Subacromial Impingement and Full Thickness Rotator Cuff Tears in Overhead Athletes
Champ L. Baker
Andrew L. Whaley
Mark Baker
HISTORICAL OVERVIEW
The incidence of shoulder injuries varies with type of sport and the level of the athletic competition. Athletes who participate in overhead sports are particularly susceptible to shoulder injuries. Because of the repetitive, forceful overhead motion in sports such as baseball, swimming, or tennis, unusual stresses occur in the rotator cuff that are not frequently found in the general population (1, 2, 3, 4). Because of these stresses, the overhead athlete can sustain cuff tears of varying thickness. Most often, these tears are of partial thickness; full thickness cuff tears are uncommon. In fact, full thickness rotator cuff tears in the general population are uncommon in the first four decades of life, which include the typical ages of the overhead athlete (5, 6, 7).
ETIOLOGY OF INJURY
Rotator cuff tears have been traditionally attributed to one of three mechanisms: primary impingement, secondary impingement due to underlying glenohumeral instability, or tensile overload (8). Neer proposed that primary, or subacromial outlet impingement, can result from the impingement of the rotator cuff against the osteophytes on the undersurface of the acromion, at the coracoacromial arch from a congenitally thickened coracoacromial ligament, or from an unstable os acromiale that hinges down and causes impingement (9). Secondary impingement occurs in individuals who have anterior capsular laxity (10). When these individuals place their arms in the overhead position with their shoulders in 90 degrees of abduction and maximal external rotation, the supraspinatus and infraspinatus tendons impinge on or make contact with the posterosuperior aspect of the glenoid and labrum (internal impingement). With repetitive throwing and with the forces generated by the act of throwing, labral injury and cuff tears can occur. The cuff tears produced by this mechanism of injury are typically partial thickness articular rotator cuff tears. Tensile overload occurs most often with a fall or with a direct blow or force to the shoulder as can occur in contact sports (11). In these situations, the forces across the tendons of the rotator cuff exceed the intrinsic strength of the tendon and it ruptures.
PRESENTATION AND PHYSICAL EXAMINATION
It is important to start the examination of the patient with a careful review of his or her history. Clues to the cause of the problem can be gained by questioning the patient as to whether the pain occurred suddenly or had an insidious onset, where the pain is located, what position the arm is in when the pain occurs, whether the arm ever feels as if it is going “dead,” and whether there is any weakness. Patients with a full thickness cuff tear may complain of weakness of the arm, either acutely or of gradual onset. They may also describe pain about the shoulder at night and with activities. A patient with primary impingement reports pain when lifting the arm overhead.
A thorough examination of the extremity for any patient with shoulder pain should include an examination of the cervical spine to rule out a neurologic problem or degenerative disease that can mimic shoulder pathology. If a rotator cuff tear or subacromial impingement is suspected, we then focus our examination and perform specific tests to reproduce the patient’s symptoms. Patients with subacromial impingement have reproducible pain with the test described by Hawkins and Kennedy (12). The patient’s arm is passively flexed to 90 degrees and forcibly internally rotated (Fig. 11-1). With the Neer test for subacromial impingement (13), the examiner stabilizes the patient’s
scapula while raising the arm in forward elevation (Fig. 11-2). Both of these tests bring the greater tuberosity, the biceps tendon, and the rotator cuff under the coracoacromial arch and reproduce the painful symptoms.
scapula while raising the arm in forward elevation (Fig. 11-2). Both of these tests bring the greater tuberosity, the biceps tendon, and the rotator cuff under the coracoacromial arch and reproduce the painful symptoms.
