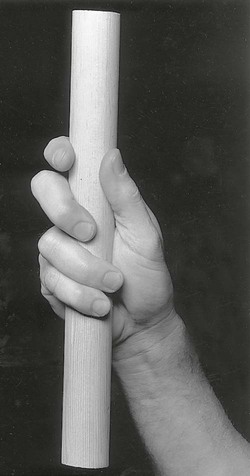
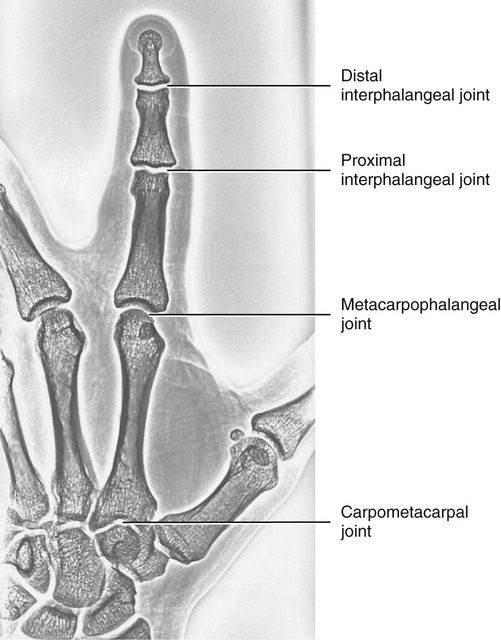
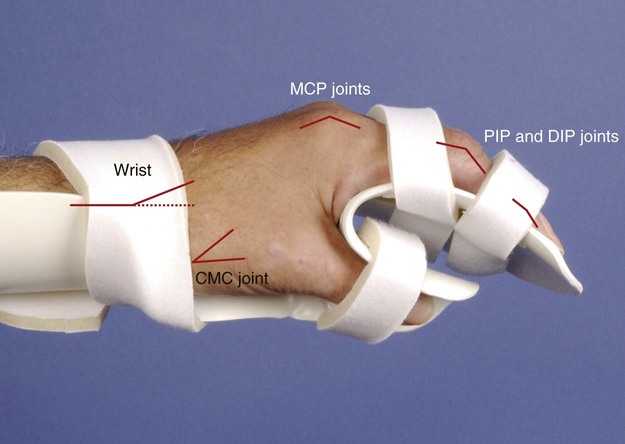
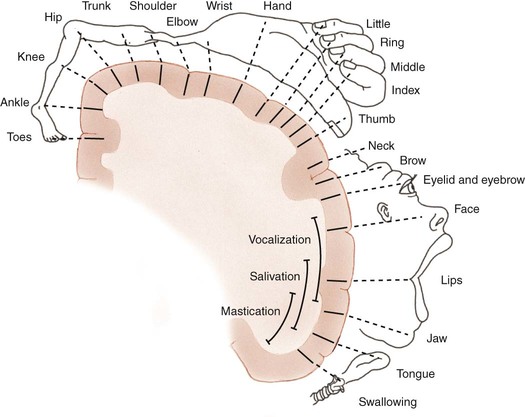
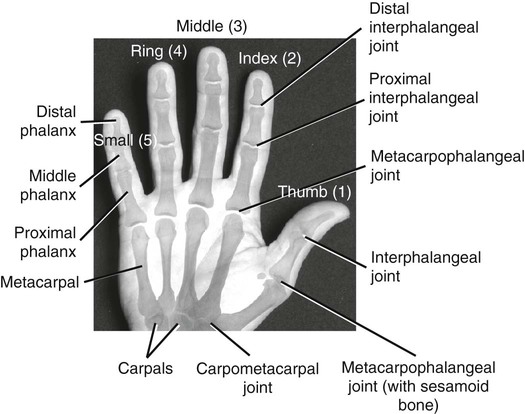
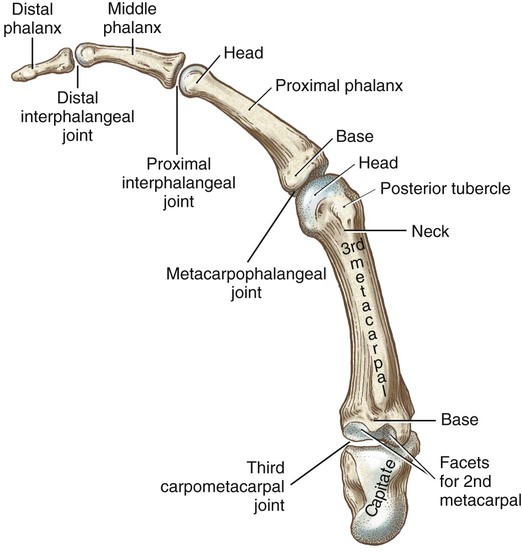
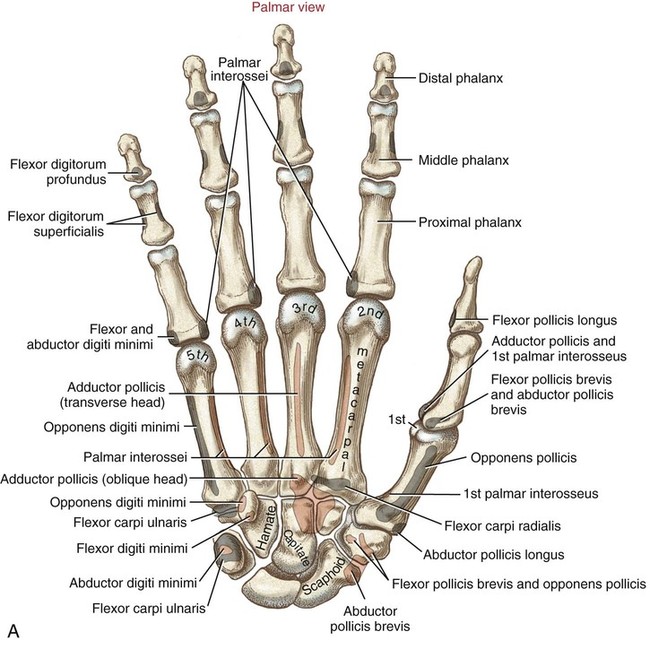
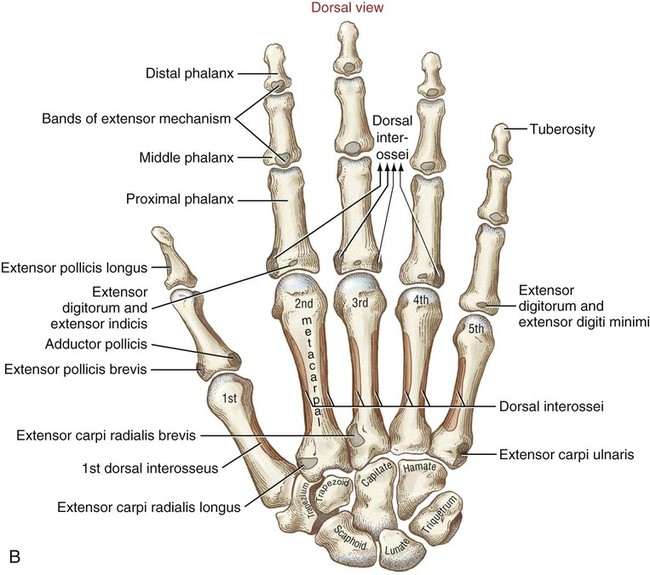
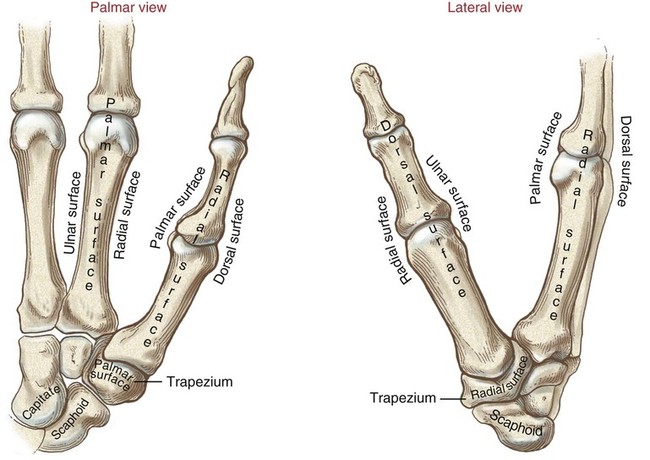
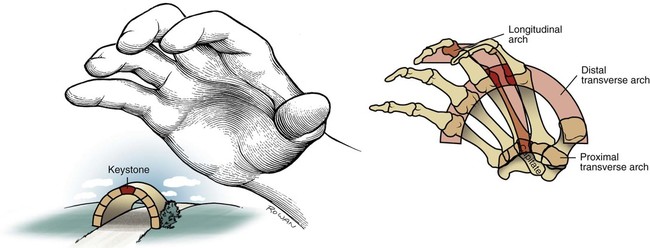
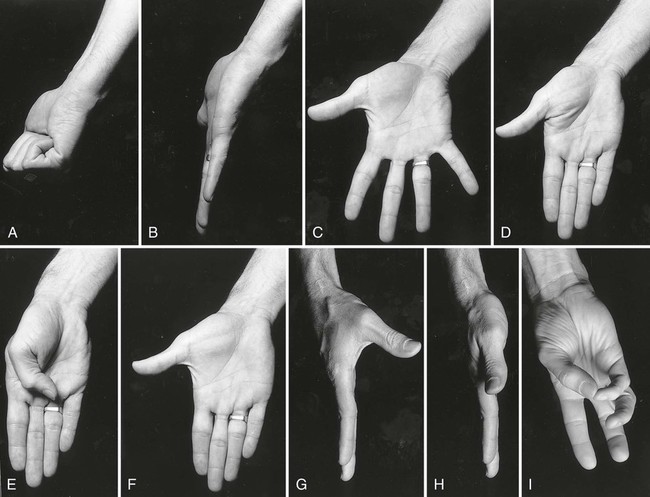
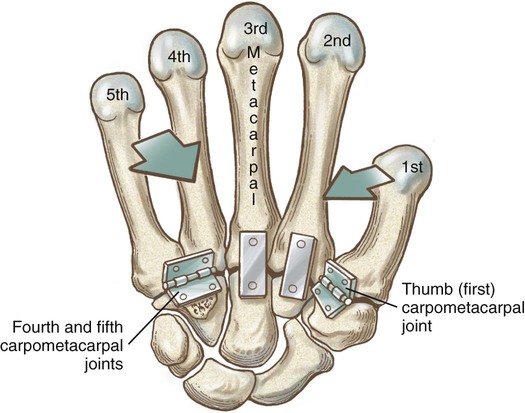
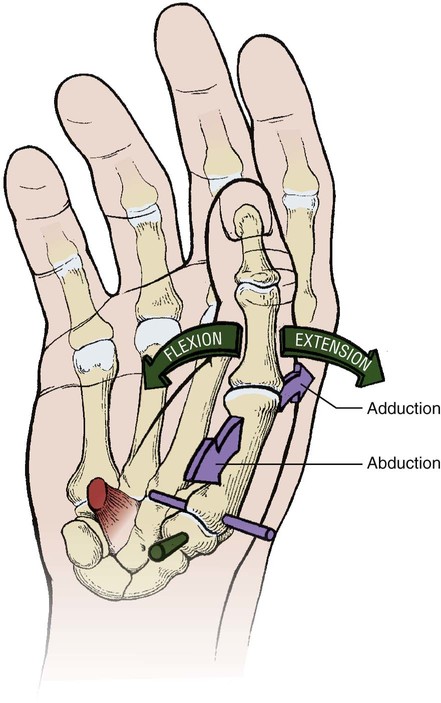
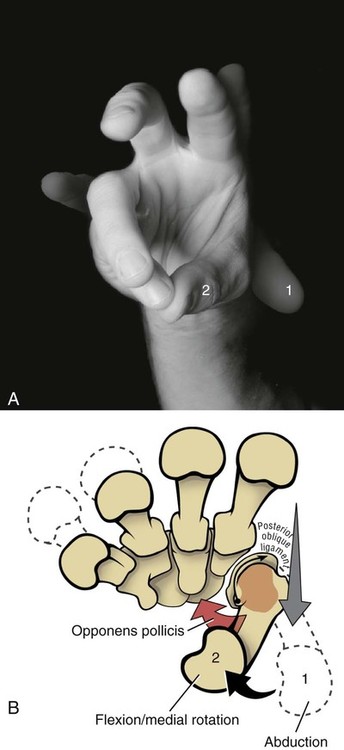
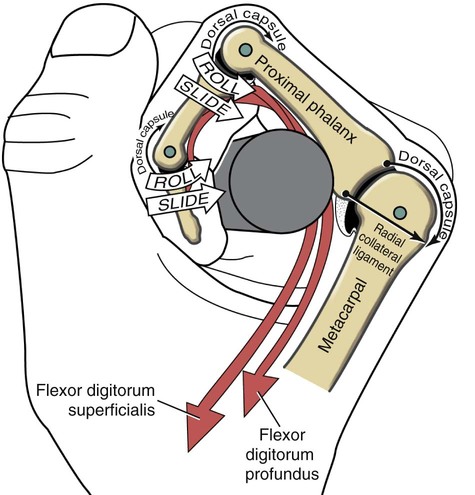
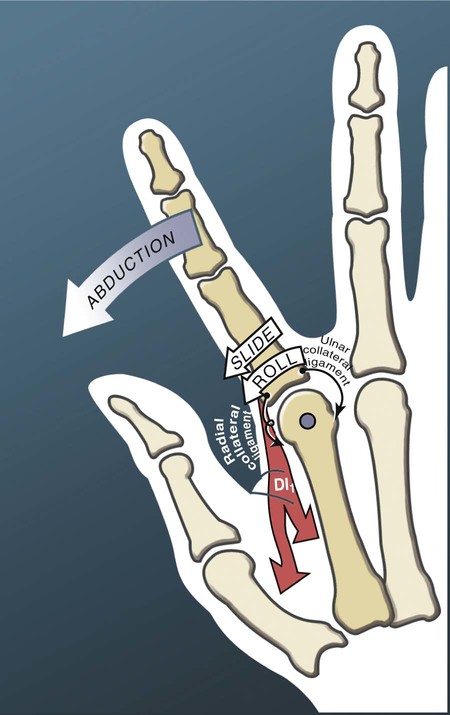
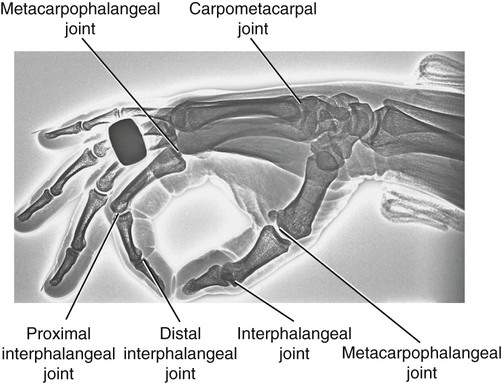
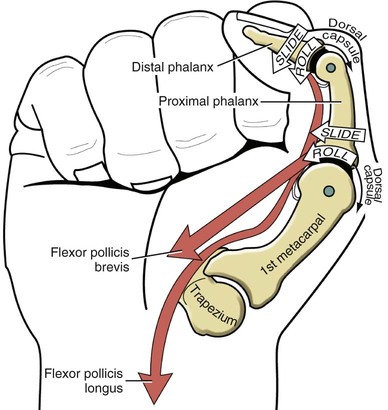
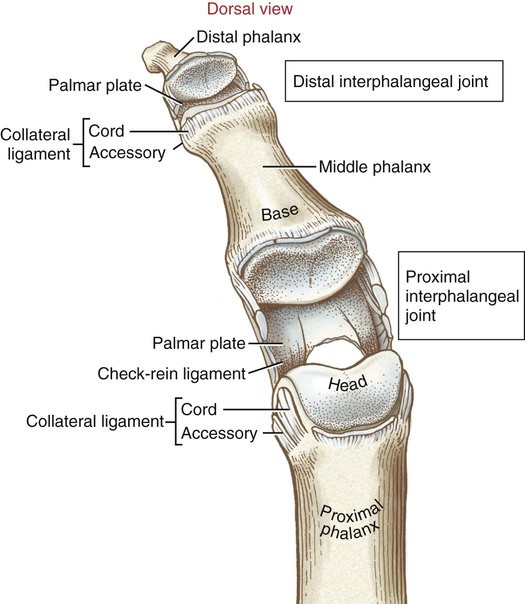
• Identify the bones and primary bony features of the hand. • Identify the carpometacarpal, metacarpophalangeal, proximal interphalangeal, and distal interphalangeal joints of the hand. • Describe the supporting structures of the hand. • Describe the planes of motion and axes of rotation for the motions of the hand. • Cite the proximal and distal attachments, as well as the innervation, of the muscles of the hand. • Justify the primary actions of the muscles of the hand. • Describe the primary mechanism that causes an ulnar drift deformity. • Describe the mechanics of a “tenodesis” grasp action of the wrist. • Explain the interaction between the intrinsic and extrinsic muscles when opening and closing the hand. • Explain why the fourth and fifth digits cannot be fully extended across all interphalangeal joints after a severance of the ulnar nerve. • Identify which active motions are lost (or severely weakened) after a cut of the median nerve at the level of the wrist. • Explain why an injury to the radial nerve would reduce the effectiveness and strength of one’s grasp. When functioning normally, the 19 bones and 19 joints of the hand produce amazingly diverse functions. The hand may be used in a primitive fashion such as a hook or a club or, more often, as a highly specialized instrument performing complex manipulations that require multiple levels of force and precision. Evidence of the hand’s enormous functional importance is evident by observing the disproportionately large area of the cortex devoted to the sensory and motor functions of the hand (Figure 7-1). A hand that is totally incapacitated by arthritis, pain, stroke, or nerve injury, for instance, can dramatically reduce the overall function of the entire upper limb. The function of the entire upper limb depends strongly on the function of the hand. The digits of the hand are designated numerically from one to five, or as the thumb and the index, middle, ring, and little (small) fingers (Figure 7-2). Each of the five digits contains one metacarpal and a group of phalanges. A ray describes one metacarpal bone and its associated phalanges. The articulations between the proximal end of the metacarpals and the distal row of carpal bones form the carpometacarpal joints (see Figure 7-2). The articulations between the distal end of the metacarpals and the proximal phalanges form the metacarpophalangeal (MCP) joints. Each finger has two interphalangeal (PIP) joints: A proximal interphalangeal joint and a distal interphalangeal joint (DIP). The thumb has only two phalanges and therefore only one interphalangeal joint. Each metacarpal has the following similar anatomic characteristics: Base, shaft, head, and neck. These characteristics are shown for the third ray in Figure 7-3. As is indicated in Figure 7-4, the first (thumb) metacarpal is the shortest and thickest, and the length of the remaining bones generally decreases in a radial-to-ulnar (medial) direction. With the hand at rest in the anatomic position, the thumb’s metacarpal is oriented in a plane different from that of the other digits. The second through fifth metacarpals are aligned generally side by side, with their palmar surfaces facing anteriorly. The position of the thumb’s metacarpal, however, is rotated almost 90 degrees medially (i.e., internally), relative to the other digits (see Figure 7-4). This rotated position places the sensitive palmar surface of the thumb toward the midline of the hand. In addition, the thumb’s metacarpal is positioned well anterior, or palmar, to the other metacarpals. This can be verified by observing your own relaxed hand. The location of the first metacarpal allows the entire thumb to sweep freely across the palm toward the fingers. Virtually all motions of the hand require the thumb to interact with the fingers. Without a healthy and mobile thumb, the overall function of the hand is significantly reduced. The medially rotated thumb requires unique terminology to describe its movement and position. In the anatomic position, the dorsal surface of the bones of the thumb (i.e., the surface where the thumbnail resides) faces laterally (Figure 7-5). Therefore, the palmar surface faces medially, the radial surface anteriorly, and the ulnar surface posteriorly. The terminology used to describe the surfaces of the carpal bones and all bones of the fingers is standard: The palmar surface faces anteriorly, the radial surface faces laterally, and so forth. The hand has 14 phalanges. The phalanges within each finger are referred to as proximal, middle, and distal (see Figure 7-4). The thumb has only a proximal and a distal phalanx. Except for differences in size, all phalanges within a particular digit have similar morphology (see Figure 7-3). Observe the natural arched curvature of the palmar surface of your relaxed hand. Control of this concavity allows the human hand to securely hold and manipulate objects of many and varied shapes and sizes. This palmar concavity is supported by three integrated arch systems: Two transverse and one longitudinal (Figure 7-6). The proximal transverse arch is formed by the distal row of carpal bones. This static, rigid arch forms the carpal tunnel, permitting passage of the median nerve and many flexor tendons coursing toward the digits. As with most arches in buildings and bridges, the arches of the hand are supported by a central keystone structure. The capitate bone is the keystone of the proximal transverse arch. Before progressing to the study of the joints, the terminology that describes the movement of the digits must be defined. The following descriptions assume that a particular movement starts from the anatomic position, with the elbow extended, the forearm fully supinated, and the wrist in a neutral position. Movement of the fingers is described in the standard fashion using the cardinal planes of the body: Flexion and extension occur in the sagittal plane, and abduction and adduction occur in the frontal plane (Figure 7-7, A through D). In most other regions of the body, abduction and adduction describe movement of a bony segment toward or away from the midline of the body; however, abduction and adduction of the fingers is described as motion toward (adduction) or away (abduction) from the middle finger. Because the entire thumb is rotated almost 90 degrees in relation to the fingers, the terminology used to describe thumb movement is different from that used for the fingers (Figure 7-7, E through I). Flexion is the movement of the palmar surface of the thumb in the frontal plane across and parallel with the palm. Extension returns the thumb back toward its anatomic position. Abduction is the forward movement of the thumb away from the palm in a sagittal plane. Adduction returns the thumb to the plane of the hand. Opposition is a special term that describes the movement of the thumb across the palm, making direct contact with the tips of any of the fingers. This special terminology, which is used to define the movement of the thumb, serves as the basis for the naming of the “pollicis” (thumb) muscles, for example, the opponens pollicis, the extensor pollicis longus, and the adductor pollicis. The carpometacarpal (CMC) joints of the hand form the articulation between the distal row of carpal bones and the bases of the five metacarpal bones. These joints are positioned at the extreme proximal region of the hand (see Figures 7-3 and 7-4). The basis for all movement within the hand starts at the CMC joints—at the most proximal region of each ray. Figure 7-8 shows a simplified illustration of relative mobility at the CMC joints. The joints of the second and third digits, shown in gray, are rigidly joined to the distal row of carpal