Surgical Dislocation of the Hip for Symptomatic Femoroacetabular Impingement
Christopher E. Pelt
Christina M. Khoury
Benjamin M. Stronach
Christopher L. Peters
Overview
Femoroacetabular impingement (FAI) is a condition that is defined as abnormal contact between the femoral head–neck junction and the acetabular rim. Specifically, the anterior superior head–neck junction of the femur abuts the anterior acetabulum (1). This condition is most commonly seen in the young to middle-aged adult population. Abnormal contact can lead to damage involving the labrum and/or articular cartilage (2,3,4) leading to early degenerative arthritis if not treated early in the disease process (2,5,6,7,8,9,10). The growing number of patients presenting with FAI have given orthopedic surgeons the opportunity to investigate the most effective means of treating this symptomatic condition. In the appropriately selected patient, open surgical dislocation of the hip has shown to be a safe and effective means of alleviating the presenting symptoms of hip pain and preserving the future health of the young adult hip joint. Open surgical treatment of FAI is directed at restoring a more normal femoral head–neck offset to alleviate femoral abutment against the acetabular rim and treating associated labral and articular cartilage damage. Direct visualization and full access to the joint allows a thorough assessment and correction of the underlying pathomorphology, and is the primary advantage of open surgical dislocation, compared to less invasive methods.
Presentation and Diagnosis
There is significant overlap in the presentation of patients with FAI who may be candidates for open surgical dislocation or other surgical approaches. Patients with hip impingement generally present anywhere from their late teenage years to their mid to late forties (11). The most common presenting complaint in patients with FAI is pain, typically in the anterior groin (12). However, pain can also be located in the lateral hip, the posterior buttock, and the lower back and the patient may demonstrate the “C-sign” (13). Although the patient may relate their symptoms to an acute or traumatic incident, the underlying morphologic abnormality of the hip has usually been present longer (11,12,13,14). A large majority of patients will also describe a mechanical-type symptom of catching or popping, attributed to an intra-articular problem such as a labral tear or chondral delamination (11). Although patients frequently are capable of performing their daily activities without difficulty, pain is usually associated with prolonged sitting, prolonged walking, and athletic activities. Activities that reproduce pain most frequently are ones that require deep flexion, such as squatting or ballet maneuvers (11,13). Patients may also describe a loss of hip range of motion, which may be noticeable in activities of daily living, such as putting on shoes and getting into and out of a car.
Physical examination of patients with symptomatic FAI should begin with an inspection of gait, palpation of the hip and surrounding area, an assessment of strength, hip range of motion, and provocative testing. Although patients will most commonly present with a normal gait, severe antalgia or Trendelenburg gait can indicate disease progression. Similarly, strength is usually preserved, but abductor weakness may be present in advanced cases. Assessment of hip range of motion, including flexion/extension, abduction/adduction, and internal/external rotation should be evaluated thoroughly and compared to the asymptomatic, contralateral limb. Limited internal rotation, frequently <15 degrees, with the hip flexed at 90 degrees is the most common finding. Patients may demonstrate obligate external rotation with hip flexion, known as “Drehmann’s sign (15).”
A positive impingement test is commonly present in patients with FAI (14). This examination is performed with internal rotation in 90 degrees of hip flexion and slight hip adduction (2,8). A positive test is associated with reproduction of the type and location of presenting groin pain. Limited internal rotation is also common and is because of impingement of the anterolateral femoral head–neck junction with the acetabular rim. In later stages of the disease process, posterior impingement can be seen. Posterior impingement is elicited in the prone position with the hip extended and externally rotated (16).
Radiographic assessment of FAI begins with a series of radiographs, which may include an AP pelvis, a false-profile view, Dunn lateral view, a modified Dunn lateral view, or a cross-table lateral of the hip (17,18). These imaging studies are used to evaluate joint space congruity, acetabular version, anterior and lateral femoral head coverage, acetabular inclination, and the contour and sphericity of the femoral head and the head–neck junction. In the setting of FAI, close evaluation of the femoral head and neck junction may reveal herniation pits or sclerosis, and may be present with cam-, pincer-, or combined-type FAI (2,19). Advanced imaging with magnetic resonance arthrography (MRA) is the preferred advanced imaging modality and allows for assessment of femoral and acetabular chondrolabral pathology. Recent advances with MRI, in the form of dGEMRIC, have provided the ability to further identify the extent of articular cartilage damage. Despite the added benefit of this imaging modality, studies by Mamisch et al. (20) have shown this to be a time-consuming process that may not yet be applicable for widespread use. Computed tomography (CT) with and/or without intra-articular contrast in the form of an arthrogram can prove useful in the evaluation, diagnosis, and surgical planning of FAI, particularly with identification of complex morphologic abnormalities.
For the subset of patients who present with groin pain but have no significant findings on physical examination and equivocal imaging studies, a fluoroscopically guided intra-articular hip injection of local anesthetic and corticosteroid can be performed, and may serve both a therapeutic as well as diagnostic role.
Indications and Contraindications
Because of the apparent relationship between FAI and hip arthritis (2,5,6,7,9,21,22), Ganz et al., among others, have advocated early surgical intervention in symptomatic hips (2,6,10,22,23). To this point, however, studies have not yet been able to prove a role for screening or prophylactic treatment of the condition. The current indications for open surgical dislocation of the hip include presence of symptoms for greater than 6 months, failure of response to conservative treatment, and clinical and radiographic findings consistent with the diagnosis of FAI. Conservative treatments typically include activity modification, rest, oral medications, injections, and physical therapy, though the value of these is questionable and may delay treatment of the underlying condition (24). Similar to the clinical presentation of patients with FAI, there is overlap in the patients who may be candidates for open surgical dislocation or other surgical treatments such as arthroscopy. In our practice, significant osseous or structural abnormalities on the acetabular or femoral side are relative indications to consider open treatment.
On the acetabular side, surgical hip dislocation is the preferred surgical approach for global acetabular overcoverage as seen with coxa profunda or severe pincer impingement. An extensive labral tear or pathology, or the presence of significant chondral delamination may also be indications given the direct visualization and access of the central compartment. On the femoral side, large cam deformities, especially lateral or anterolateral in location, are good candidates for open surgical dislocation of the hip because of the increased safe access to the lateral head–neck junction offered by open approaches. Other factors such as prior failure of mini-open or arthroscopic procedures are additional considerations in the decision to proceed with open surgical dislocation.
Contraindications for open surgical dislocation of the hip are related to the risk factors for complication or failure and include obesity, the presence of osteoarthritis or high-grade chondral lesions (Tönnis grade III or IV).
Treatment
The challenge for open treatment of FAI has been obtaining circumferential access to the femoral and acetabular pathoanatomy, without damaging articular cartilage or disrupting the blood supply to the femoral head. The various approaches to the hip have their own inherent limitations, making the appropriate surgical intervention challenging. The standard posterior approach to the hip places the medial femoral circumflex artery at risk. This is the major blood supply to the femoral head (25,26). The anterior Smith-Petersen approach to the hip allows for good visualization of the anterior aspect of both the acetabulum and the femoral head–neck junction. However, this approach does not allow for access to the superior lateral femoral neck or posterior acetabulum.
The first solution to these challenges was described by Ganz et al. (27) in 2001. He published the first treatment of FAI with a surgical dislocation of the hip. He described a lateral approach to the hip using a trochanteric flip osteotomy. A subsequent anterior capsulotomy and anterior dislocation allowed for circumferential exposure of the acetabulum and the majority of the femoral head and neck.
A more recent publication by Espinosa outlines a comprehensive surgical approach (28). We utilize a similar exposure and surgical technique with several modifications. We prefer general anesthesia with complete relaxation. The patient is placed in lateral decubitus position and the pelvis is stabilized with an adjustable post system. Once the patient is securely positioned and all nonoperative regions are well padded, a wide operative field from the ankle to the lower ribcage is prepared with an alcohol prescrub, a 2% chlorhexidine gluconate in 70% isopropyl alcohol scrub, and finally an iodine povacrylex (0.7% available iodine) in 74% isopropyl alcohol scrub. Sterile drapes are then placed to allow the operative leg to be manipulated and a sterile bag is positioned along the anterior portion of the patient. This allows the operative leg to remain sterile by placing it in the bag during dislocation as it drops below the level of the operative table.
The greater trochanter is fully palpated and the incision is centered over this landmark in both the anterior-superior and superior-inferior planes. Dissection is carried down through the subcutaneous fat to the level of the fascia overlying the gluteus maximus and the iliotibial band. At this point, we prefer to continue our dissection in a manner consistent with the initial portion of a posterior approach to the hip, which differs slightly from the Gibson approach utilized by Ganz et al. (27,28). We proceed by localizing the midline of the femur where we incise iliotibial band and dissect superiorly through the anterior fibers of gluteus maximus. A
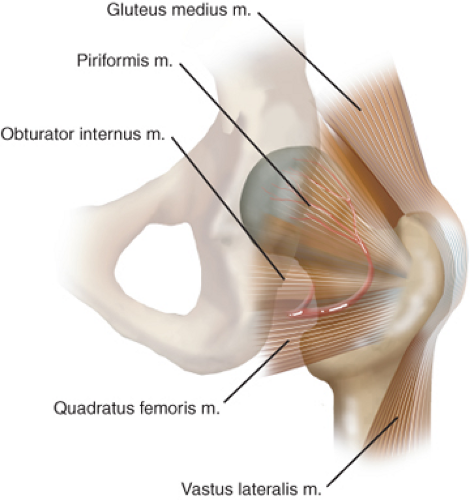
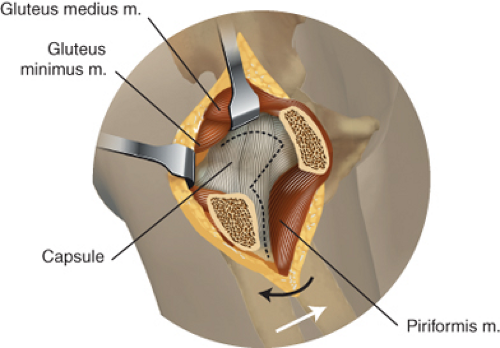