 FIGURE 11-1. Hawkins test for impingement. The arm is elevated to 90 degrees and forcibly internally rotated. Pain indicates impingement. |
Patients with full thickness tears of muscles of the rotator cuff exhibit weakness during testing of the particular muscle involved, may have a difference between active and passive range of motion of the shoulder, and may have atrophy of the muscles involved if it is a chronic tear. During range of motion testing, patients often initially shrug when attempting to abduct their arms if a cuff tear is present because they are using scapulothoracic motion to compensate for the inability of the cuff to abduct the arm. Weakness with abduction or with the shoulder at 90 degrees of abduction and the arm forward flexed 30 degrees with the thumb pointed to the ground would indicate weakness of the supraspinatus (14). Weakness or rupture of the external rotators of the shoulder should also be tested for during the physical examination (Fig. 11-3). Persons with large or massive cuff tears involving multiple tendons are often unable to actively externally rotate their arms. Another way of testing the integrity of the external rotators is to place the arm at the side of the patient with the elbow bent to 90 degrees and the arm passively externally rotated; once the arm is released, it drifts back into internal rotation because of the unopposed action of the subscapularis (external rotation lag sign) (15). Similarly, the inability to actively externally rotate the abducted arm has been termed the signe de clarion (“hornblower’s sign”) because it puts the arm in the position used to blow a bugle (10).
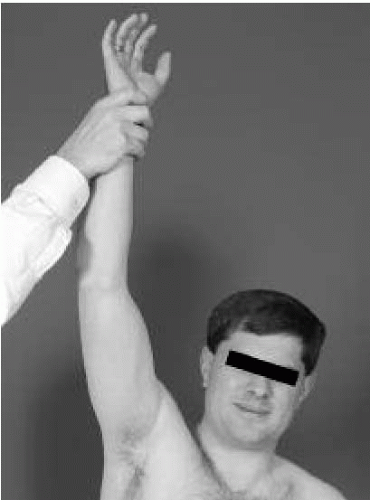 FIGURE 11-2. Neer test for impingement. The arm is raised in forward elevation. Pain near terminal elevation indicates impingement. |
Two tests specifically identify weakness of the subscapularis tendon. The first test is to have the patient attempt to push the wrist off his or her back against resistance, the so-called lift-off test (Fig. 11-4); failure to be able to do so indicates weakness of the subscapularis (16). If patients are unable to reach behind themselves for any reason, we perform a second test, the belly-press test. This test assesses the strength of internal rotation by having the patient place the
hand of the affected side on the abdomen and then pressing the hand against the abdomen with the elbows in front of the torso. If the subscapularis is not intact, the patient cannot press against the abdomen and the elbow drops behind the torso. Recent work from the Steadman-Hawkins group has demonstrated that, while both the lift-off and the belly-press are valid tests for the integrity of the subscapularis tendon, there are subtle differences (17). The lift-off test is superior for activating the lower portion of the subscapularis, and the belly-press test is superior for activating the upper portion of the subscapularis. Patients with a tear of the subscapularis not only have limited active internal rotation but also have excessive passive external rotation.
hand of the affected side on the abdomen and then pressing the hand against the abdomen with the elbows in front of the torso. If the subscapularis is not intact, the patient cannot press against the abdomen and the elbow drops behind the torso. Recent work from the Steadman-Hawkins group has demonstrated that, while both the lift-off and the belly-press are valid tests for the integrity of the subscapularis tendon, there are subtle differences (17). The lift-off test is superior for activating the lower portion of the subscapularis, and the belly-press test is superior for activating the upper portion of the subscapularis. Patients with a tear of the subscapularis not only have limited active internal rotation but also have excessive passive external rotation.
