Imaging of the Overhead Athlete
Eric D. Smith
Charles P. Ho
INTRODUCTION
The shoulder has the most complex and greatest range of motion of any joint in the body. This range and versatility is possible because of the articulation of the relatively large humeral head and smaller and shallow glenoid fossa. The inherently unequal osseous articulation must rely on the glenoid labrum to deepen and enlarge the glenoid socket and on the capsular-labral complex, glenohumeral ligaments, and rotator cuff to provide additional stability as well as power for shoulder function. This complex anatomy and function are vital to the overhead athlete as well as overhead use in occupational endeavors and activities of daily living. Overhead function produces extensive demands on the soft tissues and osseous structures of the shoulder, often leading to pain and dysfunction. The clinical evaluation of these symptoms is complex and at times inconclusive. Imaging evaluation, both with conventional radiographs and magnetic resonance imaging (MRI), has proven an invaluable aid for both diagnosis and reassessment after treatment.
The approach to imaging of the overhead athlete applies to swimmers, gymnasts, climbers, throwing athletes, paddlers, players of racquet sports, and athletes who engage in weight training either as the primary sport or as supplemental training. Repetitive overhead activity in the workplace as performed by painters, carpenters, or laborers subjects the shoulder to similar stresses and leads to similar patterns of injury as in the sports participants. This large cohort of patients is subject to the same injuries as occur in nonoverhead athletes as well as more activity-specific injuries.
RADIOGRAPHIC EVALUATION
The goals of any radiographic examination are to provide the treating physician with the necessary supporting diagnostic information to facilitate treatment with as little expense, complexity, time delay, and patient discomfort as possible. It is equally important for both the imaging specialist and treating specialist to be confident in the validity and reproducibility of the techniques used. Patients must be able to tolerate the length and positioning of the examination.
Conventional radiographs are the starting point for the imaging evaluation of nearly all musculoskeletal complaints. In the evaluation of the shoulder, they are rarely the final imaging step. They do demonstrate osseous anatomy, but their projectional rather than tomographic nature limits the evaluation of three-dimensional relationships. They provide the most limited evaluation of soft tissue. Most pathologic processes affecting the overhead athlete only demonstrate radiographic changes at the late stages, long after the optimal period for intervention.
Radiographs are most helpful in initial screening for fractures or advanced osseous degenerative change. They are also helpful in the demonstration of dystrophic or heterotopic calcification and in the evaluation and characterization of primary osseous or chondral neoplasms.
Computed tomography (CT) has optimal spatial resolution and is the most sensitive technique for showing cortical bone, complex fracture anatomy, and small amounts of calcification or ossification. Without the introduction of intraarticular contrast (gas or iodinated contrast), CT is well suited to detection of intraarticular osseous or calcific bodies, whereas intraarticular contrast may assist in evaluation of soft tissue internal bodies or debris. However, the limited soft tissue characterization of CT makes it primarily a specialty, problem-solving tool in shoulder evaluation.
In recent years, high-resolution ultrasound of the musculoskeletal system has gained in popularity and use. One of the first areas of clinical utility was in the evaluation of the rotator cuff. In experienced hands, ultrasound is highly accurate in the diagnosis of rotator cuff tears. It has high patient satisfaction, low cost, and comparatively fewer equipment requirements. However, it is less well suited for evaluating osseous anatomy, articular cartilage, and labral abnormalities that affect overhead athletes. It also has a much higher level of operator dependence. The images obtained are often more difficult for clinical colleagues to appreciate because they bear less resemblance to surgical anatomy.
MRI has become the most widely accepted technique for evaluation of the shoulder. No other technique combines its soft tissue resolution and multiplanar capability. It is the imaging gold standard for evaluation of internal derangements and shows the highest correlation with surgical results.
GENERAL SHOULDER MRI
MRI of the shoulder poses greater technical difficulty and is more often the focus of debate and controversy than imaging of other areas of the musculoskeletal system. The highly complex and variable nature of the labral and capsular structures also makes interpretation complex. There is a growing diversity of both hardware and software alternatives that make generalization about technique and establishment of standard imaging protocols difficult.
The demand for lower cost MRI combined with technical advances has led to the development of a great diversity of magnets. These include whole-body magnets as well as extremity-only scanners. Whole-body scanners are available in two basic configurations: open and closed. Closed magnets are more common and have been the predominant design for high field strength imaging. Open systems are designed to reduce the risk of claustrophobia. They are often permanent magnets that operate at room temperature and generally cost less than closed, superconducting magnets. However, the trade-off for lower field strength in the open systems is longer imaging time to achieve equal signal-to-noise and spatial resolution (1). The longer imaging time may in turn contribute to patient discomfort and motion with resulting image degradation. Lower field strength systems also restrict the ability to perform spectral fat suppression.
Coil selection is an important part of MR image quality. As with scanners, multiple different designs are available. Phased-array coils offer the highest signal-to-noise ratio. Flex coils are versatile and well suited to a range of shoulder configurations and positions. In most all situations, a single surface coil is used.
SPECIFIC SHOULDER MRI CONSIDERATIONS
The bore size of closed whole body MR systems only allows for the shoulder to be imaged with the arm at the patient’s side or overhead. Open systems allow for more flexibility in patient positioning. The shoulder is most commonly imaged with the patient supine and the arm at the patient’s side. Positioning of the hand determines the degree of external rotation. The extent of rotation is controversial. External rotation with the thumb away from the patient can be uncomfortable, tightens the anterior capsule, and can cause gas to form in the joint via vacuum phenomenon. Internal rotation with the thumb directed toward the patient causes the infraspinatus tendon to overlap the supraspinatus tendon and causes the subscapularis tendon to be redundant, folding on itself. Neutral positioning with the thumb directed up is usually best tolerated by the patient and minimizes motion artifacts.
Routine shoulder MRI is usually performed in three planes. A plane axial to the glenohumeral joint serves as a localizer for obtaining the oblique sagittal and coronal planes. The oblique coronal plane follows the orientation of the supraspinatus and infraspinatus muscle bellies. It is usually obtained by aligning with the scapular spine and orthogonal to the glenoid fossa plane on a mid glenoid slice of the axial localizer. The oblique sagittal plane is also obtained from an axial localizer, but is parallel to the articular surface of the glenoid and perpendicular to the scapular spine. Even though an attempt is made to evaluate all structures in all planes, certain anatomic features are best demonstrated in one projection. The axial plane is best suited for evaluation of the acromion base, anterior and posterior labrum, glenohumeral articular surface, intertubercular biceps tendon, and subscapularis tendon. The oblique coronal plane optimizes evaluation of the superior and inferior labrum, labral-biceps anchor, acromioclavicular (AC) joint, and supraspinatus and infraspinatus muscles. The oblique sagittal plane is best for evaluation of the coracoacromial arch, intraarticular long biceps tendon, and rotator interval.
The overhead position (also referred to as ABER for abduction and external rotation) is achieved in a supine patient by positioning the patient’s hand over or behind his head (2). Oblique axial images are obtained by aligning sections with the long axis of the humerus and orthogonal to the glenoid fossa plane using a coronal localizer. The plane is particularly helpful for demonstrating the undersurface of supraspinatus and infraspinatus tendons. It also shows the inferior glenohumeral ligament as well as the anterioinferior labrum under tension. It is also helpful to appreciate the cuff undersurface to posterior-superior glenoid and labral relationships in the overhead position that may contribute to clinical posterior-superior (internal) impingement. However, the position is often poorly tolerated by the patient with a painful shoulder and adds additional time to the imaging examination.
Sequence options for shoulder imaging include spinecho, fast spin-echo, gradient echo, and short tau inversion recovery (STIR). Each of these techniques has strengths and weaknesses.
Conventional T1-, proton density (PD)-, and T2-weighted spin-echo sequences have been the primary imaging sequences for the shoulder. T1-weighted spin-echo is relatively rapid, can be used on both high and low field strength systems, and offers high fat water contrast. However, T1-weighted images suffer from relatively poor soft tissue contrast. T1-weighted spin-echo is also used to show areas of enhancement after intravenous or intraarticular administration of gadolinium (Gd)-based contrast. Frequency selective fat suppression is often used to provide contrast between fat and Gd-enhanced tissues. Fat suppression also enhances contrast between articular cartilage and joint fluid. T2-weighted
spin-echo generates contrast on the basis of differences in free and bound water. It is more sensitive for inflammation, infection, and trauma. T2-weighted images are relatively unaffected by magic angle phenomenon. The disadvantages are long imaging time and limited signal-to-noise ratio.
spin-echo generates contrast on the basis of differences in free and bound water. It is more sensitive for inflammation, infection, and trauma. T2-weighted images are relatively unaffected by magic angle phenomenon. The disadvantages are long imaging time and limited signal-to-noise ratio.
The development of fast spin-echo allowed development of T2-weighted images in a fraction of the time of conventional spin-echo with greater spatial resolution. Fast spinecho is the least vulnerable to magnetic susceptibility effects amongst available pulse sequences. Fat also remains high in signal intensity on fast spin-echo T2-weighted images. This lowers the contrast between fat and fluid. Use of frequency selective fat suppression can be added, but magnetic field heterogeneity can produce uneven fat suppression.
STIR imaging provides fat suppression that is less susceptible to magnetic field inhomogeneities. The technique is extremely sensitive to free water. It can be obtained on both low and high field scanners. However, signal-to-noise ratio is relatively low and excessive signal loss in soft tissues can reduce overall diagnostic utility of the images.
Gradient echo images are another alternative to conventional T2-weighted spin-echo images. They are considerably faster, thus permitting thinner image sections. They also accentuate edges, which may be helpful in labral evaluation. However, they are vulnerable to magic angle effects, have a low sensitivity for evaluation of articular cartilage, and have high sensitivity to magnetic susceptibility effects.
MR ARTHROGRAPHY AND CONTRAST IMAGING
In addition to standard MRI of the shoulder, MR arthrography can be performed either by direct or indirect approach. Direct arthrography uses intraarticular injection of contrast material whereas indirect arthrography uses intravenous injection of Gd-based contrast agents. Direct MR arthrography has been the most widely used technique and is analogous to other forms of arthrography. Typically 15 to 20 mL of a Gd-saline solution (diluted to about 1/200) is injected into the joint under fluoroscopic visualization. Saline only may also be used for MR arthrography. T1-weighted images are then obtained in two to three planes, typically with frequency selective fat saturation. After injection, PD- or T2-weighted images with fat suppression are acquired in two to three planes. This technique distends the joint to provide better definition of labrocapsular structures and may improve sensitivity of some rotator cuff tears. The disadvantages of direct arthrography include the need for fluoroscopic guidance, which adds to procedure time and may be unavailable at some outpatient imaging centers. Direct arthrography converts a noninvasive standard MRI examination to a somewhat invasive procedure. The beneficial effects of direct arthrography are also limited to the space or compartment injected. There is also potential discomfort and apprehension on behalf of the patient. Some patients may experience a symptomatic synovitis after the intraarticular injection, particularly when an initial test injection of iodinated radiographic contrast is done to confirm intraarticular position before infusing the saline or Gd-saline solution.
An alternative to direct arthrography is indirect arthrography in which a standard dose of Gd contrast is injected intravenously and allowed to diffuse into the joint fluid through the synovial lining. The diffusion process typically takes 20 to 30 minutes. Active mobilization speeds the diffusion process. Indirect arthrography is less invasive and less time consuming, and may have greater patient acceptance. However, indirect arthrography does not produce joint distention to separate adjacent labral structures.
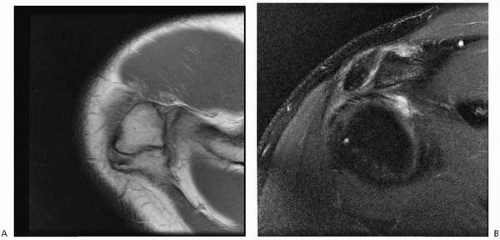
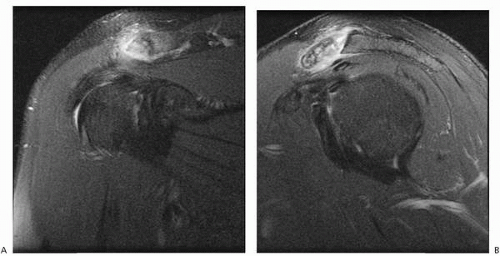
Yet another alternative may be direct contrast enhancement imaging immediately after intravenous injection of standard dose Gd contrast. The patient is imaged immediately after the Gd contrast is given intravenously, rather than after a period of waiting or exercise. This technique anticipates and uses direct enhancement of well-vascularized or hyperemic tissues by intravenous Gd contrast, and actively highlights areas of inflammation, granulation tissue, and developing scarring. Examples include the synovial tissue overgrowth associated with labral and capsular tears as well as disruptions of the bursal and articular margins of the rotator cuff (Fig. 4-1). The immediate, direct enhancement imaging is “active” contrast enhancement pointing to the area of derangement, as opposed to the “passive” contrast enhancement distending the joint indiscriminately in arthrography,
either direct or indirect. The active enhancement is not confined to the joint space or compartment injected, but encompasses the entire imaged field of view. The longer the delay between intravenous contrast administration and image acquisition, the more the direct enhancement diffuses away from the area of maximal inflammation. After the standard delay of 20 to 30 minutes, the direct technique has transformed into the passive contrast of indirect arthrography.
either direct or indirect. The active enhancement is not confined to the joint space or compartment injected, but encompasses the entire imaged field of view. The longer the delay between intravenous contrast administration and image acquisition, the more the direct enhancement diffuses away from the area of maximal inflammation. After the standard delay of 20 to 30 minutes, the direct technique has transformed into the passive contrast of indirect arthrography.
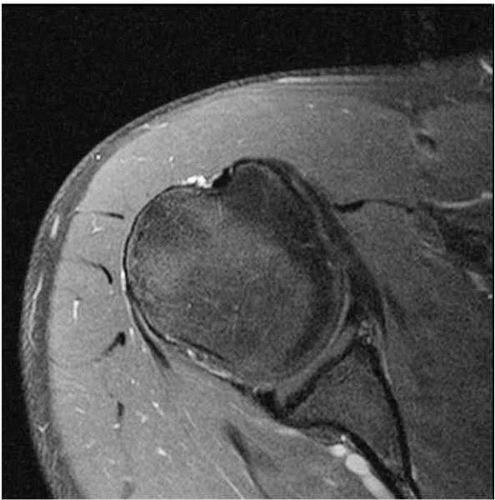 FIGURE 4-1. Anterior labral tear after intravenous gadolinium. Axial fat-suppressed T2-weighted image after intravenous gadolinium administration highlights anterior labral tearing. |
In most patients, none of the above invasive or minimally invasive contrast-enhanced procedures are necessary. The noncontrast shoulder MRI examination is generally comprehensive and diagnostic. The additional procedures are best used as specialty problem-solving tools to increase conspicuity in the patient whose case is a diagnostic dilemma. As always, cost, risk, benefit, and patient satisfaction must be considered.
Given the variety of hardware and software alternatives available, there are many possibilities for efficient and thorough shoulder imaging. The senior author uses the following protocol on high field scanners: PD-weighted and frequency selective fat-suppressed PD-weighted oblique sagittal images, PD-weighted and second echo T2-weighted oblique coronal images, and PD-weighted and gradient echo axial images.
OSSEOUS ACROMIAL OUTLET
MRI provides the optimal imaging evaluation of the osseous acromial outlet as well as soft tissues of the coracoacromial arch that may be associated with rotator cuff impingement (3). Osseous changes that can lead to extrinsic impingement and are well evaluated by MRI include anteriorly hooked acromion, lateral downsloping acromion, low-lying acromion, subacromial enthesophytes, and an os acromiale. Capsular and osseous hypertrophy of the AC joint as well as an enlarged coracoid process may also contribute to rotator cuff impingement.
The shape of the acromion and subacromial enthesophyte formation are best determined on oblique sagittal images located lateral to the AC joint. Any lateral downsloping or subacromial enthesophyte formation is best seen on oblique coronal images. Osteophytes or callus under the AC joint can predispose to impingement. However, AC arthrosis is not specific for impingement and is common in asymptomatic individuals. An inferolaterally sloping acromion has been associated with lateral supraspinatus injury near the greater tuberosity in overhead athletes who perform forceful abduction.
The os acromiale is an accessory ossification center along the outer edge of the acromion that has failed to fuse by age 25 years. Its prevalence ranges from 1% to 15% (4). It is uncertain what percentage of these are symptomatic. The synchondrosis may be fibrous or cartilaginous. The variant is bilateral 60% of the time. An association between os acromiale and impingement and rotator cuff pathology has been found, but identifying the os does not implicate it as the source of shoulder pain. The os is best seen on the axial and sagittal planes (Fig. 4-2).
A thickened coracoacromial ligament has been associated with impingement. However, objective criteria for thickening have been elusive. Others suggest that the thickening is a secondary result of impingement. The ligament and coracoacromial arch are best seen on oblique sagittal images.
The AC joint itself may be symptomatic and is well evaluated on coronal and axial images. Arthrosis manifests as prominent osteophyte formation with capsular and synovial hypertrophy and scarring. Cystic change of the acromion and distal clavicle about the joint may be seen, with reactive bone edema. Synovitis may manifest as joint effusion and debris, as well as surrounding bone edema (Fig. 4-3).
Stress-related or posttraumatic synovitis with bone edema and hyperemia may suggest developing resorption and osteolysis in overhead athletes (Fig. 4-4).
ROTATOR CUFF
Impingement Syndromes
Clinical extrinsic impingement is a syndrome that results from compression of the supraspinatus tendon, as well as the biceps tendon and subacromial bursa, between the humeral head and subacromial arch. It is common in overhead athletes and in those whose occupations require overhead motion. There are multiple types of impingement. Primary extrinsic impingement is caused by entrapment of the supraspinatus tendon by the coracoacromial arch. This is exacerbated by subacromial enthesophyte, downsloping acromion, anteriorly hooked acromion, AC joint osteophytes, os acromiale, or thickened coracoacromial ligament. The final common pathway is mechanical narrowing, friction, and impaction on the bursal surface of the supraspinatus with increased wear, degeneration, and tearing.
Secondary extrinsic impingement can be caused by narrowing of the coracoacromial outlet from glenohumeral or scapulothoracic instability. It is most common in young patients and those who perform repetitive overhead movements. It is commonly associated with anterior or multidirectional instability (5). Chronic instability is associated with capsular laxity and weakening, which forces the rotator cuff to play a greater role in stabilization. This leads to wear on the tendons with excessive humeral head translation, which results in undersurface degeneration and tearing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree