Fig. 13.1
Sagittal T2-weighted lumbar MRI image demonstrating degeneration of the L4–5 intervertebral disc (white arrow). Water has high signal intensity on T2-weighted MRI imaging. As the disc degenerates, it loses its water content and, as such, loses its high signal intensity compared to the healthy disc. The degenerative disc becomes grey or black and is often referred to as a “dark disc.” Note that the L3–4 and L5–S1 discs above and below the L4–5 level still have high signal intensity
Discography can be a useful tool to differentiate the source in discogenic low back pain. The test involves pressurizing the disc with contrast dye in an attempt to stimulate nerve endings in injured discs. Discography can provide information regarding the morphology of the degenerated disc and can assist with identifying the pain generator (Fig. 13.2). Precise reproduction of the patients presenting pain symptoms, or concordance, makes the test clinically useful. Some studies have identified a high level of sensitivity and specificity, whereas others have disputed this claim (Mooney et al. 1988; Walsh et al. 1990; Simmons et al. 1988; Carragee et al. 2000; Guyer and Ohnmeiss 1995). Carragee et al. showed discography to have a best-case positive predictive value of 50–60 % (Carragee et al. 2006). The subjective nature of the test can never completely be overcome, but it is arguably the only study whereby a painful degenerated disc can potentially be identified. However, the use of discography should be carefully considered in terms of risks and benefits because accelerated disc degeneration, disc herniation, and loss of disc height have been reported in comparison to matched controls at a 7–10-year follow-up (Carragee et al. 2009).
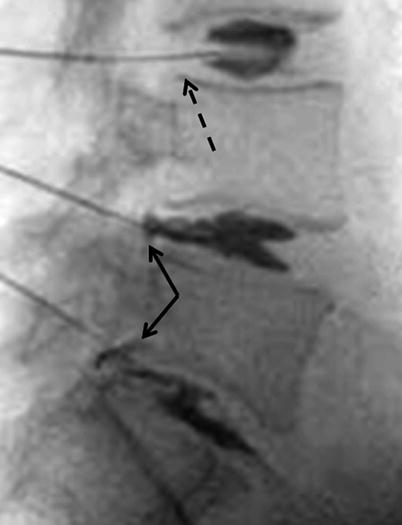
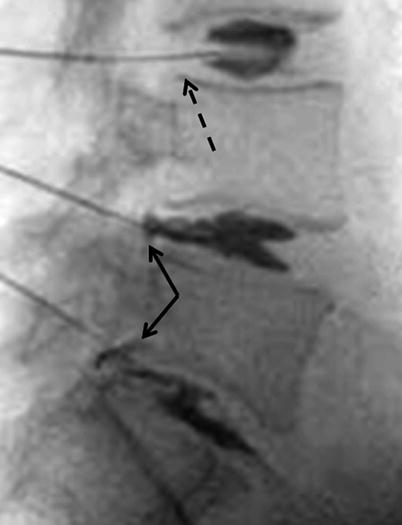
Fig. 13.2
A lateral lumbar fluoroscopic image obtained during a discogram. Needles are inserted into the L3–4, L4–5, and L5–S1 discs (in this specific case), and contrast dye is inserted under pressure into each of the discs. The L4–5 and L5–S1 levels (solid black arrows) demonstrate posterior leakage of the dye, indicating the presence of an annular tear at each of these levels. There is no dye leakage at L3–4 level (broken black arrow) as it all remains contained within the disc space, thus indicating the absence of a significant annular tear. If, while injecting the dye into a certain disc, the patient complains of pain similar to that which he/she experiences clinically, the disc that triggers such pain is said to cause concordant pain. This study is largely used in patients who are considering a surgical fusion for low back pain and is used to help decide which levels need to be fused, i.e., those levels which produce concordant pain on discography
13.2.5 Treatment of Discogenic Pain
The initial treatment of discogenic pain is nonsurgical. It is important to note, however, that the evidence available supporting various nonsurgical treatment options is limited (Ostelo et al. 2009; Thomas et al. 2006). For non-radicular low back pain, systematic review has shown no or insufficient evidence to support the use of botulinum toxin injections, local injections, prolotherapy, intraspinal steroid injections, epidural injections, facet joint or intradiscal steroid injections, sacroiliac injections or medial branch blocks, intradiscal electrothermic therapy, radiofrequency denervation, or spinal cord stimulation (Chou et al. 2007, 2009). There are “weak recommendations” from the American Pain Society for exercise, spinal manipulation, and interdisciplinary rehabilitation for chronic LBP or subacute LBP, as well as acupuncture, massage therapy, and yoga (Chou et al. 2007, 2009).