 FIGURE 11-3. Weakness with the arm at the side and the elbow to flexed 90 degrees while resisting external rotation indicates weakness or rupture of the external rotators of the shoulder. |
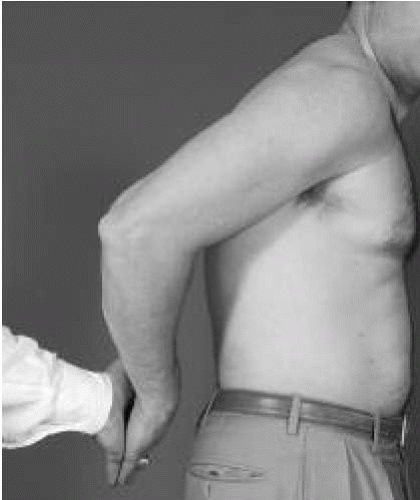 FIGURE 11-4. The lift-off test for subscapularis strength. With the hand behind the back, the patient attempts to push the hand off the back against resistance. |
If there is a question as to the integrity of the rotator cuff with subacromial impingement, we routinely inject the subacromial bursa with lidocaine, and, after several minutes, we retest the strength of the rotator musculature. If the pain is no longer present but weakness persists, the diagnosis of compromised cuff integrity can be made. If pain is no longer present when the test for impingement is repeated, the diagnosis of subacromial impingement is also made.
RADIOGRAPHIC AND DIAGNOSTIC EVALUATION
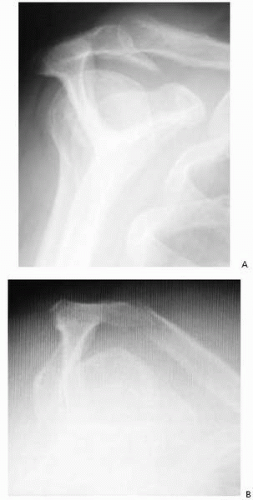
We obtain three radiographic views of the involved shoulder in patients with suspected rotator cuff injury. The first is an anteroposterior view of the glenohumeral joint in the scapular plane. This radiograph allows the clinician to examine the glenohumeral joint for evidence of fracture or degenerative disease. Also on this view, one can examine the acromioclavicular joint and assess the acromion for undersurface spur formation or degenerative changes. Additional findings that can be seen on this radiographic view are calcifications
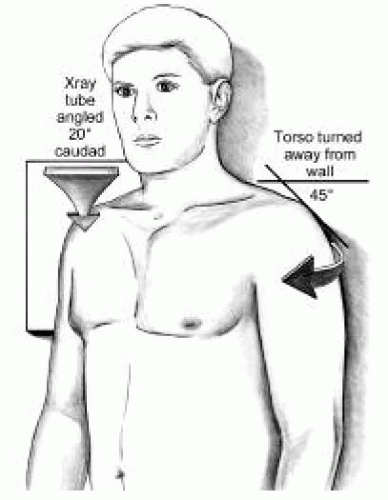
within the cuff tendons and superior migration of the humeral head. Normally, the space available for the cuff tendons between the humeral head and the acromion is estimated to be between 7 and 14 mm (18). With a space of less than 7 mm, there is an increased likelihood of a large rotator cuff tear and a poorer prognosis (19). The second view is the axillary lateral radiograph. Not only does this particular view allow one to verify that the shoulder is not dislocated, but it also is used to examine for bony avulsions off the glenoid or the humerus. This view is also used to make the diagnosis of glenohumeral arthritis. An os acromiale is visible on this view. An unstable os acromiale can hinge through the unfused segment and cause impingement symptoms. The third view can be either a supraspinatus outlet view (Fig. 11-5) or an ALVIS, (anterolateral view of impingement site) view (Figs. 11-6 and 11-7). We use either view to assess the shape of the acromion, bony impingement that might be present, and the space available for the rotator cuff. Of the three acromial shapes visible on these radiographic views—flat (type I), curved (type II), or hooked (type III)—type III acromions a greater association with abnormalities of the rotator cuff (Fig. 11-8) (20).
within the cuff tendons and superior migration of the humeral head. Normally, the space available for the cuff tendons between the humeral head and the acromion is estimated to be between 7 and 14 mm (18). With a space of less than 7 mm, there is an increased likelihood of a large rotator cuff tear and a poorer prognosis (19). The second view is the axillary lateral radiograph. Not only does this particular view allow one to verify that the shoulder is not dislocated, but it also is used to examine for bony avulsions off the glenoid or the humerus. This view is also used to make the diagnosis of glenohumeral arthritis. An os acromiale is visible on this view. An unstable os acromiale can hinge through the unfused segment and cause impingement symptoms. The third view can be either a supraspinatus outlet view (Fig. 11-5) or an ALVIS, (anterolateral view of impingement site) view (Figs. 11-6 and 11-7). We use either view to assess the shape of the acromion, bony impingement that might be present, and the space available for the rotator cuff. Of the three acromial shapes visible on these radiographic views—flat (type I), curved (type II), or hooked (type III)—type III acromions a greater association with abnormalities of the rotator cuff (Fig. 11-8) (20).
