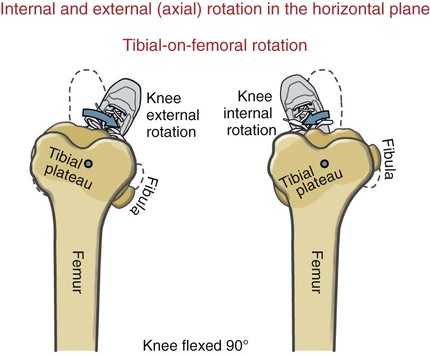
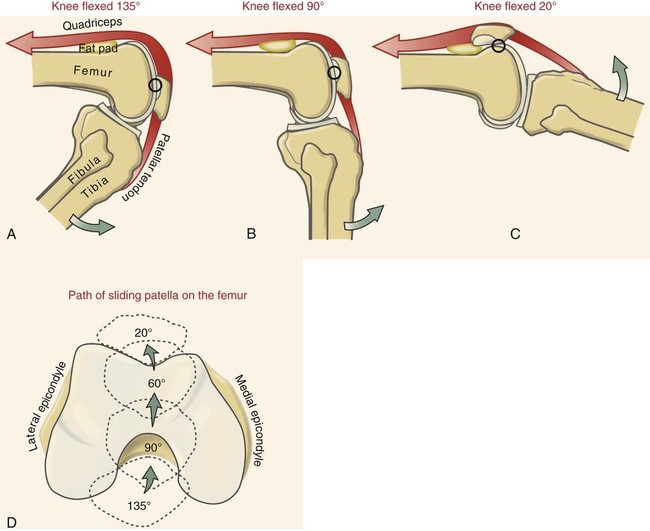
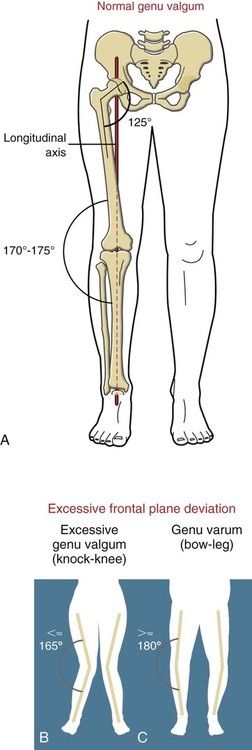
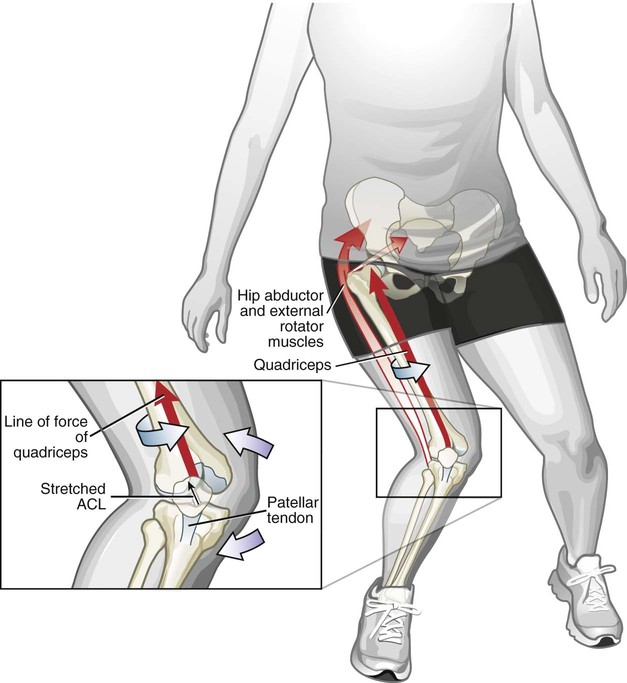
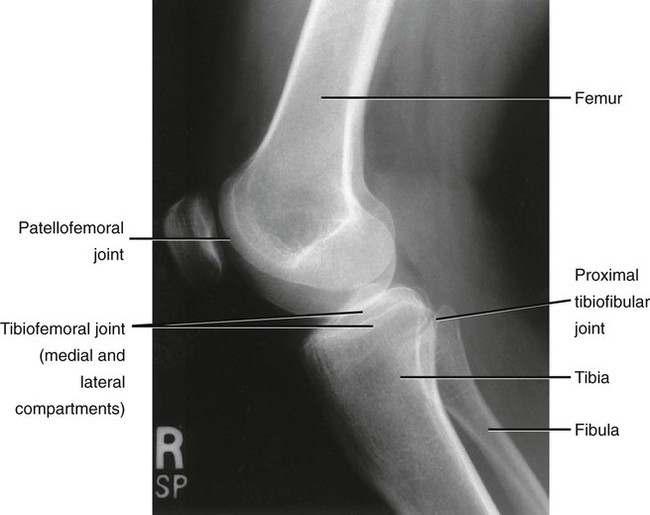
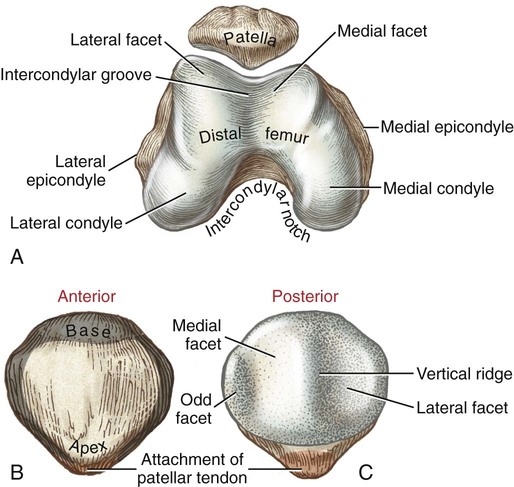
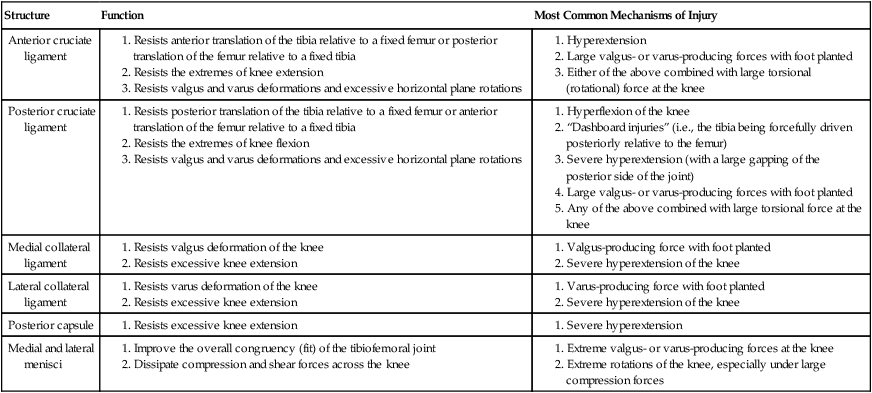
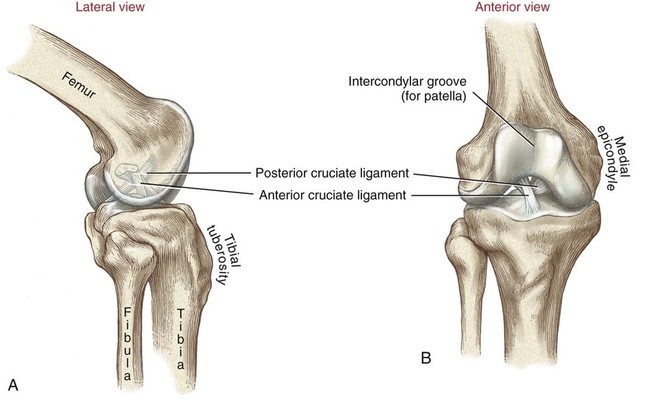
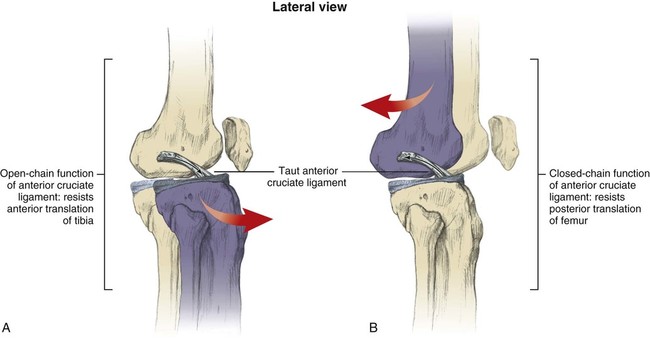
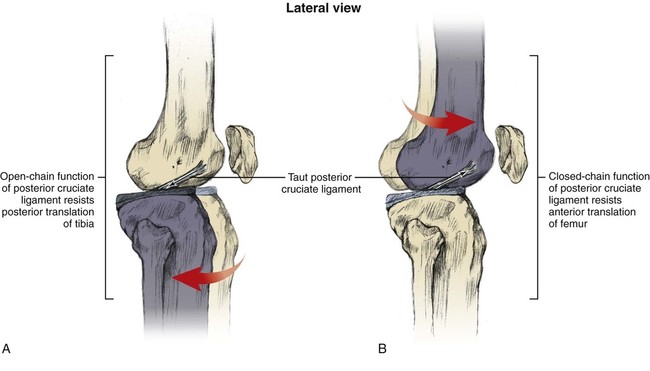
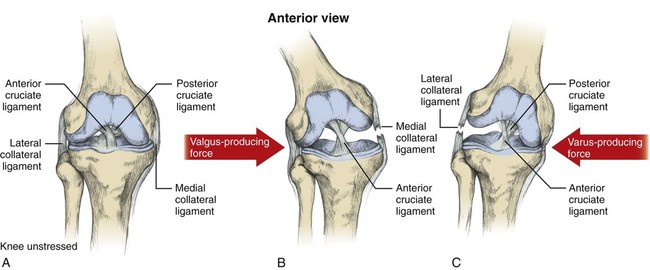
Chapter 10 • Identify the bones and primary bony features of the knee. • Describe the primary supporting structures of the knee. • Describe the planes of motion and axes of rotation for the motions of the knee. • Cite the proximal and distal attachments of the muscles of the knee. • List the innervation of the muscles of the knee. • Justify the primary actions of the muscles of the knee. • Describe the factors that contribute to excessive lateral tracking of the patella. • Explain how patellofemoral joint compression force is increased or decreased relative to the depth of a squatting position. • Describe one biomechanical consequence associated with hamstring tightness. • Explain the principles of active and passive insufficiency with regard to the multi-articular muscles of the knee. • Describe the combined movements at the hip and knee that promote the most effective force production in the hamstrings and rectus femoris. The knee consists of the tibiofemoral joint and the patellofemoral joint. As illustrated in Figure 10-1, the tibiofemoral joint is formed between the large condyles of the distal femur and the relatively flat proximal tibia. The patellofemoral joint is formed between the patella and the distal femur. Both joints are considered anatomic components of the knee. The medial and lateral condyles (from the Greek kondylos, meaning “knuckle”) are the large rounded projections of the distal femur that articulate with the medial and lateral condyles of the tibia. The intercondylar groove is the smooth rounded area between the femoral condyles that articulates with the posterior surface of the patella (Figure 10-2). The intercondylar notch is located on the posterior-inferior aspect of the distal femur, separating the medial and lateral condyles. This notch forms a passageway for the anterior and posterior cruciate ligaments. The medial and lateral epicondyles (Figure 10-3) are palpable bony projections on the medial and lateral femoral condyles, respectively; these projections serve as attachments for the medial and lateral collateral ligaments of the knee. The medial and lateral condyles of the tibia are smooth and shallow for articulation with the condyles of the femur (Figure 10-4). The flattened superior surfaces of the condyles are often called the tibial plateau. The intercondylar eminence is a double-pointed projection of bone separating the medial and lateral condyles of the tibia. This structure serves as an attachment for the anterior and posterior cruciate ligaments, as well as for the medial and lateral meniscus. The tibial tuberosity is a protrusion of bone located on the anterior aspect of the proximal tibia, which serves as the distal attachment for the quadriceps muscle. The fibula (see Figure 10-4) is a long, slender bone that courses along the lateral shaft of the tibia. The fibular head is the rounded superior portion of the fibula that articulates with the superior-lateral aspect of the tibia. This articulation forms the firm proximal tibiofibular joint. The head of the fibula is the distal attachment of the lateral collateral ligament and the biceps femoris muscle. The patella, or knee cap, is a small, plate-like bone embedded within the quadriceps tendon. Because the patella exists within the quadriceps tendon, it is highly mobile