Despite these limitations, the initial treatment of discogenic LBP is nonsurgical and includes medication and physical therapy. Acetaminophen is effective for pain relief but has minimal anti-inflammatory effects. Hepatotoxicity may be encountered at high doses. Nonsteroidal anti-inflammatory drugs (NSAIDs) and COX-2 inhibitors are a mainstay in treatment as well. Opiate analgesics are more useful in treating chronic nociceptive pain and are rarely necessary in the treatment of acute pain. Muscle relaxants and antidepressants, particularly those that block norepinephrine, may provide analgesia. Physical therapy relies on mobilization, stretching, conditioning, and aerobic training. For discogenic low back pain, McKenzie extension-based exercise programs are the most beneficial. It is believed that these exercises will unload the disc by restoring lumbar lordosis and decreasing mechanical strain. Other recommendations include smoking cessation, weight loss, and activity alteration. The topic of nonsurgical treatment of low back pain is discussed in detail in Chap. 15.
Surgical interventions for discogenic disc disease are controversial and the results of high-level randomized studies are conflicting (Ostelo et al. 2009; Thomas et al. 2006; Chou et al. 2007, 2009). Surgery should not be considered until a structured 6-month regimen of physical therapy, NSAIDs, and activity modification has failed to improve the patient’s symptoms. In addition, it is important to rule out serious underlying pathology as the source of pain – it is necessary to screen for secondary pain, localize the pain to a specific region, and characterize the type of pain as mechanical versus myofascial. Brox et al. performed a single-blind randomized study to compare the effectiveness of lumbar instrumented fusion with cognitive intervention and exercises in patients with chronic low back pain and disc degeneration (Brox et al. 2003). At 1-year follow-up, there was equal improvement in patients with chronic low back pain and disc degeneration randomized to cognitive intervention and exercises, or lumbar fusion (Brox et al. 2003). Fairbanks et al. performed a randomized control trial to assess the effectiveness of spinal fusion versus intensive rehabilitation in patients with chronic low back pain. Over the 2-year follow-up, both groups reported statistically similar reductions in disability (Fairbank et al. 2005). A randomized controlled study was carried out to determine whether lumbar fusion could reduce pain and diminish disability more effectively than nonsurgical treatment in patients with severe chronic low back pain (Fritzell et al. 2001). Patients in the nonsurgical group were treated with different kinds of physical therapy. At 2 years, back pain was reduced in the surgical group by 33 % compared with 7 % (63 to 58) in the nonsurgical group (Fritzell et al. 2001).
Surgical options are largely limited to lumbar arthrodesis through an anterior, posterior, or combined approach. More recent options that are still under investigation include dynamic stabilization and total disc arthroplasty. Surgery is considered if the patient has failed a prolonged course of conservative management and there exists a strong correlation between clinical presentation and radiographic findings, and possibly discography. Posterolateral fusion has been shown to successfully manage chronic discogenic back pain in a highly selected subset of patients receiving worker’s compensation and those chronically disabled (Parker et al. 1996).
13.3 Intervertebral Disc Herniation
13.3.1 Epidemiology of Disc Herniation
Disc herniation is one of the most common intervertebral disc pathologies presented to spinal surgeons. Lumbar disc herniation has a peak incidence in the fourth decade of life, and men are more likely to be affected than women (Weinstein et al. 2008a, b). However, it is reported that only 4–6 % of lumbar herniations will become symptomatic (Weinstein et al. 2008a, b).
13.3.2 Pathoetiology of Disc Herniation
A cascade of degenerative changes occurs in the lumbar spine with age. The nucleus pulposus desiccates and loses its ability to recover from compressive deformation. In the annulus fibrosis, there are fissures that form between the collagen fibrils of the lamellae. With continued torsional, axial, and flexion strains across the disc, the nucleus pulposus can herniate through the fissures in the weakened outer annulus. The loss of nucleus pulposus containment alters the biomechanics of the entire disc. The annular fibrils become exposed to higher forces, which may lead to chondro-osseous changes at the disc–vertebral body junction. Details of these changes are presented in greater detail in Chaps. 7 and 19. A herniated nucleus pulposus can cause mechanical and/or chemical irritation of the affected nerve root and lead to severe radicular symptoms.
Disc herniation may have one of three morphological characteristics. A disc protrusion is defined as an eccentric bulging of the nucleus pulposus into an intact but thinned annulus. Disc extrusion occurs when disc material crosses through an annular defect but remains continuous with the disc space. A sequestered disc refers to one that is not continuous with the disc space and is a free fragment. Disc herniation can also be classified according to the location of the disc herniation in relation to the spinal canal, i.e., central, paracentral, foraminal, or far lateral. The most common location of disc herniation is paracentral, in which the herniated disc compresses the traversing nerve root (e.g., the L5 nerve root at the L4–5 disc level). A foraminal or far lateral disc will compress the exiting nerve root of the involved level (e.g., the L4 nerve root at the L4–5 disc level).
13.3.3 Clinical Presentation of Herniation
Most disc herniations are characterized by back and leg pain of varying severity and duration. Onset may be insidious or proceeded by a traumatic event. The L4–5 and L5–S1 discs are most commonly affected. Leg pain commonly occurs in the dermatome supplied by the compressed nerve root. Low back pain may subside after herniation because of the depressurization of the intervertebral space and relief of annular tension. Radiculopathy can present as pain, paresthesias, motor deficits, sensory deficits, and/or depressed reflexes. The distribution of symptoms (i.e., specific dermatome and myotome) often provides information as to the level of disc herniation than can then be correlated with the findings on MRI. Symptoms from a disc herniation are typically worse with sitting and improved with standing and walking. Sitting with the waist flexed not only causes an increase in the disc pressure but also causes the involved nerve to be stretched over the herniated disc. Often, paracentral and foraminal herniations will present with a predominance of leg pain, whereas central herniations often present with a predominance of back pain, as the central herniation, unless very large, does not directly compress the exiting or traversing nerve root.
A thorough evaluation and examination is needed for a patient with suspected disc disease. A detailed medical history includes investigation of possible serious underlying pathology, such as tumor, infection, fracture, or critical neurologic compromise. “Red flags” such as fever, chills, night pain, unrelenting pain, unexplained weight loss, progressive lower extremity weakness, and bowel or bladder dysfunction are indicative of a more severe and potentially emergent condition. These symptoms should prompt an expedited workup, including advanced imaging, such as an MRI. Family history may be informative as well as reports exist of a familiar and genetic predisposition to lumbar disc herniation. A full neurologic evaluation of muscle strength, sensation, proprioception, vibration, and deep tendon reflexes should be performed. Examination of patient standing position and gait may also provide useful information. A variety of maneuvers exist, such as the straight leg raise, to help diagnose a herniated disc.
13.3.4 Imaging of Herniation
Imaging studies are useful to confirm clinical diagnosis. Plain lumbar radiographs are of little benefit in the direct evaluation of a disc herniation, as they do not show soft tissue. However, they are indicated in patients with longer than 6 weeks of low back pain and in patients with medical history of serious underlying pathology, such as cancer or infection. Furthermore, radiographs (anteroposterior, lateral, flexion, and extension views) are helpful in evaluating a patient with lumbar degenerative disease for evidence of instability, disc collapse, and deformity (i.e., scoliosis). MRI is the diagnostic test of choice for evaluating a patient for a disc herniation (Fig. 13.3a, b). However, relatively high rates of lumbar disc herniations are found on MRI in asymptomatic patients (Boden et al. 1999a, b). Therefore, clinical correlation is of great importance. Dynamic MRI performed with patients in a variety of patients has begun to gain popularity. CT scan may be useful in specific situations, such as to assess bony anatomy in a patient who has had prior fusion surgery. CT myelogram is the study of choice in patients who cannot have an MRI. It is important to keep in mind when treating a patient with a symptomatic lumbar disc herniation that up to 90 % of patients will have gradual resolution of symptoms within 3 months of onset. For this reason, unless “red flags” exist, imaging is not indicated for at least 6 weeks following the onset of radiculopathy and low back pain.
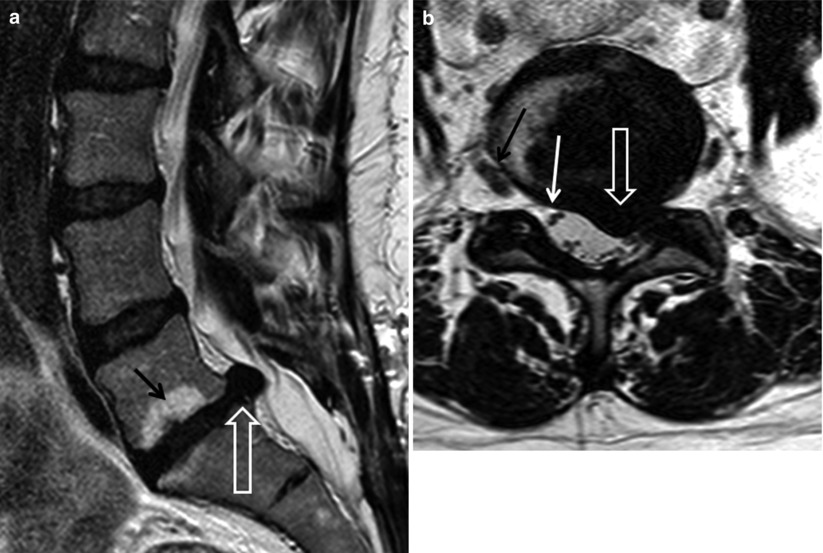
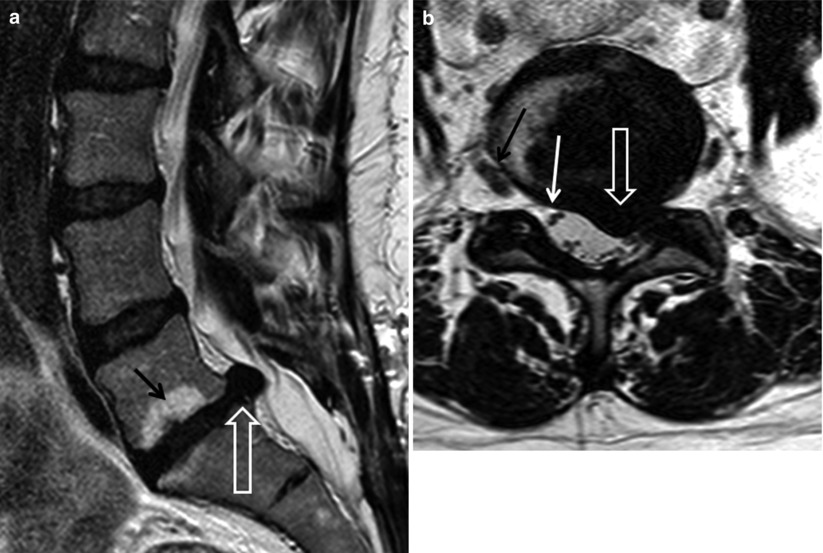
Fig. 13.3
Sagittal (a) and axial (b) T2-weighted lumbar MRI images demonstrating a left-sided L5–S1 paracentral disc herniation. On the sagittal image (a) the disc herniation is demonstrated by the open white arrow. The herniated disc can be seen protruding posteriorly into the spinal canal. The L5–S1 disc itself is considerably degenerated, and bone marrow edema (black arrow) is noted within this L5 vertebral body, adjacent to the inferior end plate, and, to a lesser extent, in the S1 vertebral body, adjacent to the superior end plate. This edema likely represents the bone response to abnormal load distribution that results from the degenerative disc. The axial image (b) demonstrates the location of the disc in the left paracentral region, extending somewhat into the left L5–S1 intervertebral foramen (open white arrow). The right exiting L5 nerve root (black arrow) and right traversing S1 nerve root (closed white arrow) are demonstrated. The exiting L5 and traversing S1 nerve roots on the left side are significantly compressed by the disc herniation
13.3.5 Herniation Treatment
Initial treatment for patients presenting with acute radicular symptoms is conservative. It involves a short period of rest, activity modification, and anti-inflammatory analgesia. Muscle relaxants and a short course of oral steroids have also proven beneficial. Physical therapy and spinal manipulation are used frequently as well. Fluoroscopic epidural steroid injections can be administered to reduce nerve root inflammation and significantly improve symptoms. Generally, conservative management is performed for at least 6 weeks.
Radicular symptoms not relieved by nonoperative methods are often treated by surgery to remove the herniated disc. Relative indications for surgery include intractable radicular pain, pseudoclaudication, neurologic deficit that does not improve with conservative treatment, recurrent symptoms following a successful trial of nonsurgical care, and significant motor deficit. Absolute indications include cauda equina disease or a progressive neurologic deficit.
The Spine Patient Outcomes Research Trial (SPORT) prospectively evaluated the outcomes of surgical versus nonsurgical intervention in patients with symptomatic lumbar disc herniation. Candidates with image-confirmed herniation meeting eligibility criteria were enrolled and randomized to standard open discectomy versus nonoperative care. At 4 years, patients who underwent surgery achieved greater improvement than nonoperatively treated patients (Weinstein et al. 2008a, b). Furthermore, it has also been demonstrated that with appropriate patient selection (i.e., symptoms and physical examination correlate to the findings on MRI), surgery provides faster resolution of symptoms and perceived quicker recovery than nonoperative management at 1–2 years (Weinstein et al. 2006; Peul et al. 2007).
Microdiscectomy is the gold standard surgical procedure for lumbar disc herniation. This procedure can be performed through a small incision in an outpatient setting. Complications of surgical intervention include inadvertent durotomy, nerve root injury, and infection. Later complications can include postoperative instability and recurrent disc herniation, which can occur up to 7 % of cases (Weinstein et al. 2008a, b). It is often difficult to discern recurrent disc herniation from epidural fibrosis on standard MRI imaging. Therefore, when evaluating for recurrent disc herniation, gadolinium-enhanced MRI should be used to differentiate between disc herniation and fibrosis.
13.4 Lumbar Stenosis
13.4.1 Epidemiology of Lumbar Stenosis
Lumbar stenosis refers to the narrowing of the neural canal and neuroforaminal spaces of the lumbar spine. It is the most common end-stage consequence of disc degeneration often resulting from adaptive changes of the facet joints and end plates. Most patients with symptomatic lumbar stenosis present between the ages of 60 and 80 (Johnson et al. 1992; Arbit and Pannullo 2001). Women are slightly more likely to have lumbar stenosis than men, and the majority of patients with lumbar stenosis are of Caucasian descent (Johnson et al. 1992; Arbit and Pannullo 2001). Degenerative spinal stenosis most commonly affects the L3–4 and L4–5 (Arbit and Pannullo 2001). Clinically, adults with radiographic evidence of lumbar stenosis may be asymptomatic; however, as age increases, a higher percentage becomes symptomatic (Johnson et al. 1992; Arbit and Pannullo 2001).
13.4.2 Etiology of Lumbar Stenosis
The most common cause of lumbar stenosis is age-related degenerative changes of the spine (Arbit and Pannullo 2001). End-stage lumbar disc degeneration alters facet and disc biomechanics and may induce hypertrophy and overgrowth of the facet joints and vertebral end plates, respectively. The resultant encroachment and the narrowing of the neuroforamina from osteophyte formation, loss of disc space height, and hypertrophy of the ligamentum flavum can cause marked reduction in space available for the spinal nerve roots.
Another cause of spinal stenosis is congenital lumbar spinal stenosis, which is associated with shorter pedicle lengths and innately narrowed spaces for neural elements in patients from birth. Instability associated with spinal stenosis most commonly occurs due to lumbar disc and/or facet degeneration and translation (spondylolisthesis) of the vertebra relative to each other. Instability can also result from the structural incompetence of the pars interarticularis (isthmic spondylolisthesis) or scoliosis. The shift forward, backward, or laterally can further reduce space in the spinal column centrally and/or foraminal spaces. Less common causes of lumbar spinal stenosis include epidural lipomatosis, tumors, infections, and metabolic bone disorders such as Paget’s disease. The main anatomic regions of lumbar stenosis include the central canal, lateral recess (subarticular), foraminal, and extraforaminal (Arbit and Pannullo 2001).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








