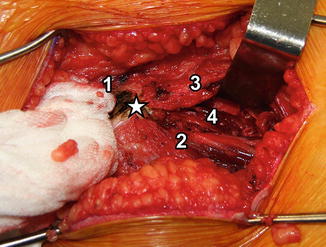
Fig. 1
Overview of skin incision and the underlying muscles (Figure taken with permission from “Periacetabular osteotomy in the treatment of severe acetabular dysplasia. Surgical technique.” Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. J Bone Joint Surg Am. 2006 Mar; 88 Suppl 1 Pt 1:65–83)
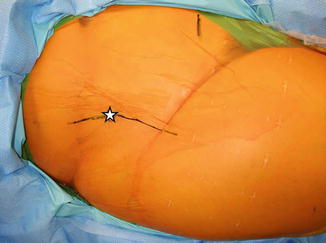
Fig. 2
Skin incision. The skin incision is located over the iliac crest proximally and the palpable anterior border of the tensor fascia latae muscle belly distally. Star, anterior superior iliac spine; black line, skin incision
The original incision described by Ganz uses the skin incision of the Smith-Petersen approach [1, 2]. The incision is started along the gluteal tubercle of the iliac crest and then turned at the level of the ASIS to follow the course of the underlying tensor fascia latae muscle fibers. Proximally, the incision is made over the iliac crest and just lateral to the ASIS to avoid a painful surgical scar formation over bony prominences and to avoid injuring the lateral femoral cutaneous nerve which runs just medial to the ASIS deep to the inguinal ligament. Some surgeons advocate at this stage to identify and dissect out the lateral femoral cutaneous nerve to avoid its entrapment during closure of the incision; however, it is sufficient to keep the dissection lateral to it so that the nerve remains uninjured in the more medial soft tissues.
Alternatively in thin patients, the incision does not have to angle at the ASIS but can remain straight and follows the course of the inguinal ligament just distal to it. This type of incision allows for a more cosmetic “bikini line” scar but makes the subsequent steps of the surgical approach more difficult especially in more muscular or obese patients.
Deep Dissection
Proximally, the interval between the origin of the tensor fasciae latae muscle and the abdominal muscle aponeurosis consistent of the external oblique, internal oblique, and transverse muscle layers is identified (Fig. 3). As the abdominal muscle aponeurosis wraps around the iliac crest, this interval is located proximally just distal to the iliac crest and at the level of the ASIS right over the iliac crest. The interval is incised down to the periosteum, and dissection is carried out towards the inner iliac table just across the iliac crest leaving the origin of the tensor fasciae latae untouched. In the early developmental phases of the this approach, Ganz et al. have detached the origin of the tensor fasciae latae of the anterior part of the outer pelvic table [1]; however, they have later on abandoned it as it was deemed unnecessary [3, 4].
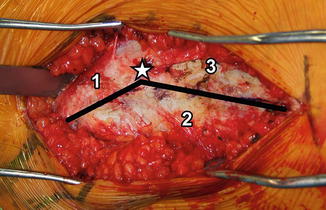
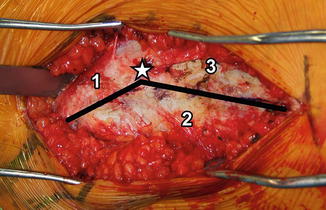
Fig. 3
Fascial incision. Proximally, the facial incision is located over the iliac crest where the abdominal muscle fascia meets the origin of the tensor fascia latae. Distally, the fascial incision lies over the anterior border of the tensor fascia latae muscle belly. Star, anterior superior iliac spine; black line, fascial incision; 1, external oblique abdominal muscle; 2, tensor fasciae latae; 3, sartorius femoris
Care is taken not to cut into the external oblique muscle belly which forms the superficial layer of the abdominal muscle aponeurosis and to remain subperiosteal to avoid unnecessary bleeding. At this point the dissection of the iliacus muscle from the inner pelvic table is continued. As the periosteum thins out on the inner pelvic table, the dissection of the iliacus origin from the inner pelvic table can be associated with substantial blood loss from blood vessels from the muscle belly as well as the nutrient artery of the ilium which is a branch of the superior gluteal artery and enters the ilium approximately 2 cm anterior to the sacroiliac joint and 2 cm proximal to the pelvic brim [5, 6]. Inevitably the nutrient vessel of the ilium is severed and bone wax is necessary for hemostasis. Dissection is carried out along the inner table of the pelvis until the pelvic brim is visualized. This area can be packed with lap pads to allow hemostasis to occur while the more distal dissection is completed.
Next, further distal dissection is performed. The fascia over the tensor fascia lata muscle belly is incised just posterior to the anterior edge of the muscle belly. The tensor fascia lata muscle belly can sometimes be difficult to identify, and it is advisable to err posteriorly. The interval between the sartorius and the tensor fasciae latae is easier to identify proximally near the ASIS. A helpful landmark is a leash of vessels at the posterior aspect of the tensor fasciae latae muscle belly which pierces the fascia to supply the overlying skin [7]. The fascia lata itself is posterior to the tensor fasciae latae muscle belly. The dissection is too posterior if the surgeon encounters increased bleeding or visualizes the fascia lata at this stage. After proper incision of the fascia over the tensor fasciae latae at its anterior edge, the muscle belly is retracted laterally within its sheath. Proximally, a tissue sleeve including the sartorius and the inguinal ligament is dissected off the ASIS (Fig. 4). Alternatively, as originally described by the ASIS can be osteotomized with the origin of the sartorius and the inguinal ligament. The fascia at the floor of the tensor sheath is incised exposing the rectus femoris. The sartorius is retracted medially fully exposing the rectus. Dissection between the rectus femoris and the sartorius is carried out (Fig. 4). After release of the sartorius, exposure of the inner table of the supraacetabular region, iliopectineal eminence, and superior pubic ramus continues from lateral to medial (Fig. 5). It is important to remove all periosteal and soft tissue connections to the brim of the acetabulum, quadrilateral plate, and proximal portion of the superior ramus; otherwise, these will interfere with the mobility of the fragment after the osteotomies are performed. The origin of the straight head of the rectus from the anterior inferior iliac spine is visualized. Medial to the rectus femoris, the iliopsoas is visualized as it comes across the pelvic brim. The fascia overlying the psoas is carefully incised to allow increased mobilization of the psoas. This fascia should be divided under direct visualization distally, as the femoral nerve will lie directly under the fascia. At this point the hip is hyperflexed and adducted to relax the iliopsoas muscle. The iliopsoas has contributing muscle fibers that originate from the anterior hip capsule. Those muscle fibers have been named the iliocapsularis muscle [8]. Dissection is carried out medial to the straight head of the rectus femoris and lateral to the iliocapsularis and iliopsoas. The iliocapsularis muscle fibers are dissected off their origin at the anterior hip capsule. Dissection is carried out between the hip capsule and the iliopsoas proximal to the crossing fibers of the obturator externus down to the subcotyloid groove of the ischium just inferior to the posterior horn of the acetabulum. This is done somewhat blindly and is most easily performed by directing a curved Mayo scissors between the capsule over the femoral neck and the psoas until the ischium is encountered. This is typically deeper and more medial than expected. Fluoroscopic guidance is often helpful in locating the anterior edge of the ischium for those with less experience in the procedure. Care is taken not to stray medially as the obturator neuromuscular bundle is close as it exits the inner pelvis underneath the obturator canal and pierces the obturator membrane. In a study of 29 cadaveric hemipelvises, the distance between the inferior ischial osteotomy site and the obturator artery has been shown to be an average of 36mm with a minimum of 22 mm [9]. It is also important to not dissect distal to the cephalad margin of the obturator externus in order to not jeopardize the medial femoral circumflex artery which constitutes the main blood supply to the femoral head [10]. Optionally, the straight head of the rectus femoris muscle can be taken off the anterior inferior iliac spine to facilitate the exposure; however, in our opinion that is not routinely necessary. It can be useful to perform a capsulotomy to assess the labrum and the femoral neck offset for possible impingement after the acetabular correction.