). Release of the tendon may then be performed with cautery. Once released, retraction of the psoas becomes quite easy, and the hip capsule can now be exposed as medially as possible along and inferior to the pubic ramus.


Fig. 8
Psoas tendon
The capsulotomy is performed in a “T” shape with the top of the incision running along the acetabular margin and the stem of “T” brought out horizontal roughly over the center of the dislocated femoral head (Fig. 9). It is important that the capsule be released as medial as possible to allow full exposure of the true acetabulum. Using a scalpel, the initial incision into the capsule is best performed medially over the empty acetabulum to prevent inadvertent injury to the articular cartilage of the femoral head. The capsulotomy can then be safely extended using scissors. The redundant corner may be excised to facilitate later capsulorrhaphy (Fig. 10).
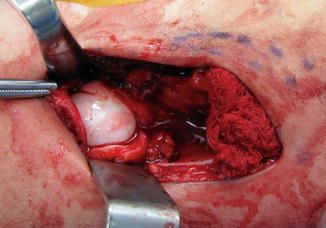
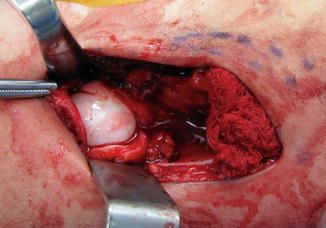
Fig. 9
Capsulotomy
Fig. 10
Schematic of capsulotomy and repair
The first structure to identify upon opening the hip joint is the ligamentum teres. This can be sharply transected off of the femoral head using a scalpel and then followed down to the true acetabulum before being excised with scissors (Fig. 11). The pulvinar can be removed from the acetabulum with a pituitary rongeur to expose the acetabular cartilage (Fig. 12). Finally, the transverse acetabular ligament should be released from the depths of the acetabulum where it joins both ends of the labrum as it crosses the cotyloid fossa. This is an extremely important step to allow relaxation and expansion of the labrum, which widens the acetabular opening to accommodate the femoral head.
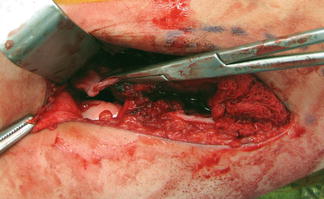
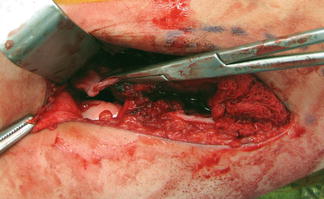
Fig. 11




The ligamentum teres is transected and followed into the true acetabulum
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