deep self-retaining retractor is placed and the operative leg is then slightly internally rotated to visualize the posterior portion of the hip. It is critical at this point to understand the anatomical structures involved before proceeding to ensure the blood supply to the femoral head is not injured. The posterior borders of the gluteus medius, greater trochanter, and vastus lateralis are identified. The fat overlying the external rotators is not disturbed and no dissection should be carried out in this specific region. We palpate the superior border of the piriformis and dissect the gluteus minimus from the capsule. Dissecting inferiorly into the piriformis fossa should be avoided, instead remaining at or above the cephalad edge of the piriformis tendon. The joint capsule is partially visualized in the interval between the gluteus minimus and the piriformis tendon and a bent Hohmann retractor is placed in this interval deep to the gluteus minimus and superficial to the capsule. We have found that the definition of this interval prior to the trochanteric flip makes later dissection much easier and less traumatic to soft tissues. We then turn our attention to the inferior border of the greater trochanter where the posterior border of the vastus lateralis is identified and elevated from the femur. A retractor is placed on to the anterior femur in this interval, allowing retraction of the vastus lateralis. The posterior margin of the greater trochanter is well visualized and the precise location of the trochanteric osteotomy can be determined.
deep self-retaining retractor is placed and the operative leg is then slightly internally rotated to visualize the posterior portion of the hip. It is critical at this point to understand the anatomical structures involved before proceeding to ensure the blood supply to the femoral head is not injured. The posterior borders of the gluteus medius, greater trochanter, and vastus lateralis are identified. The fat overlying the external rotators is not disturbed and no dissection should be carried out in this specific region. We palpate the superior border of the piriformis and dissect the gluteus minimus from the capsule. Dissecting inferiorly into the piriformis fossa should be avoided, instead remaining at or above the cephalad edge of the piriformis tendon. The joint capsule is partially visualized in the interval between the gluteus minimus and the piriformis tendon and a bent Hohmann retractor is placed in this interval deep to the gluteus minimus and superficial to the capsule. We have found that the definition of this interval prior to the trochanteric flip makes later dissection much easier and less traumatic to soft tissues. We then turn our attention to the inferior border of the greater trochanter where the posterior border of the vastus lateralis is identified and elevated from the femur. A retractor is placed on to the anterior femur in this interval, allowing retraction of the vastus lateralis. The posterior margin of the greater trochanter is well visualized and the precise location of the trochanteric osteotomy can be determined.
The osteotomy starts superiorly at the posterior border of the gluteus medius and is carried inferiorly to the posterior margin of the vastus lateralis (Fig. 41.1). The plane of the osteotomy is parallel to the calf to ensure the osteotomy site is parallel to the alignment of the femur. The wafer of bone is approximately 1.5 cm thick but this will vary slightly based on the patient’s body habitus and osseous anatomy. After the osteotomy is completed, we place granular collagen/thrombin on the osteotomy site to improve visualization and decrease blood loss for the remaining portion of the procedure. Proximally, gluteus medius and a portion of minimus remain attached and distally, the vastus lateralis remains attached to the osteotomy fragment, allowing these structures to be retracted anteriorly. A provisional retractor is placed over the anterior femoral neck and capsule whereas the leg is externally rotated gently to increase the exposure of the anterior capsule. The dissection is continued with electrocautery, releasing the adherent fibers of rectus femoris and any remaining gluteus minimus. Once the capsule can be visualized, we palpate the acetabular rim and femoral head to ensure adequate exposure and replace the provisional retractor with a large bent retractor. The exposure is continued to include the anterior-inferior capsule and medially to the border of the iliopsoas tendon.
Once exposure of the capsule is complete, we then perform a Z capsulotomy (Fig. 41.2). The first incision is placed longitudinally down the anterior femoral neck. The second incision is started at the distal margin of the first incision and carried anteriorly along the intertrochanteric line, releasing the inferior margin of the anterior capsule from the inferior neck. We then return to the superior margin of our first incision and continue this capsulotomy superiorly with intra-articular visualization of the labrum to prevent injury. Once this incision is cephalad to the labrum, the third incision is made by releasing the capsule along the acetabular rim in a posterior direction.
With the hip capsule now open, the appearance of the head–neck junction and labrum is inspected. The hip can then be flexed and internally rotated to identify the area of impingement. Frequently, there is visible damage on the
anterior femoral neck to include periosteal blushing consistent with ecchymosis and osseous reaction (Fig. 41.3



anterior femoral neck to include periosteal blushing consistent with ecchymosis and osseous reaction (Fig. 41.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree