Introduction
The lower limbs are the supporting pillars when we stand. A pillar must have strength and must not collapse under the weight above. The bones, joints and muscles together convert the lower limb into a stable support which is linked to the trunk by the pelvic girdle. The pillar is divided into segments, the thigh, leg and foot. The segments are linked by joints, the hip, knee, ankle and joints of the foot, which can adjust to the changes that occur in the line of weight through the limbs as the head and trunk move above. The muscles around the joints counteract the effects of gravity and any external forces that disturb the balance of the body.
Locomotor movements require the lower limbs to support the weight of the head, arms and trunk above while the body is propelled forwards. The limbs perform repetitive movements of one limb in support while the other limb swings forward. This alternation of swing and support means that each limb as a whole must combine strength with mobility. The pattern of movement must also adapt to walking sideways, up and down slopes and different textures of the ground.
In functional activities, for example getting out of bed and getting up from a chair, the lower limbs are active in transferring the body from one position to another. Weakness of muscles or loss of joint mobility makes these transfer activities difficult and the upper limb then has to compensate (see Chapter 5, Figure 5.14b).
Information from pressure receptors in the skin of the sole of the foot and from the proprioceptors in all the muscles of the lower limb plays an important role in maintaining the balance of the upright body. Feedback from these receptors maintains an economical pattern of locomotion.
In summary, the overall functions of the lower limb are to provide:
- transfer of the body from lying to sitting, to standing;
- support for the head, arms and trunk in all upright positions and movements;
- propulsion in walking, running and climbing stairs;
- sensory information for posture and balance.
Joints and movements of the pelvis, thigh and leg
The pelvis forms the link between the vertebral column and the thigh for the transmission of the body weight downwards from the trunk to the hip and knee joints, and on to the feet. The joints of the thigh and the leg combine to give stability for support of the upright body and adequate range of movement for the limb as a whole.
Movements at the hip allow the thigh to move in the frontal, sagittal and transverse planes. The knee, like the elbow, moves mainly in one plane (sagittal), and allows shortening of the lower limb so that the foot can clear the ground in walking. The ankle is important in placing the foot on different surfaces of the ground for support and then initiating the propulsion of the body forwards.
The pelvic girdle: position and function
The pelvis or pelvic girdle is an irregular ring of bone composed of the two innominate bones and the sacrum formed by five fused vertebrae. Each innominate bone is made up of the ilium, ischium and pubis, which fuse at the socket for the hip joint. The ilium extends upwards and ends at the iliac crest, which can be felt when placing ‘hands on hips’. The ischium lies inferiorly and ends with a roughened ischial tuberosity, which can be felt when sitting upright on a hard seat. The pubis on either side meets in the midline to complete the ring of bone anteriorly. The sacrum articulates superiorly with the fifth lumbar vertebra at the lumbosacral joint.
The stability of the pelvis is provided by strong ligaments binding the innominate bone to the sacrum anteriorly and posteriorly. The bony pelvis provides a base for the attachment of muscles of the trunk and the hip. The anterior abdominal muscles end in an aponeurosis which is thickened inferiorly to form the inguinal ligament, extending from the anterior end of the iliac crest to the pubis in the midline. This forms an anatomical space for the passage of nerves and blood vessels from the trunk to the thigh anteriorly.
The bony pelvis, together with the muscles lying across its floor (see Chapter 10), support and protect the reproductive organs, the bladder and the rectum. During childbirth, the pelvis adapts to increase the diameter of the canal for the passage of the head of the baby.
Joints of the pelvis
The sacroiliac joint between the sacrum and the ilium of the innominate bone is a joint that is part synovial and part fibrous. The ear-shaped irregular joint surfaces, on the posterior medial part of the ilium and the upper lateral side of the sacrum, fit closely. The joint is bound by anterior and posterior ligaments. The thin joint cavity often becomes fused by fibrous bands with age. The two innominate bones join anteriorly at the pubic symphysis, a secondary cartilaginous joint.
Only limited gliding movements are possible at these joints. Mobility has been sacrificed for the stability required to resist the high level of forces on the pelvis in walking, running and jumping.
