8
Supporative Flexor Tenosynovitis
John C. P. Floyd and Waldo E. Floyd III
History and Clinical Presentation
A 52-year-old insulin-dependent diabetic man presented to his primary care physician 4 days after sustaining a palmar stab wound while sharpening a knife. Due to swelling and erythema about the wound overlying the palmar aspect of the fourth metacarpophalangeal joint, the patient was admitted to the hospital and placed on parenteral cefazolin. Significant medical history included insulin-dependent diabetes mellitus, peripheral vascular disease, and coronary artery disease. Bilateral above the knee amputations, multiple coronary artery bypass grafts complicated by wound healing problems, and drug allergies to vancomycin, sulfa, doxycycline, clindamycin, and ceftazidime characterized his medical history.
The patient had undergone a limited incision and drainage procedure by an orthopedic surgeon in the palmar wound just proximal to the A-1 pulley. The flexor tendons were reported to have been intact. Purulent fluid had been expressed from a rent in the flexor tendon sheath. The sheath was further incised and irrigated through a pediatric feeding tube. Purulent material was obtained for cultures and sensitivities. Despite oral amoxicillin management, purulent drainage and erythema persisted, prompting hand surgery referral.
Physical Examination
On presentation to the hand surgeon, the palmar wound was draining serous fluid and there was no flexor tendon function (Fig. 8–1). Flexor tendons were visible within the wound, with a significant amount of surrounding nonviable tissue. Further surgical intervention was deemed appropriate.
Diagnostic Studies
Anteroposterior and lateral radiographs of the left hand were positive for arterial calcification and soft tissue swelling.
PEARLS
- Early diagnosis followed by early antibiotic and surgical intervention
- Adequate drainage of infection
- Appropriate antibiotic management based on cultures
PITFALLS
- Necrotic tissue removal necessary
- Complications result from inadequate drainage of infection
Differential Diagnosis
Posttraumatic nonspecific inflammation
Cellulitis
Pyogenic, fungal, or mycobacterial infection
Flexor tendon sheath infection with rupture of the flexor tendons
Septic arthritis
Osteomyelitis
Foreign body
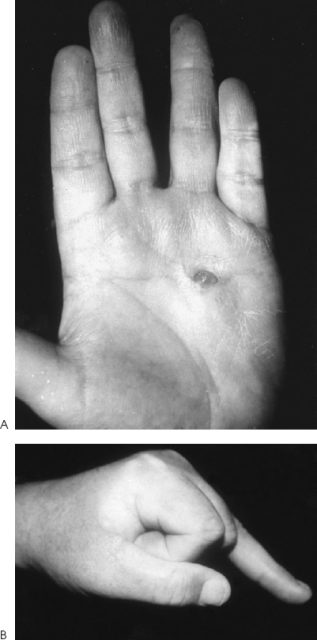
Figure 8–1. (A) Ongoing palmar drainage and lack of wound healing following limited palmar drainage of suppurative ring finger flexor tenosynovitis. (B) Due to rupture of necrotic flexor tendons, the digit rested in full extension, rather than the characteristic semiflexed posture of flexor tenosynovitis.
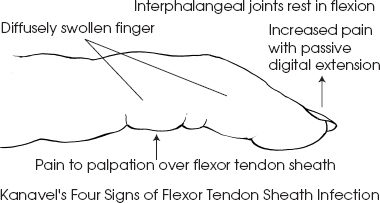
Diagnosis
The diagnosis was flexor tendon rupture secondary to suppurative flexor tenosynovitis. Kanavel outlined the four classic, cardinal signs of digital flexor tenosynovitis: (1) fusiform digital swelling, (2) semiflexed digital posture, (3) significant pain associated with passive extension of the digit, and (4) exquisite tenderness along the entire flexor tendon sheath (Fig. 8–2). All four signs are present in an advanced case and a combination of one or more signs is found in less severe cases. However, in this case, the semiflexed posture was not present as the flexor tendons had ruptured secondary to the advanced process.