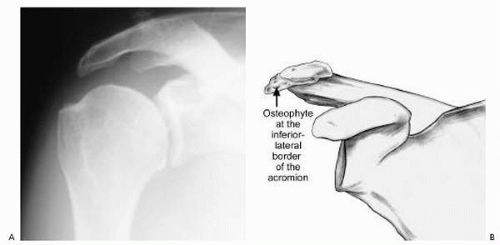 FIGURE 11-7. A: ALVIS view shows osteophytes on the lateral border of the acromion. B: Drawing shows location of osteophyte that may be source of impingement. |
We obtain additional radiographs as indicated clinically. Nakagawa and associates reported visualizing a notch on the greater tuberosity on the anteroposterior scapular view, the Stryker view, and the 45-degree craniocaudal view in throwing athletes (21). They noted that the presence of a notch was significantly related to the existence of a rotator cuff tear, whereas the size of the notch was significantly related to the depth and width of the tear.
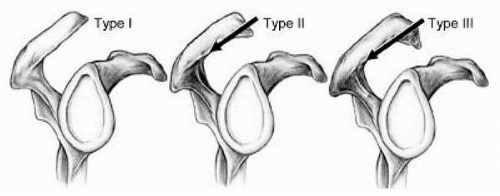 FIGURE 11-8. Three types of acromion: type I, flat; type II, curved; type III, hooked. The arrow indicates the plane of resection for a subacromial decompression. |
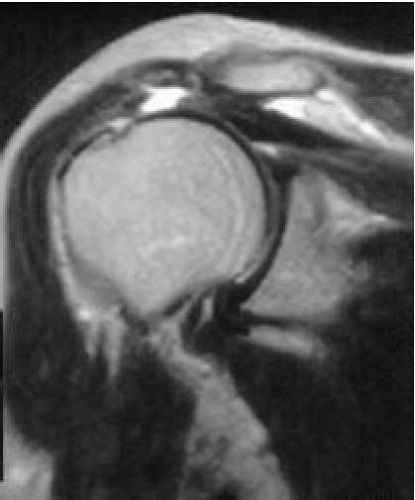
Magnetic resonance imaging (MRI) is not routinely done unless a question remains regarding the integrity of the cuff or if there is a suggestion of concurrent pathologic anatomy that might need to be addressed at the time of surgery. An MRI scan provides information as to the quality of the tissues of the cuff as well as the size and location of the tears. We order MRI scans with gadolinium contrast because it greatly improves the delineation of cuff disorders and other possible problems, such as labral and bicipital involvement (Fig. 11-9).
CLASSIFICATION OF SUBACROMIAL IMPINGEMENT
Neer classified primary or subacromial impingement into three stages of increasing severity (13) (Table 11-1). Stage I lesions are usually seen in athletes younger than 25 years of age and are characterized by edema and hemorrhage of the subacromial bursa. Stage II lesions are seen in athletes who are typically older than 25 years of age and are characterized by fibrosis and scarring of the subacromial bursa. Stage III impingement is seen in older athletes, usually 40 years or older, and involves the rotator cuff, which is torn to some extent. If impingement is left untreated, it will likely progress through the aforementioned stages, resulting in chronic degeneration and eventually full thickness tears.
TREATMENT OF SUBACROMIAL IMPINGEMENT
Nonoperative Treatment of Subacromial Impingement
In our experience, most patients with subacromial impingement syndrome recover with nonoperative intervention. Prevention and treatment of stage I impingement in athletes can prevent its progression. Icing the shoulder after
workouts and nonsteroidal antiinflammatory medications reduce the inflammatory reaction. Ultrasound and transcutaneous nerve stimulation may be helpful in the treatment of athletes with impingement. The nonoperative program should include rest or modification of activities, subacromial injection of steroids, and a physical therapy regimen.
workouts and nonsteroidal antiinflammatory medications reduce the inflammatory reaction. Ultrasound and transcutaneous nerve stimulation may be helpful in the treatment of athletes with impingement. The nonoperative program should include rest or modification of activities, subacromial injection of steroids, and a physical therapy regimen.
TABLE 11-1. NEER CLASSIFICATION OF SUBACROMIAL IMPINGEMENT | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||
The patient with impingement syndrome should be placed on a program of strengthening exercises. The following program should be adhered to until all strengthening goals are met.
Phase 1 (Protective)
Heat and ice as needed to help obtain motion
Achieve staged passive range-of-motion goals in forward elevation
Achieve staged passive range-of-motion goals in external rotation at 20 and 90 degrees of abduction
Posterior capsule stretching
Initiate functional internal rotation and active assisted range of motion as tolerated
Theraband scapular retractions
Progressive serratus anterior strengthening (isolated)
Theraband external rotation and internal rotation strengthening (pain-free, elbow by side)
Active assisted forward elevation → active forward elevation (pain-free)
Continue isometric abduction
Cautions:
Do not initiate rotator cuff strengthening until night pain has subsided and overall pain level is low.
Assure normal scapulohumeral rhythm with active forward elevation.
Phase 2 (Progressive Strengthening)
Goals
Achieve staged range-of-motion goals
Eliminate shoulder pain
Improve strength, endurance, and power
Increase functional activities
Scapular stabilization
Core strengthening
Operative Treatment of Subacromial Impingement
Treatment depends somewhat on the stage of the disease, with stage I and most of stage II impingement being amenable to nonoperative treatment. In general, most athletes with early stages of primary impingement without full thickness rotator cuff tears do well with nonoperative treatment aimed at strengthening the cuff musculature, reducing inflammation, and regaining range of motion (12,22). When patients do not respond to nonoperative treatment or have advanced stage II or stage III impingement, they are treated surgically with open anterior acromioplasty, resection of coracoacromial ligament, or by arthroscopic subacromial decompression.
Initial reports on the surgical treatment of impingement in athletes were not particularly encouraging. Tibone and co-workers reported their results of open acromioplasty in young athletes (28 overhead athletes) with chronic impingement (23). Overall, 26 of the 34 shoulders (76%) continued to have problems with throwing or overhead activities after surgery, and only 22% of pitchers and throwers had a good result. Fly and associates also reported their results with arthroscopic subacromial decompression in young athletes with chronic impingement (24). Despite excellent relief of pain, only 77% could return to their previous levels of activity. These reports may be misleading. Arroyo and associates asserted that some of the patients in these studies might have had internal impingement leading to failures of surgical treatment (25).
Bigliani and others reported the results of 26 patients (10 recreational athletes, no high-performance athletes) who were younger than 40 years with primary impingement (26). They concluded that open acromioplasty would give good results (81% excellent or good) in patients who had not responded to nonoperative treatment. Although this and other published studies have reported higher satisfaction rates with open or arthroscopic decompressions, usually in the range of 80%, most show only modest improvement in the results of overhead athletes. Roye and associates reported their results of subacromial decompression in 90 shoulders (including 34 throwing athletes and 12 pitchers) with stage II or early stage III impingement at 2 to 7 years of follow-up (27). They found that arthroscopic decompression was comparable to open acromioplasty, regardless of the presence of a cuff tear (93% satisfaction). They did note, however, that throwing athletes might not return to their preinjury levels of functional activity (68% satisfactory results), that reinjury is common, and that pitchers had the worst prognosis (50% satisfactory results). The authors recommended that any instability of the shoulder be treated concomitantly. Despite the better overall patient satisfaction rate in these studies, it seems that it is difficult for the overhead athlete to return to his or her previous level of competition after subacromial decompression.