bones, forming a stable central pillar throughout the hand. In contrast, the peripheral CMC joints (shown in green) form mobile radial and ulnar borders, which are capable of folding around the hand’s central pillar. The CMC joints of the hand transform the palm into a gentle concavity, greatly improving dexterity. This feature is one of the most impressive functions of the human hand. Cylindrical objects, for example, can fit snugly into the palm, with the index and middle digits positioned to reinforce grasp (Figure 7-9). Without this ability, the dexterity of the hand is reduced to a primitive, hinge-like grasping motion. The CMC joint of the thumb is located at the base of the first ray, between the metacarpal and the trapezium (see Figure 7-5). This joint is by far the most complex and likely the most important of the CMC joints, enabling extensive movements of the thumb. Its unique saddle shape allows the thumb to fully oppose, thereby easily contacting the tips of the other digits. Through this action, the thumb is able to encircle objects held within the palm. The CMC joint of the thumb is the classic saddle joint of the body (Figure 7-10). The characteristic feature of a saddle joint is that each articular surface is convex in one dimension and concave in the other—just like the saddle on a horse. This shape allows maximal mobility and stability. Motions at the CMC joint occur primarily in 2 degrees of freedom (Figure 7-11). Abduction and adduction occur generally in the sagittal plane, and flexion and extension occur generally in the frontal plane. Opposition and reposition of the thumb are special movements that incorporate the two primary planes of motion. The kinematics of opposition and reposition is discussed after the two primary motions are considered. For ease of discussion, Figure 7-12, A, shows the full arc of opposition divided into two phases. In phase 1, the thumb metacarpal abducts. In phase 2, the abducted metacarpal flexes and medially rotates across the palm toward the small finger. Figure 7-12, B, shows the detail of the kinematics of this complex movement. Muscle force, especially from the opponens pollicis, helps guide and rotate the metacarpal to the extreme medial side of the articular surface of the trapezium. The metacarpophalangeal (MCP) joints, or knuckles, of the fingers are relatively large articulations formed between the convex heads of the metacarpals and the shallow concave proximal surfaces of the proximal phalanges (Figure 7-13). Motion at the MCP joint occurs predominantly in two planes: (1) Flexion and extension in the sagittal plane, and (2) abduction and adduction in the frontal plane. Figure 7-14 illustrates many of the supporting structures of MCP joints. • Capsule: Connective tissue that surrounds and stabilizes the MCP joint • Radial and ulnar collateral ligaments: Cross the MCP joints in an oblique palmar direction; limit abduction and adduction; become taut on flexion • Fibrous digital sheaths: Form tunnels or pulleys for the extrinsic finger flexor tendons; contain synovial sheaths to help lubrication • Palmar (or volar) plates: Thick fibrocartilage ligaments or “plates” that cross the palmar side of each MCP joint; these structures limit hyperextension of the MCP joints • Deep transverse metacarpal ligaments: These three ligaments merge into a wide, flat structure that interconnects and loosely binds the second through fifth metacarpals Mechanical stability at the MCP joint is critical to the overall biomechanics of the hand. As discussed earlier, the MCP joints serve as keystones that support the mobile arches of the hand. In the healthy hand, stability at the MCP joints is achieved by an elaborate set of interconnecting connective tissues (Figure 7-14). As is shown in Figure 7-14, the concave component of an MCP joint is extensive, formed by the articular surface of the proximal phalanx, the collateral ligaments, and the dorsal surface of the palmar plate. These tissues form a three-sided receptacle that is aptly suited to accept the large metacarpal head. This structure adds to the stability of the joint and increases the area of articular contact. In addition to the motions of flexion and extension and abduction and adduction at the MCP joints, substantial accessory motions are possible. With the MCP joint relaxed and nearly extended, appreciate on your own hand the amount of passive mobility of the proximal phalanx relative to the head of the metacarpal. These accessory motions permit the fingers to better conform to the shapes of held objects, thereby increasing control of grasp (Figure 7-15). Figure 7-16 shows the kinematics of flexion of the MCP joints, controlled by two finger flexor muscles: The flexor digitorum superficialis and the flexor digitorum profundus. Flexion stretches and therefore increases tension in both the dorsal part of the capsule and the collateral ligaments. In the healthy state, this passive tension helps guide the joint’s natural arthrokinematics. Increased tension in the dorsal capsule and collateral ligaments stabilizes the joint in flexion; this is useful during grasp. The kinematics of extension of the MCP joints occurs in reverse fashion compared with that described for flexion. Figure 7-17 shows the kinematics of abduction of the MCP joint of the index finger, controlled by the first dorsal interosseus muscle. During abduction, the proximal phalanx rolls and slides in a radial direction: The radial collateral ligament becomes slack, and the ulnar collateral ligament is stretched. The kinematics of adduction of the MCP joints occurs in a reverse fashion. Abduction and adduction at the MCP joints occur to about 20 degrees on either side of the midline reference formed by the third metacarpal. The MCP joint of the thumb consists of the articulation between the convex head of the first metacarpal and the concave proximal surface of the proximal phalanx of the thumb (Figure 7-19). The basic structure of the MCP joint of the thumb is similar to that of the fingers. Active and passive motions at the MCP joint of the thumb are significantly less than those at the MCP joints of the fingers. For all practical purposes, the MCP joint of the thumb allows only 1 degree of freedom: Flexion and extension within the frontal plane. Unlike the MCP joints of the fingers, extension of the thumb MCP joint is usually limited to just a few degrees. From full extension, the proximal phalanx of the thumb can actively flex about 60 degrees across the palm toward the middle digit (Figure 7-20). Active abduction and adduction of the thumb MCP joint is limited and therefore these are considered accessory motions. The proximal and distal interphalangeal joints of the fingers are located distal to the MCP joints (see Figure 7-19). Each joint allows only 1 degree of freedom: Flexion and extension. From both a structural and a functional perspective, these joints are simpler than the MCP joints. The proximal interphalangeal (PIP) joints are formed by the articulation between the heads of the proximal phalanges and the bases of the middle phalanges (Figure 7-21). The distal interphalangeal (DIP) joints are formed through the articulation between the heads of the middle phalanges and the bases of the distal phalanges. The articular surfaces of these joints appear as a tongue-in-groove articulation similar to that used in carpentry to join planks of wood. This articulation helps limit motion at the PIP and DIP joints to flexion and extension only. Except for being smaller, the same ligaments that surround the MCP joints also surround the PIP and DIP joints. The capsule at each interphalangeal (IP) joint is strengthened by radial and ulnar collateral ligaments and a palmar plate. The collateral ligaments restrict any side-to-side movements, and the palmar (volar) plate limits hyperextension. In addition, the fibrous digital sheaths house the tendons of the extrinsic finger flexor muscles (see index and small fingers in Figure 7-14).
Structure and Function of the Hand
Osteology
Metacarpals
Phalanges
Arches of the Hand
Arthrology
Carpometacarpal Joints
Overview
Carpometacarpal Joint of the Thumb
Saddle Joint Structure
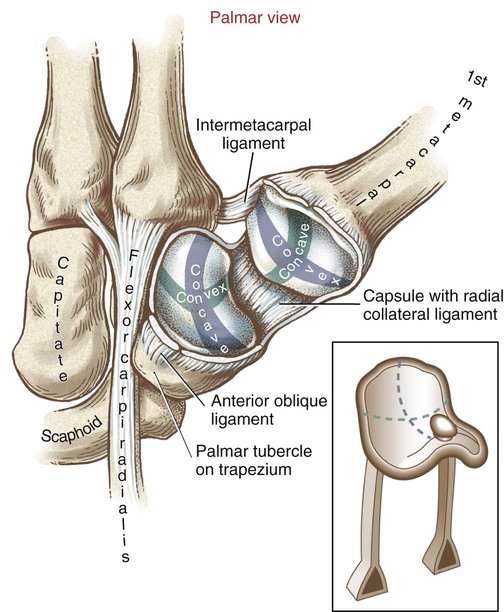
Kinematics
Metacarpophalangeal Joints
Fingers
General Features and Ligaments
Supporting Structures
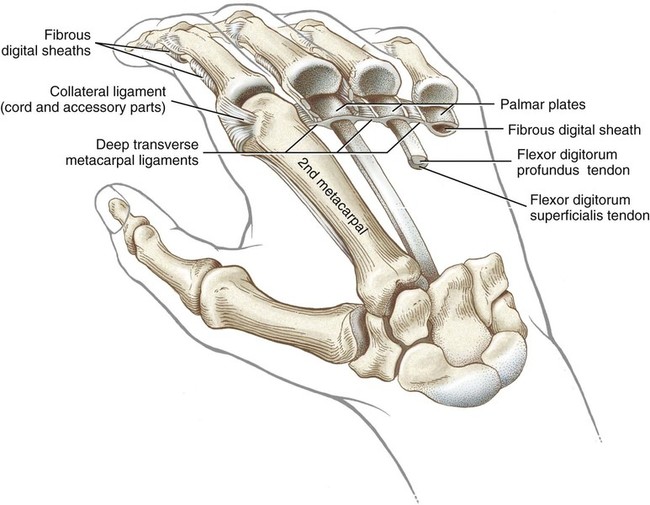
Kinematics

Thumb
Interphalangeal Joints
Fingers
General Features and Ligaments
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree