CHAPTER 18 Superior Labrum Anterior and Posterior (SLAP) Tears
Pathology of the superior glenoid labrum and bicipital tendon insertion can present as chronic shoulder pain and yield subtle findings. In 1985, Andrews initially described this type of pathology in throwing athletes.1 Superior labrum anterior and posterior (SLAP) lesions, originally referred to by Snyder as superior labrum anterior and posterior lesions, were classified by Snyder in 1990.2 This initial classification was later expanded to include a total of 10 SLAP subtypes.3,4 Whereas this classification has enabled surgeons to approach SLAP lesions systematically and study them more thoroughly, difficulty lies in the preoperative diagnosis and differentiating symptomatic superior labral pathology from normal variants. The difficulty is compounded by the natural degenerative changes that occur in the labrum with advancing age.5 In addition, the accepted mechanisms of injury are as different as the different types of SLAP pathology.6 Included in this chapter are the current SLAP tear classifications and a systematic approach to diagnosis and treatment.
ANATOMY AND PATHOANATOMY
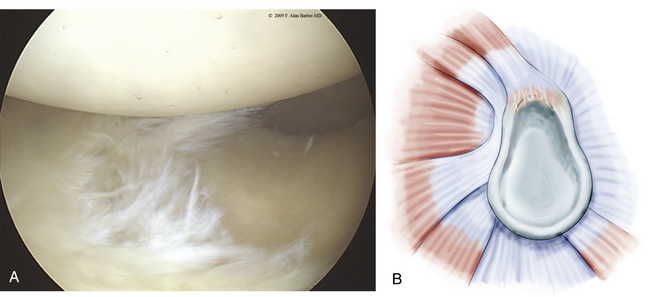
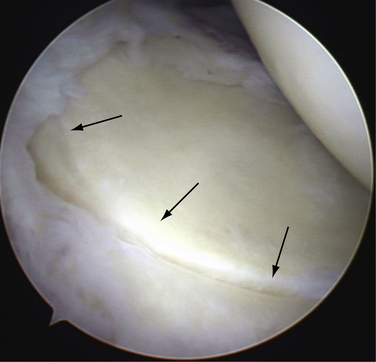
With the increased acceptance and improved techniques of shoulder arthroscopy, clinically significant SLAP lesions have become more distinguishable from normal anatomy. As noted, Snyder’s initial classification of SLAP lesions was expanded to include 10 SLAP subtypes.2–4 Type 1 SLAP lesions have fraying on the inner margin of the superior labrum (Fig. 18-1). These are likely to represent normal degenerative changes and the retreat of blood supply from the superior labrum associated with normal aging.5 Occasionally, a meniscus-like superior labrum (meniscoid labrum, a normal variant) can have similar degenerative fraying of the inner rim and can also be classified as a type 1 lesion; it is the most frequently encountered type.
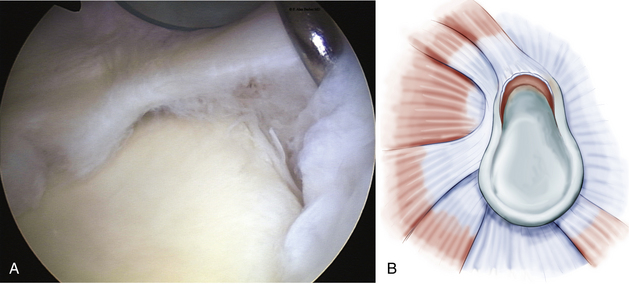
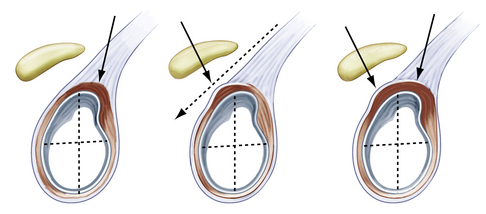
In a type 2 SLAP (Fig. 18-2), which is the most common clinically significant lesion,2,7–9 the superior labrum is pulled off the superior glenoid tubercle at the bicipital attachment. Three subtypes have been described by Morgan and colleagues,10 including anterior, posterior, and combined anterior and posterior (Fig. 18-3). The anterior variant is the most common type 2 SLAP in throwing athletes, but the posterior variant is also commonly seen in the same population. Combined avulsion from both anterosuperior and posterosuperior quadrants of the glenoid is the least common subtype encountered.
The peel-back phenomenon initially described by Burkhart and Morgan11 occurs when the labrum detaches and slides medially or peels off the posterior superior glenoid because of the force transmission of the biceps tendon origin. This pathology may be demonstrated by placing the shoulder into abduction and external rotation while viewing arthroscopically.
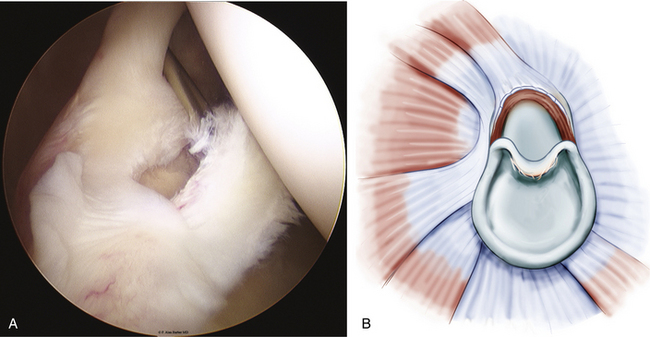
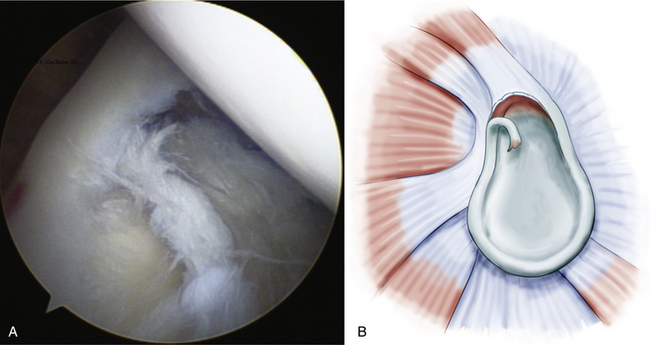
Type 3 SLAP lesions usually extend from anterior to posterior with a bucket handle tear configuration (Fig. 18-4). Type 3 differs from type 2 because there is no elevation of the biceps-labral attachment from the glenoid. The type 4 SLAP is a bucket handle labral tear that extends into the biceps tendon, resulting in a split in the tendon attachment (Fig. 18-5).
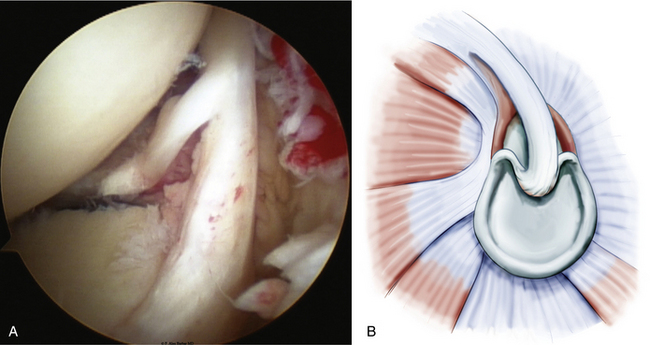
FIGURE 18-5 The type 4 SLAP lesion is a bucket handle labral tear (A) that extends into the biceps tendon, resulting in a split in the tendon attachment (B); left shoulder, posterior portal, lateral decubitus position.
(B from Powell SE, Nord KD, Ryu RK. The diagnosis, classification and treatment of SLAP lesions. Oper Tech Sports Med. 2004;12:99-110.)
Classifications of labral pathology that include shoulder instability were later added.3 Type 5 SLAP lesions are Bankart lesions that extend superiorly to the biceps attachment (Fig. 18-6). Type 6 SLAP lesions have an anterior or posterior labral flap and a type 2 separation from the superior glenoid (Fig. 18-7). Type 7 SLAP lesions include a separation of the biceps attachment that extends into the middle glenohumeral ligament (Fig. 18-8). A type 8 SLAP4 is a posterior labral extension of a type 2 SLAP lesion (Fig. 18-9). Type 9 SLAP lesions show complete circumferential labral tearing (Fig. 18-10). A type 10 SLAP lesion includes a type 2 SLAP with a posterior inferior labral separation.
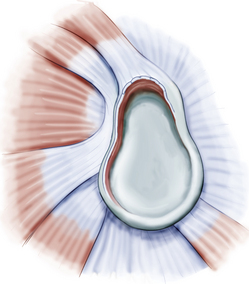
FIGURE 18-6 A type 5 SLAP is a Bankart lesion that extends to the biceps attachment.
(From Powell SE, Nord KD, Ryu RK. The diagnosis, classification and treatment of SLAP lesions. Oper Tech Sports Med. 2004;12:99-110.)
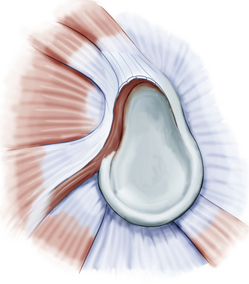
FIGURE 18-8 Type 7 SLAP lesions include a separation of the biceps attachment that extends into the middle glenohumeral ligament.
(From Powell SE, Nord KD, Ryu RK. The diagnosis, classification and treatment of SLAP lesions. Oper Tech Sports Med. 2004;12:99-110.)
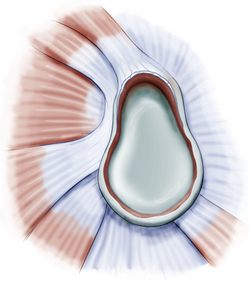
FIGURE 18-10 A type 9 SLAP lesion is a type 2 SLAP with circumferential labral tearing.
(From Powell SE, Nord KD, Ryu RK. The diagnosis, classification and treatment of SLAP lesions. Oper Tech Sports Med. 2004;12:99-110.)
Despite the extensive classification of SLAP tears, the overall incidence of superior labral pathology is low unless associated with shoulder instability. Type 2 tears are the most frequently observed clinically significant labral lesions. Excluding a type 1 tear, type 2 lesions represent 50% or more of SLAP tears, but only 4% to 6% of all intra-articular pathology detected at the time of arthroscopy.2,7 The most frequently associated pathology in patients younger than 40 years with clinically significant type 2 lesions is shoulder instability. When the patient is older than 40 years and a type 2 SLAP lesion is present, rotator cuff pathology or glenohumeral arthritis is most frequently found.9 There is no advantage to repairing a SLAP lesion in patients older than 50 years.12
CLINICAL PRESENTATION
History
The history and physical examination are very important in the identification of clinically significant SLAP lesions, which are commonly found in throwing athletes or after a specific traumatic event.2,3,7 Many patients complain about anterior shoulder pain, clicking and popping in the shoulder, and decreased function. A long history of overhead throwing activity may result in significant humeral retroversion. Athletes often will present with overhead activity pain, decreased power or velocity of their throws (sometimes termed dead arm syndrome),13,14 or slower lap time in swimmers. Each of these may manifest acutely or over time.
The primary challenge for the clinician is to distinguish symptomatic superior labral pathology from asymptomatic lesions and normal anatomic variations.8 The physical examination and mechanism of injury should correlate with a SLAP tear. The addition of imaging studies can be helpful, but should be reviewed with discernment because they can give false-positive results.15,16
Most SLAP lesions are found in the dominant arm of male patients who have been involved with overhead or throwing activities at a high level, and are younger than 40 years. The traumatic subgroup may have isolated shoulder trauma or variations of instability. The initial history should reveal patients who have a history of a shoulder dislocation, a fall on outstretched hand, or a motor vehicle accident during which the patient was wearing a shoulder lap belt over the involved shoulder.17
Patient age is an important consideration when diagnosing shoulder pain, and it is important to understand which patients are likely to develop a true SLAP injury. Patients older than 40 years often have naturally occurring degenerative changes that can mimic a SLAP lesion.9,12 Pfahler and associates5 have described the normal aging pattern of the superior labrum. Microscopic and macroscopic evaluation of normal shoulders demonstrated age-dependent variations. Three age- dependent stages were described: (1) a child up to 10 years old has a normal circumferential labral attachment without damage; (2) adults between 30 and 50 years old demonstrate fissuring and sublabral recesses at the superior and anterosuperior area of the glenoid labrum; and (3) those older than 60 years demonstrate an inconsistently attached superior labrum with tearing, fissuring, and labral detachment.5
Physical Examination
Various physical examination maneuvers have been described to aid in diagnosis of symptomatic SLAP lesions. The common element of these maneuvers is the application of either torsional or tensile loads on the biceps anchor.
A positive Speed test18 produces pain at the anterior bicipital groove by resisted forward flexion with the shoulder flexed at 90 degrees and the forearm fully supinated. A positive test suggests biceps tendinitis.
The modified O’Brien test19 is performed with the patient’s arm in 10 to15 degrees of adduction and 90 degrees of forward flexion (Fig. 18-11). With the patient’s arm fully pronated and the thumb pointing toward the floor, the patient resists the examiner’s downward pressure on the wrist of the outstretched arm. Next, the arm is fully supinated, with the palm facing up, and the examiner again places downward pressure on the wrist while the patient resists. Anterior shoulder pain with forearm pronation that is relieved with supination is considered a positive test and suggestive of a SLAP lesion. Tenderness at the acromioclavicular (AC) joint combined with local tenderness to palpation is suggestive of AC joint pathology. In both cases, a positive test consists of less pain with the palm up than with the thumb down.