Movements of the pelvis as a whole change the tilt of the innominate bones. The ilium moves forwards and the ischium moves backwards in anterior forward tilting of the pelvis. The reverse occurs in backward tilting. The posterior muscles of the hip and the anterior abdominal wall produce these movements (see Chapter 10). Pelvic tilting also occurs in response to the tension in the hamstring muscles, which originate on the ischial tuberosities and pass down the posterior aspect of the thigh to the knee.
The hip joint
The hip joint, like the glenohumeral joint at the shoulder, is a synovial joint of the ball and socket type, but there the similarities end. The shoulder joint is designed for mobility, but the hip joint has to fulfil two functions, those of mobility and stability. The socket of the hip joint is formed by the acetabulum, meaning ‘little vinegar cup’. The acetabulum lies at the side of the pelvis and is a deep, outwards-facing cup surrounded by a rim of fibrocartilage, known as a labrum. The head of the femur forms the ball, which is two-thirds of a sphere. When the ball is in the socket, the labrum curves inwards beyond the equator of the head of the femur to grip it and help to hold it in place.
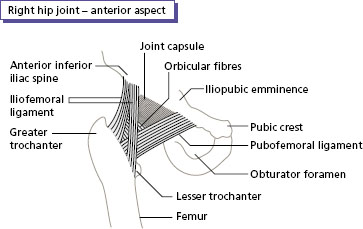
The hip joint has a strong capsule that includes most of the femoral neck. The capsule is further strengthened by very strong ligaments anteriorly, and by small half rotator cuff muscles posteriorly. ThFe iliofemoral ligament is the strongest in the body; it is Y-shaped, passing across the front of the joint (Figure 8.1). This ligament limits the range of extension of the hip and therefore can be used to support the trunk on the lower limb. Stability is also assisted by circular fibres within the capsule, called the orbicular fibres, which give the capsule a ‘waist’, so increasing the suction effect of the cup on the head of the femur (Figure 8.1).
The movements of the hip joint are as follows:
- Flexion carries the thigh forwards in the sagittal plane, as in the leg swing in walking and lifting the foot on to the step above in climbing stairs.
- Extension is the return movement from flexion and continues beyond the anatomical position to place the foot behind the body. Extension raises the body from sitting to standing, and up on to the step above in climbing stairs.
- Abduction carries the thigh sideways in the frontal plane to step to the side.
- Adduction is the return movement from abduction and also carries the foot across the body.
- Medial and lateral rotation turn the femur inwards and outwards. These movements turn the foot inwards and outwards as there is no rotation at the knee.
Figure 8.1 Hip joint, right anterior view.
The knee joint
The knee is a large, complex synovial joint, which may be called an atypical hinge joint. The main axis of movement flexes and extends the leg on the thigh, but there is some rotation at the knee when the knee is flexed and the foot is off the ground.
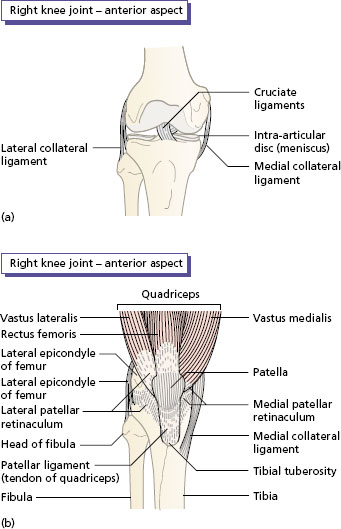
The rounded condyles of the femur articulate with the shallow, saucer-shaped condyles of the tibia. Note that the fibula is not included in the joint. A fibrocartilaginous semicircular disc, known as a meniscus, lies on each of the tibial condyles (Figure 8.2a). The menisci have four important functions within the knee: (i) to increase congruence between the femur and the tibia; (ii) to act as shock absorbers as the body weight falls on to the tibial plateau; (iii) to assist in weight bearing across the joint; and (iv) to aid lubrication by the circulation of synovial fluid within the knee joint.
The knee joint has strong collateral ligaments, and an obique ligament that passes posteriorly across the joint. The medial collateral ligament is a broad band, the posterior margin of which is attached to the medial meniscus. The lateral collateral ligament is a round cord which is mobile and not attached to the capsule or the lateral meniscus. Anteriorly, the knee joint is strengthened by the tendon of the anterior muscle of the thigh (quadriceps) as it passes over the patella to be inserted into the anterior tubercle of the tibia (Figure 8.2b).
Within the knee joint, there are two further very important ligaments. These are attached to the centre of the tibial plateau and pass upwards to attach within the intercondylar notch of the femur (Appendix I). They appear to cross one another and so they are called the cruciate ligaments (Figure 8.2a). The position of the cruciate ligaments in the centre of the joint means that they prevent the femur rolling off the tibia. The cruciate ligaments also form a fulcrum for the ‘locking action’ of the knee, which occurs when the femur rotates slightly medially at the end of full extension.
The movements of the knee joint are as follows:
- Flexion is the movement in the sagittal plane that bends the leg towards the thigh. The knee flexes when the leg is lifted up to the next step in climbing stairs, and when sitting in a crouched position or cross-legged.
- Extension straightens the leg from the flexed position to the anatomical position. When the foot is fixed by the ground, there is some rotation at the end of the range into full extension, and at the start of flexion, owing to the shape of the condyles of the femur.
Figure 8.2 Knee joint, right anterior view: (a) patella, capsule and quadriceps removed; (b) intact.
- The medial meniscus tears and splits through its length. The torn portion sometimes becomes displaced and lodged between the femur and the tibia.
- The medial ligament is most commonly torn, and in severe cases the anterior cruciate ligament is involved as the tibia rotates laterally. Less commonly, the lateral ligament is torn, and the posterior cruciate ligament tears when the tibia is forced backwards in relation to the femur.
The ankle joint
The ankle joint is a synovial hinge joint. The articular surfaces of the ankle joint are the upper surface of the talus bone of the foot and the inferior surface of the tibia. The weight-bearing surfaces are the curved trochlear of the talus and the reciprocal shallow notch of the tibia. Stabilising surfaces are the medial malleolus of the tibia and the lateral malleolus of the fibula, which provide a firm grip on the sides of the talus, creating a bony mortice and tenon joint.
The medial collateral ligament (also known as the deltoid ligament) is very strong and fan-shaped (Figure 8.3a). Its attachment to the navicular bone of the foot makes it an important support mechanism for the medial arch of the foot. The lateral ligament has three bands binding the lower end of the fibula to the talus and the calcaneum (Figure 8.3b).
The movements of the ankle joint are described with reference to the neutral position, which is the position of the foot in the normal standing position, when the foot makes a right angle with the leg.
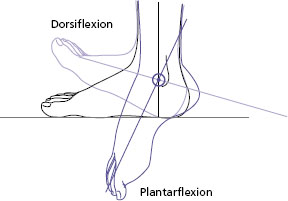
Dorsiflexion is when the foot is drawn upwards towards the leg (Figure 8.4). Dorsiflexion of the ankle lifts the toes clear of the ground when the leg is swinging forwards in walking or kicking a ball.
Plantar flexion when the movement is in the opposite direction from the neutral position (Figure 8.4). Plantar flexion lifts the heel off the ground to give propulsion forwards in walking, and upwards in standing on the toes. The ankle is least stable in the plantar flexed position.
- Sit with the foot off the ground. Start with the foot at right angles to the leg. MOVE the ankle through dorsiflexion (toes up) and then plantar flexion (toes down).
- Stand upright and lift the body up on to the toes. Note how this is a plantar flexion movement at the ankle.
Figure 8.3 Ankle joint, right: (a) medial view; (b) lateral view.
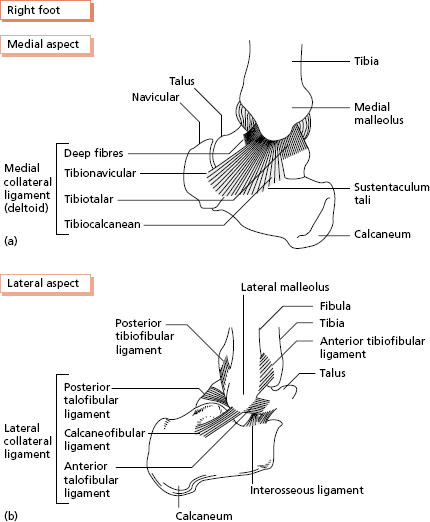
Figure 8.4 Movements of the ankle: dorsiflexion and plantar flexion.
Muscles of the thigh and leg in support, swing and propulsion
The muscles of the leg and thigh will be described under three headings related to their function in support, swing and propulsion.
The support muscles convert the lower limb into a pillar, either single or double, in standing, walking and negotiating stairs.
The muscles involved in swing carry the lower limb forwards, backwards, sideways or upwards while the opposite limb is in support.
Propulsion muscles exert forces on the ground to propel the body horizontally or upwards in walking, jumping or climbing stairs.
Support
There is a remarkable economy of muscle activity involved in standing upright on two legs. The joints of the lower limb are in a close-packed position when standing, and stability depends largely on the tension of the ligaments around the joints. Two particular structures are important.
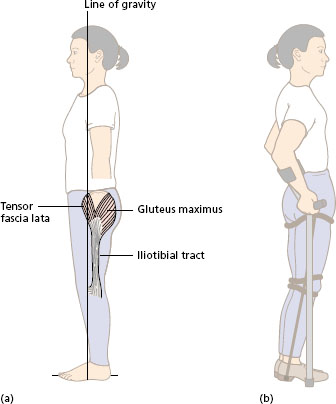
The anterior ligament of the hip joint, the iliofemoral ligament (Figure 8.1 ) is important in resisting the tendency for the trunk to fall backwards on the lower limbs when the line of the body weight falls behind the hip joint. Little activity is required in the hip flexors and extensors. The paraplegic with paralysed hip muscles learns to place the hips well in front of the line of gravity and relies entirely on the tension in the iliofemoral ligament for stability at the hips in standing (Figure 8.5a).
The iliotibial tract (also known as the fascia lata) is a band of dense fascia that extends across the hip and knee on the lateral side of the thigh. In standing, the tension in a small muscle, known as the tensor fascia lata, which originates on the anterior superior spine of the ilium and inserts into the iliotibial tract, keeps the hip and knee extended, with the help of the gluteus maximus, the large superficial muscle of the buttock (Figure 8.5b).
People rarely stand to attention like guardsmen on parade, but adopt changing positions of ‘slack standing’ with the knees slightly flexed and the weight shifting from one leg to the other.
Figure 8.5 Upright standing: (a) iliotibial tract, line of gravity; (b) paraplegic standing.
Muscles of the hip in single support
In standing on one leg, the muscles around the hip of the supporting leg are active to move the body weight over the supporting leg; and to prevent the pelvis from dropping on the unsupported side.
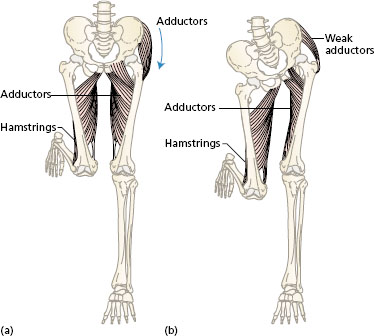
The adductor group of muscles on the inside of the thigh contracts to shift the pelvis over the supporting leg. At the same time, the tendency for the pelvis to drop is counteracted by activity in the abductors of the hip in the supporting leg. Figure 8.6a shows the position of the abductors and adductors in the supporting leg. Contraction of the abductors will pull on the pelvis and keep it level. Further tilt of the pelvis gives added clearance for the raised foot.
The abductors of the hip are the gluteus medius and gluteus minimus.
Two fan-shaped muscles lie deep to the gluteus maximus, the largest muscle of the buttock. Gluteus medius and minimus originate from the outer surface of the ilium, and both muscles insert into the greater trochanter of the femur (Figure 8.7).
Figure 8.6 Single support: (a) action of the hip abductors and adductors to keep the pelvis level; (b) Trendelenburg’s sign.