and is at risk for abnormal gliding or subluxation. A portion of the stability provided to the patellofemoral joint comes from the fit of the posterior patella within the intercondylar groove of the femur (Figure 10-5, A). The base, or superior pole, of the patella accepts the quadriceps tendon; the apex, or inferior pole, accepts the proximal side of the patellar tendon (Figure 10-5, B). The posterior articular surface of the patella articulates with the intercondylar groove of the femur through medial and lateral facets. The lateral facet is steeper than the medial facet, matching the general shape of the intercondylar groove of the femur (Figure 10-5, C). As illustrated in Figure 10-7, A (and studied in Chapter 9), the 125-degree angle of inclination of the proximal femur directs the shaft of this bone toward the midline, for eventual articulation with the tibia at the knee. Because the tibia is oriented essentially vertically while standing, the articulation between the femur and the tibia does not typically form a straight line. As shown in Figure 10-7, A, the femur usually meets the tibia to form a lateral angle of 170 to 175 degrees (the femur projects 15 to 20 degrees laterally—relative to the tibia). This alignment is referred to as normal genu valgum. Variations of this angle are not uncommon because the knee must adjust to malalignment at either the hip or the ankle. A lateral angle of less than 170 degrees is considered excessive genu valgum, or knock-kneed (Figure 10-7, B). A lateral angle greater than 180 degrees is called genu varum, giving a bow-legged appearance (Figure 10-7, C). The knee joint must remain stable even while subjected to large internal and external forces. In addition to muscle, stability of the knee is provided by the anterior and posterior cruciate ligaments, medial and lateral collateral ligaments, posterior capsule, and the menisci. The following sections will describe the structure and basic function of these important connective tissues. Table 10-1 summarizes the primary functions of these structures and lists common mechanisms of their injury. Functions and Mechanisms of Injury of the Supporting Structures of the Knee 2. “Dashboard injuries” (i.e., the tibia being forcefully driven posteriorly relative to the femur) 3. Severe hyperextension (with a large gapping of the posterior side of the joint) 4. Large valgus- or varus-producing forces with foot planted 5. Any of the above combined with large torsional force at the knee Cruciate, literally meaning “cross,” describes the X shape of the anterior and posterior cruciate ligaments as they interconnect the tibia with the femur (Figure 10-8). The predominant anterior-posterior direction of the cruciate ligaments stabilizes the knee against the large anterior-posterior shear forces that occur while walking and running. The anterior and posterior cruciate ligaments, therefore, are the most important stabilizers of the knee in the sagittal plane. Table 10-1 summarizes the primary functions of the ACL and PCL, which are illustrated in Figures 10-9 and 10-10, respectively. The medial and lateral collateral ligaments strengthen the medial and lateral sides of the capsule of the knee (Figure 10-11, A). These ligaments are the primary frontal plane stabilizers of the knee, protecting against forces that produce excessive genu valgus. The wide, flat medial collateral ligament (MCL) spans the medial side of the knee between the medial epicondyle of the femur and the proximal medial tibia. The primary function of the MCL is to resist valgus-producing forces (Figure 10-11, B). Some fibers of the MCL attach to the medial meniscus of the knee; therefore, injury to the MCL may involve injury to the medial meniscus as well. The lateral collateral ligament (LCL) is a round, cord-like ligament that crosses the lateral side of the knee, attaching to the lateral epicondyle of the femur and the head of the fibula. The primary function of the LCL is to protect the knee from varus-producing forces (Figure 10-11, C). Although the knee is stressed only minimally in the frontal plane while walking or running, rapid changes in direction or a large impact of external forces frequently injures the collateral ligaments, especially the MCL. Consider, for example, a football player who is tackled from the side (Figure 10-12). With the foot in firm contact with the ground, the medially directed force on the lateral side of the knee creates a forceful genu valgus, often tearing the MCL. The medial and lateral menisci are crescent-shaped fibrocartilaginous discs located at the top of the medial and lateral condyles of the tibia (Figure 10-13). These structures play an important role in absorbing compressive forces across the knee caused by muscular contraction and body weight. While walking, compressive forces at the knee routinely reach two to three times body weight. By nearly tripling the area of joint contact and expanding outward on weight bearing, the menisci significantly reduce the pressure across the knee. Also, the cup-shaped menisci “deepen” the articular surface of the knee, facilitating the arthrokinematics and further stabilizing the joint. The primary role of the posterior capsule is to prevent hyperextension of the knee. Two major ligaments or thickenings of the posterior capsule exist: The arcuate popliteal ligament and the oblique popliteal ligament (Figure 10-15). Flexion and extension occur in the sagittal plane about a medial-lateral axis of rotation. Motion occurs from about 5 degrees of knee hyperextension to about 130 to 140 degrees of flexion. As illustrated in Figure 10-16, the range of motion at the knee is the same whether viewed from an open-chain (tibial-on-femoral) or closed-chain (femoral-on-tibial) perspective. The only differences involve which bone is fixed and which is moving. Internal and external rotation of the knee occurs within the horizontal plane about a vertical or longitudinal axis of rotation. This motion, also called axial rotation, refers to the rotation between the tibia and the femur (Figure 10-17). With the knee flexed, the knee joint permits 40 to 50 degrees of total rotation (Table 10-2); however, with the knee fully extended, essentially no rotation occurs between the two bones.
Structure and Function of the Knee
Osteology
Distal Femur
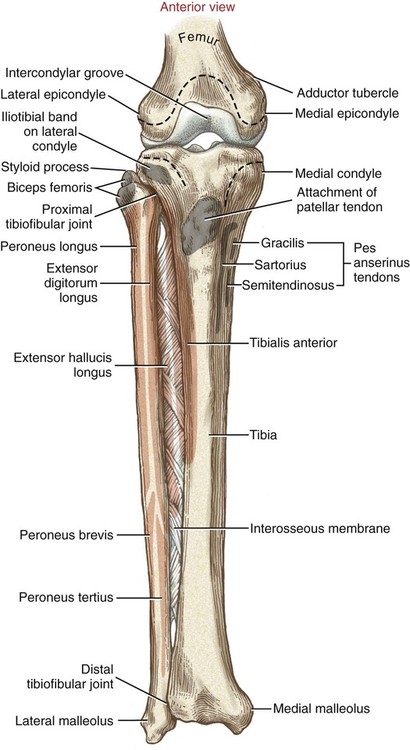
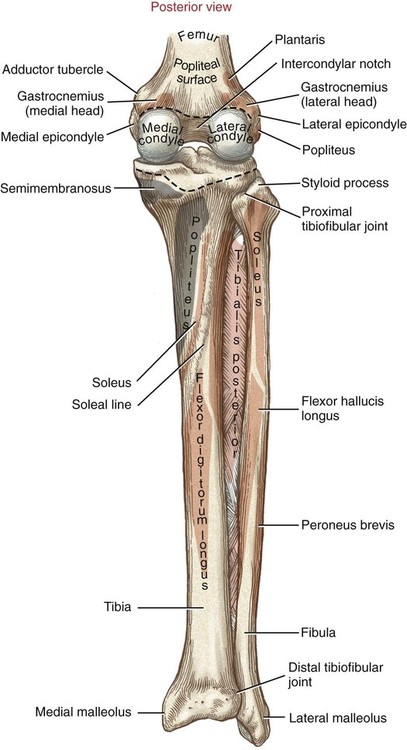
Proximal Tibia
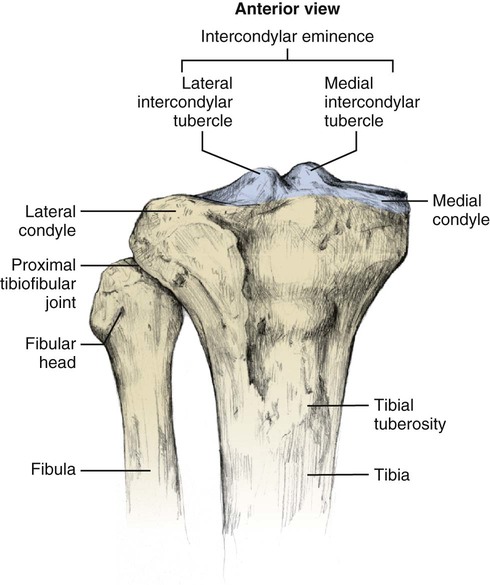
Proximal Fibula
Patella
Arthrology
General Features
Normal Alignment
Supporting Structures
![]() Table 10-1
Table 10-1
Structure
Function
Most Common Mechanisms of Injury
Anterior cruciate ligament
Posterior cruciate ligament
Medial collateral ligament
Lateral collateral ligament
Posterior capsule
Medial and lateral menisci
Anterior and Posterior Cruciate Ligaments
Medial and Lateral Collateral Ligaments
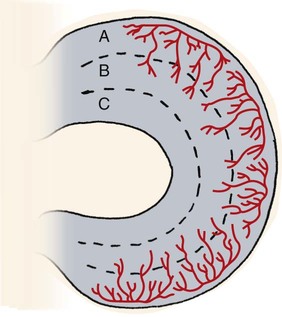
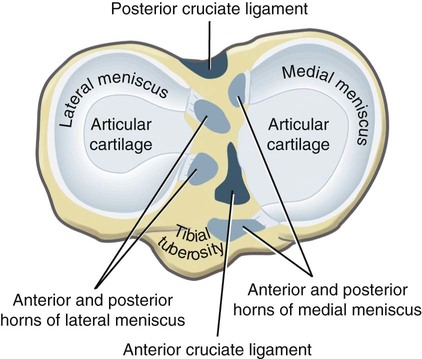
Medial and Lateral Menisci
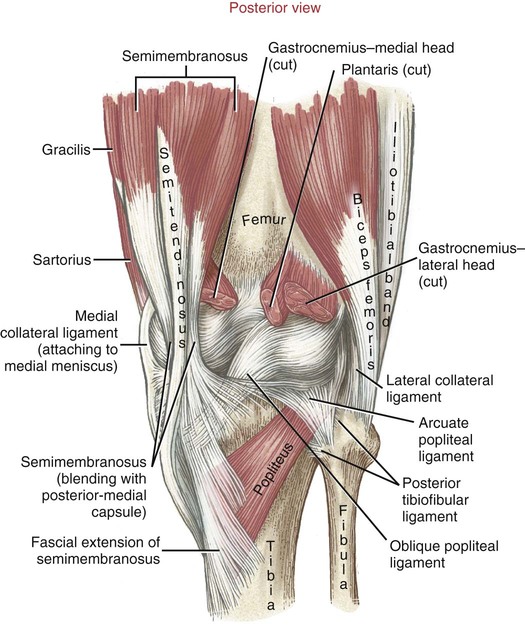
Posterior Capsule
Kinematics
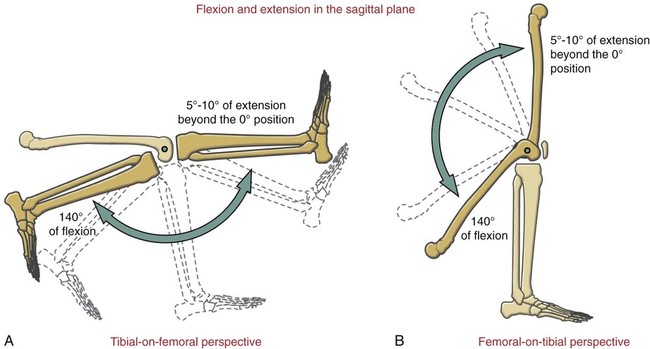
Osteokinematics of the Tibiofemoral Joint
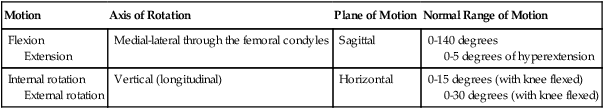
![]() Table 10-2
Table 10-2
Motion
Axis of Rotation
Plane of Motion
Normal Range of Motion
Flexion
Extension
Medial-lateral through the femoral condyles
Sagittal
0-140 degrees
0-5 degrees of hyperextension
Internal rotation
External rotation
Vertical (longitudinal)
Horizontal
0-15 degrees (with knee flexed)
0-30 degrees (with knee flexed)