In cases of primary impingement in which nonoperative treatment has failed to relieve symptoms, it is important to identify the cause of the impingement (the shape of the acromion or presence of osteophytes, a thickened coracoacromial ligament, or os acromiale) and verify that there is no concomitant internal impingement. One should also be cognizant that acromioclavicular arthritis can mimic impingement and should be dealt with accordingly. Neer is credited with identifying the need to resect the offending bony portion of the acromion impinging upon the cuff (9).
Several authors have noted that selective sectioning of the coracoacromial ligament gave good results in the treatment of impingement in the overhead athlete (12,13,22,28). Jackson reported his results in 10 athletes with chronic impingement who underwent an open resection of the coracoacromial ligament (29). Five of the patients had excellent results with no pain and full function, and six of the patients were able to return to their previous levels of competition. Another cause of impingement is an unstable os acromiale, which can hinge through the unfused portion with contraction of the deltoid and impinge on the rotator cuff. Satterlee demonstrated that surgical fusion of an impinging os acromion with internal fixation could alleviate symptoms of impingement (30).
Several authors have noted that selective sectioning of the coracoacromial ligament gave good results in the treatment of impingement in the overhead athlete (12,13,22,28). Jackson reported his results in 10 athletes with chronic impingement who underwent an open resection of the coracoacromial ligament (29). Five of the patients had excellent results with no pain and full function, and six of the patients were able to return to their previous levels of competition. Another cause of impingement is an unstable os acromiale, which can hinge through the unfused portion with contraction of the deltoid and impinge on the rotator cuff. Satterlee demonstrated that surgical fusion of an impinging os acromion with internal fixation could alleviate symptoms of impingement (30).
Primary impingement and cuff tears can be interrelated. Although there was no mention of athletes in their study group, Esch and co-workers reviewed their results of arthroscopic subacromial decompression in 71 patients (age range, 17 to 89 years) with stage II or III impingement (31). Using the UCLA rating system, they found satisfactory subjective results in 82% and satisfactory objective results in 78% of their patients with stage II impingement. Of those with stage II impingement without a cuff tear, the objective score was 82%. Patients with stage II impingement and a partial cuff tear had an objective score of 78%. Of those with stage III impingement, they noted that 88% had subjective satisfactory results and 77% had objective satisfactory ratings. The presence of a cuff tear, regardless of thickness, only slightly decreases the subjective and objective results in the general population.
CLASSIFICATION SYSTEM FOR ROTATOR CUFF TEARS
A variety of classification systems for rotator cuff disease exist. Some are applicable for both partial and full thickness cuff tears. Patte described a classification scheme based on the extent of the tear, the topography of the tear in the sagittal and frontal planes, the quality of the tendons, and the status of the biceps tendon (32). Snyder’s classification is based on the location of the tear, the tendon involved, and the grade of the tear (Table 11-2) (33). Other ways to describe the type of tear include using descriptive terms: partial or full thickness tear, location and orientation of the tear, and shape of the tear.
Several classification methods based on the size of the tear or number of tendons involved have been described specifically for complete tears. Ellman and co-workers classified full thickness tears as small if they were less than 2 cm, as large if they were between 2 and 4 cm, or as massive if they were greater than 4 cm (19). Post and associates classified small tears as those less than 1 cm, moderate as those between 1 and 3 cm, large as those between 3 and 5 cm, and massive as those greater than 5 cm (34). Others have classified tears that are confined to only the supraspinatus tendon as small, tears involving two tendons as moderate, and tears involving three or four tendons as large or massive (35). Cofield defined a massive tear as a tear that is larger than 5 cm in maximum diameter (36). Others define massive as disinsertion of at least two complete tendons (36).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree