Surgical Repair of Fifth Digit Deformities
Thomas F. Smith
Carl A. Kihm
Keith D. Pfeifer
Chronically painful problems of the fifth toe are a common source of patient complaints regardless of age, occupation, or activity level. Pain is typically associated with hyperkeratoses in various locations or combinations of locations about the fifth toe. Asymptomatic hyperkeratosis in the insensate foot associated with conditions such as sensory neuropathy can result in wounds on the fifth toe and their associated complications. Hyperkeratoses generally occur from pressure of the fifth toe against the shoe, the fourth toe, or a combination of both. Painful pressure hyperkeratoses are more often the result of deformity of the fifth toe rather than ill-fitting shoes. The fifth toe, the shoes, or both are all important etiologic possibilities when considering nonoperative or operative treatment options. Nonoperative treatments including periodic or regular débridement of the hyperkeratosis combined with various digital paddings and shoe accommodations can improve patient comfort. These measures are not necessarily expected to correct fifth toe deformities but can relieve pressure and reduce pain. If nonoperative treatments do not meet patient needs, surgical intervention to attempt correction of fifth toe deformities is not an unreasonable treatment option. Surgical intervention, in the absence of fifth toe deformity to permit comfort for specific shoe wear or fashion needs, is not realistic.
Surgical correction of deformities of the fifth toe, as compared with the remaining lesser digits, presents special challenges. The fifth toe anatomy includes three bones, three joints, as well as intrinsic and extrinsic musculature, all rather small and delicate. The fifth toe is without a lateral supporting buttress as the lateralmost digit of the forefoot. It lies in closest proximity to the inner lateral toe box of shoes. Intrinsic fifth toe stability is necessary postoperatively to help maintain the position of correction, especially important for wearing opentoed shoes such as sandals. This close proximity of the fifth toe to shoe pressures requires supple scarring of both the skin and deeper structures postoperatively. Persistent postoperative swelling can readily occur in the fifth toe, especially if surgical dissection principles and appropriate postoperative dressing and splinting techniques are not appreciated and employed. A chronically edematous and indurated fifth toe postoperatively can be as painful to shoe pressure as the presenting osseous deformity and hyperkeratosis preoperatively. A multitude of surgical procedure options are available to the surgeon to address the many fifth toe pathologies possible. An appreciation for patients and their complaints, the location or locations of hyperkeratosis, and the various positions and planes of fifth toe deformities all require careful consideration in determining the procedural approach best suited for the particular needs of the patient.
FIFTH TOE SURGICAL ANATOMY
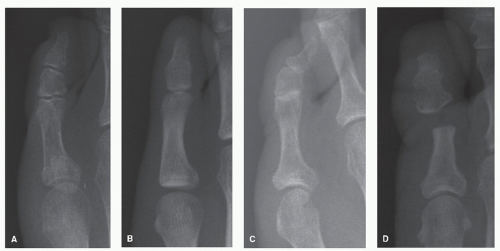
The anatomy of the fifth toe is unique and must be appreciated to understand the implications of various deformities and their specific surgical correction (Fig. 18.1). The fifth toe is the lateralmost digit and contains three bones, the proximal, middle, and distal phalanges, with two ginglymus joints, the proximal and distal interphalangeal joints. The fifth toe articulates with the fifth metatarsal through the fifth metatarsophalangeal joint. The middle and distal phalanges may be congenitally fused and function as a coalition. This synostosis can result in a loss of flexibility within the toe making it more difficult for the fifth toe to accommodate to shoe pressures. This condition predisposes the fifth toe to develop painful pressure hyperkeratoses medially and laterally, especially at the distal interphalangeal joint synostosis site. The associated interphalangeal stiffness with the absence of distal digital mobility can result not only in painful pressure hyperkeratoses of the fifth toe but also in painful thickening and dystrophy of the fifth digital nail from chronic shoe irritation.
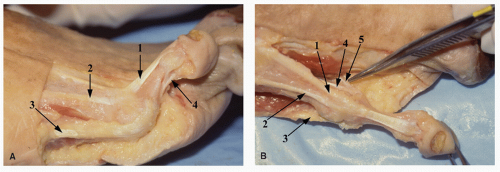
The anatomy of the metatarsophalangeal joint and extrinsic musculature of the fifth toe is analogous to that of the remaining lesser metatarsophalangeal joints. The specific intrinsic muscles and tendons of the fifth toe differ. No short extensor tendon segment inserts into the long extensor tendon of the fifth toe as occurs in the first through fourth digits. An anomalous tendon slip can present, termed the peroneus digiti quinti, extending distally primarily from the peroneus brevis on the dorsal lateral aspect of the fifth metatarsophalangeal joint (1,2). The fourth lumbrical muscle originates from the contiguous sides of the long flexor tendons to the fourth and fifth toes coursing plantar to the transverse intermetatarsal ligament to insert into the medial extensor wing of the fifth metatarsophalangeal joint. It functions to aid extension and adduction to the fifth proximal phalanx. The fifth toe has no dorsal interosseous muscle (Fig. 18.2).
The third plantar interosseous muscle originates from the medial surface of the fifth metatarsal to course dorsal to the transverse intermetatarsal ligament and insert in the medial aspect of the base of the fifth proximal phalanx. The unipennate flexor digiti quinti brevis muscle arises from the plantar surface of the base of the fifth metatarsal to insert into the plantar lateral surface of the fifth proximal phalanx. The function of these two muscles is to stabilize the fifth metatarsophalangeal joint in plantarflexion before contraction of the long flexor tendon. The abductor digiti minimi is a rather long fusiform muscle that originates from the lateral calcaneal tuberosity to insert into the lateral base of the fifth proximal phalanx. This muscle in some individuals can independently abduct the fifth
toe. It is innervated by the first branch of the lateral plantar nerve or Baxter nerve, and loss of this function can be indicative of nerve entrapment at this level. Sensation to the fifth toe is provided by the lateral plantar nerve of the posterior tibial nerve plantarly and the intermediate dorsal cutaneous nerve branch of the superficial peroneal nerve and possibly sural nerve dorsally.
toe. It is innervated by the first branch of the lateral plantar nerve or Baxter nerve, and loss of this function can be indicative of nerve entrapment at this level. Sensation to the fifth toe is provided by the lateral plantar nerve of the posterior tibial nerve plantarly and the intermediate dorsal cutaneous nerve branch of the superficial peroneal nerve and possibly sural nerve dorsally.
SURGICAL PRINCIPLES
PLANES OF DEFORMITY
Deformities of the fifth toe can involve one or more of the three cardinal body planes (Fig. 18.3). The sagittal plane fifth toe deformities are hammertoe, claw toe, and mallet toe. The
hammertoe deformity of the fifth toe presents with either rigid or flexible flexion contracture of the proximal interphalangeal joint. This flexion deformity is associated with varying degrees of extension deformity at the fifth metatarsophalangeal joint. Extensor contracture of the fifth metatarsophalangeal joint can result in retrograde forces that increase pressure on the plantar fifth metatarsal with hyperkeratosis formation beneath the fifth metatarsal head. Both extensor contracture or flexor weakness can reduce fifth toe purchase power to the weight-bearing surface. A dorsally displaced fifth metatarsal
following fracture or surgery can likewise reduce fifth toe to floor purchase power. A “floating” fifth toe that does not touch the floor can be symptomatic from shoe irritation and affect fourth toe position and alignment. Reestablishing flexor power to the fifth toe can be a difficult surgical challenge. Extensor contracture of the fifth metatarsophalangeal joint level may require surgical release that is separate and distinct from the flexion release that may be necessary at the proximal interphalangeal joint level. A congenital sagittal plane deformity of the fifth toe, termed digiti quinti varus, is associated with extreme extensor contracture of the fifth metatarsophalangeal joint. Extensor contracture here can involve all dorsal fifth metatarsophalangeal joint soft tissue structures from the joint to include the skin. Claw toe deformity of the fifth toe involves flexion contracture of both interphalangeal joints associated typically with flexor contracture of the metatarsophalangeal joint. Generally, claw toe deformities involve all of the digits, rarely just the fifth, and are associated with neuromuscular imbalances. Mallet toe deformities with flexion contracture of only the distal interphalangeal joint of the fifth toe are of little clinical significance.
hammertoe deformity of the fifth toe presents with either rigid or flexible flexion contracture of the proximal interphalangeal joint. This flexion deformity is associated with varying degrees of extension deformity at the fifth metatarsophalangeal joint. Extensor contracture of the fifth metatarsophalangeal joint can result in retrograde forces that increase pressure on the plantar fifth metatarsal with hyperkeratosis formation beneath the fifth metatarsal head. Both extensor contracture or flexor weakness can reduce fifth toe purchase power to the weight-bearing surface. A dorsally displaced fifth metatarsal
following fracture or surgery can likewise reduce fifth toe to floor purchase power. A “floating” fifth toe that does not touch the floor can be symptomatic from shoe irritation and affect fourth toe position and alignment. Reestablishing flexor power to the fifth toe can be a difficult surgical challenge. Extensor contracture of the fifth metatarsophalangeal joint level may require surgical release that is separate and distinct from the flexion release that may be necessary at the proximal interphalangeal joint level. A congenital sagittal plane deformity of the fifth toe, termed digiti quinti varus, is associated with extreme extensor contracture of the fifth metatarsophalangeal joint. Extensor contracture here can involve all dorsal fifth metatarsophalangeal joint soft tissue structures from the joint to include the skin. Claw toe deformity of the fifth toe involves flexion contracture of both interphalangeal joints associated typically with flexor contracture of the metatarsophalangeal joint. Generally, claw toe deformities involve all of the digits, rarely just the fifth, and are associated with neuromuscular imbalances. Mallet toe deformities with flexion contracture of only the distal interphalangeal joint of the fifth toe are of little clinical significance.
The frontal plane component of fifth toe deformities is commonly seen and often overlooked. It almost always represents as a varus rotation resulting clinically in the fifth digital nail facing laterally rather than dorsally. The varus position of the fifth digital nail represents a varus alignment of the osseous structures within the toe including the middle and distal phalanges as well as the distal interphalangeal joint. The padded weight-bearing tuft of the fifth toe is rotated medially. Body weight is transmitted abnormally through the lateral unpadded surface of the toe over the prominences of both the proximal and distal lateral interphalangeal joint condyles rather than the padded tuft of the toe. As a consequence, painful pressure hyperkeratoses may develop over the lateral aspect of the toe from the proximal interphalangeal joint area to the lateral margin of the nail at the distal interphalangeal joint.
Transverse plane deformities of the fifth toe involve either adduction or abduction. Adduction of the fifth toe is an exaggeration of frontal plane varus that can result in uncomfortable or painful underlapping or overlapping of the fifth toe about the fourth toe. Radiographs can demonstrate a wedgeshaped middle phalanx of the fifth toe with a shortened medial surface length relative to the lateral surface length as opposed to a more symmetrical structure. Abductory deformity of the fifth toe can be noted following surgery or trauma. The medial collateral ligaments of either the metatarsophalangeal joint or the proximal interphalangeal joint can be weakened resulting in lateral toe deviation. Malunion of phalangeal fractures and resorption or hypertrophy of bone following fifth digital surgery can result in transverse plane deformities of the fifth toe. Abductory weakness or deformity of the fifth toe can make closed-toed shoe fit painful from pressure and open-toed shoe wear awkward with overriding of the toe over the lateral edge of the shoe.
PRESSURE HYPERKERATOSES
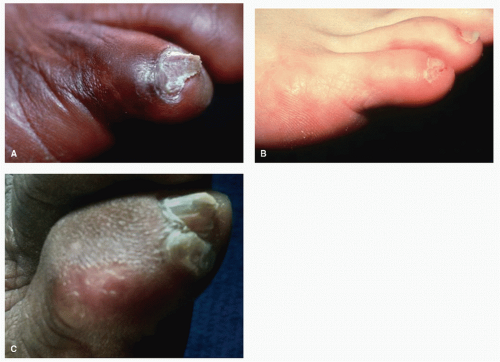
The classic patient complaint associated with a painful fifth toe is a pressure hyperkeratosis known as a “hard corn” or heloma durum located on the dorsolateral or lateral aspect of the proximal interphalangeal joint (Fig. 18.4). The “soft corn” or heloma molle is located proximally and medially between the fourth and fifth toes (3,4) (Fig. 18.5). These interdigital lesions should not be confused with skin conditions such as interdigital tinea or psoriasis. An abscess or cellulitis can develop in this thin sensitive skin between the toes complicating the lesion. Pressure hyperkeratosis may occur as isolated lesions or on multiple sites of the fifth toe. Multiple heavy areas of hyperkeratosis on a fifth toe may represent a skin problem, not necessarily a fifth toe deformity or shoe pressure problem. An individual with skin sensitive to form pressure hyperkeratoses can impact prognosis for a successful nonsurgical or surgical treatment course. Various morphologic types of pressure hyperkeratosis can be noted. Discrete, well-localized, and deep-seated lesions generally result in rather acute and severe pain. These must be distinguished from verruca. A more diffuse and larger lesion may be less acutely painful but still rather bothersome. Some patients may have only a thickening or lichenification of the skin known as a “knuckle pad,” which is minimally asymptomatic and may be more of a cosmetic concern. Other complaints of pain may be associated with chemical burns from home topical acid plaster treatments, fluid-filled friction blisters, or wounds and ulcerations in individuals with neurovascular compromise. Fifth toe pain may be suspected and associated with nerve damage, bursitis, or arthrosis if local débridement of an overlying pressure hyperkeratosis provides little relief of pain. More complex skin pathologies such as metastatic squamous cell carcinoma resembling cellulitis as well as osteomyelitis have been described on the fifth toe (5). Pressure hyperkeratoses about the fifth toe are more often the result of deformity and malalignment of the fifth toe rather than exostoses or bony prominences (6,7 and 8). Surgical correction of a fifth toe deformity typically resolves painful lesions. Surgical remodeling of exostoses or prominent bony contours in the absence of fifth toe deformities can be effective in managing painful pressure hyperkeratoses of the fifth toe and meeting patient needs.
Careful identification of the location of pressure hyperkeratoses on the fifth toe helps determine the surgical correction to be employed. One of the most common locations for a pressure hyperkeratosis on the fifth toe is the lateral or dorsolateral aspect of the proximal interphalangeal joint. This lesion is typically associated with flexion contracture of the proximal interphalangeal joint and varying degrees of extensor contracture of the metatarsophalangeal joint in the sagittal plane or a classic hammertoe deformity. In the absence of deformity, an exostosis at the proximal interphalangeal joint or digital malalignment and malunion from a prior fifth toe phalanx fracture may account for the pressure hyperkeratosis. The dorsolateral or lateral hyperkeratosis may extend well over the middle phalanx. A combination of sagittal plane deformity combined with frontal plane varus positioning can result in a broader exposed area for shoe irritation and hyperkeratosis formation. It should always be remembered that poorly fitting shoes in the absence of fifth toe pathology can result in pressure hyperkeratosis.
Interdigital pressure hyperkeratosis can develop between the fourth and fifth toes. These lesions can be deep and proximal in the web space overlying the adjacent surfaces of the lateral aspect of the fourth metatarsophalangeal joint and the medial aspect of fifth proximal interphalangeal joint. The lesions may be more distal in the interdigital space overlying
the lateral aspect of the proximal interphalangeal joint of the fourth toe and the medial aspect of the distal interphalangeal joint of the fifth toe. Fifth toe deformities can result in interdigital malalignment with the fourth toe bringing the broader bone structural areas about the joints into apposition creating pressure and hyperkeratoses. Foreshortening of the fourth or fifth rays by surgery or fracture can result in this type of interdigital joint apposition resulting in painful hyperkeratosis between the toes. Interdigital exostoses from trauma or arthritic processes can result in interdigital pressure hyperkeratoses. This type of lesion is found more often in women than men (7).
the lateral aspect of the proximal interphalangeal joint of the fourth toe and the medial aspect of the distal interphalangeal joint of the fifth toe. Fifth toe deformities can result in interdigital malalignment with the fourth toe bringing the broader bone structural areas about the joints into apposition creating pressure and hyperkeratoses. Foreshortening of the fourth or fifth rays by surgery or fracture can result in this type of interdigital joint apposition resulting in painful hyperkeratosis between the toes. Interdigital exostoses from trauma or arthritic processes can result in interdigital pressure hyperkeratoses. This type of lesion is found more often in women than men (7).
Isolated lesions over the lateral aspect of the distal interphalangeal joint of the fifth toe, known as a “Lister’s corn,” can be very painful (Fig. 18.6). A patient typically relates the perception of having two fifth toe nails. The more lateral false “nail” can be rather symptomatic and represents a pressure hyperkeratosis within the lateral nail groove of the fifth toe. Minimal fifth toe deformity is typically noted other than possibly frontal plane varus rotation. Radiographs can show an exostosis at the
lateral distal interphalangeal joint. Typically, a synostosis of the middle and distal phalanx exists in the presence of this lesion. The fifth toe nail itself can become permanently dystrophic and thickened from shoe irritation resulting in a secondary source of pain separate and distinct from the pressure hyperkeratosis.
lateral distal interphalangeal joint. Typically, a synostosis of the middle and distal phalanx exists in the presence of this lesion. The fifth toe nail itself can become permanently dystrophic and thickened from shoe irritation resulting in a secondary source of pain separate and distinct from the pressure hyperkeratosis.
 Figure 18.5 Pressure hyperkeratosis possibilities of the fourth interdigital space. A: Proximal location in web space. B: Distal location in web space. |
FLEXIBILITY AND RIGIDITY
The joints of the entire fifth ray should be manually manipulated to assess the rigidity or flexibility of the deformity. Both active and passive ranges of motion should be compared as a marker for neuromuscular disease or compromise. The fifth toe position and function should be observed in stance and gait. Rigidity as a factor of joint ankylosis can be of a bony or soft tissue etiology. The longer the duration of the deformity, the more rigid the deformity can become over time. The fifth toe can be rigidly deformed by arthritic changes as any of the interphalangeal joints of the fingers or toes. The fifth toe is prone to fracture and injury that can affect joint mobility and flexibility long-term. Synostosis of the middle and distal phalanges of the fifth toe has been described as the most common coalition of the foot (9). This synostosis creates a more rigid fifth digit not as adaptable to shoe pressures and prone to painful distal pressure keratoses and nail dystrophy problems (10). Radiographically, there is absence of the distal interphalangeal joint, and clinically, with careful palpation, absence of distal motion near the base of the nail can be appreciated. The fifth digit with a synostosis of the middle and distal phalanx can be clinically thicker and broader relative to the fourth toe. Sonographic hypoplasia of the fifth toe middle phalanx has been described as an associated finding in Down syndrome (11). Neuromuscular imbalance creating spasticity or contracture of the tendons can result in rigidity of the fifth toe. Spasticity as opposed to rigidity may only present in active foot function of gait and not be evident in non-weight-bearing in the clinical evaluation. Painful pressure hyperkeratoses of the fifth toe with little clinical deformity may represent digital rigidity with inability of the toe to conform to shoes. Flexible and reducible fifth toe deformities can be noted in neuromuscular imbalances and represent a need to not only surgically correct the deformity but also create stability for maintenance of correction. Flexible digital deformities such as hammertoes, regardless of etiology, can represent a neuromuscular imbalance that results in insidious progression of deformity and increasing rigidity over time. Hypermobility or joint laxity of the fifth toe can be the result of poorly healed joint soft tissues following trauma or surgery. This “flail” fifth toe does not help balance fifth metatarsal function. Malposition and weakness of the fifth toe can be rather troublesome especially for open-toed shoe wear. Surgical reconstruction of the unstable flail fifth toe has been described with the use of interpositional bone graft (12,13).
SURGICAL PROCEDURES
METATARSOPHALANGEAL JOINT RELEASE
As with hammertoe deformities of the central digits, extensor contracture of the metatarsophalangeal joint of the fifth toe can contribute substantially to the hammertoe deformity and patient complaints (Fig. 18.7). Resecting the head of the fifth proximal phalanx, or a classic fifth toe “arthroplasty,” to repair hammertoe deformity releases flexion contracture at the proximal interphalangeal joint but effects little release of extensor contracture at the fifth metatarsophalangeal joint (14). Inadequate fifth metatarsophalangeal joint release can produce a prominent fifth proximal phalangeal stump dorsally with apparent need for further fifth proximal phalanx resection. Overzealous resection of additional bone from the fifth proximal phalanx serves only to shorten and weaken the fifth toe and does not encourage any reduction of extensor deformity at the fifth metatarsophalangeal joint. A dorsally prominent fifth proximal phalanx generally represents extensor contracture at the fifth metatarsophalangeal joint, not inadequate bone resection of the fifth proximal phalanx. Surgical extensor release of the fifth metatarsophalangeal joint involves first long extensor tendon lengthening typically by a Z-plasty technique. This is followed by the extensor hood release that lengthens the extensor tendon from its origin in the leg to its insertion in the toe, including the functional insertion of the metatarsophalangeal joint. If extensor contracture is still noted, the dorsal capsule of the metatarsophalangeal joint is incised transversely (6). This dorsal release may need to be carried medially and laterally to release all contracted tissues on the extensor side of the transverse metatarsophalangeal joint axis. Any medial release of the fifth metatarsophalangeal joint should be done with care to avoid overly weakening the joint medially. Medial fifth metatarsophalangeal joint weakness can result in the unopposed fifth toe deviating laterally postoperatively. Additional release may be required on the plantar aspect of the metatarsophalangeal joint with a McGlamry elevator if plantar capsular adhesions block plantarflexion of the joint.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree