CHAPTER 95 Spinal Dural Injuries
Epidemiology
Traumatic Dural Injuries
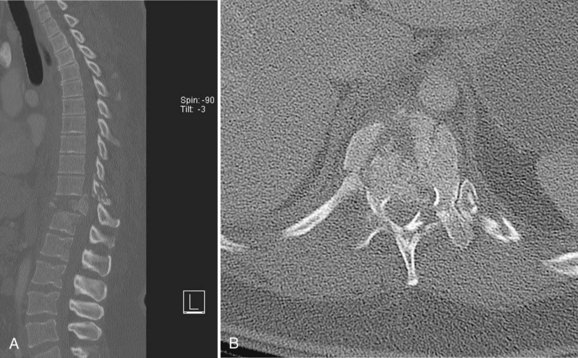
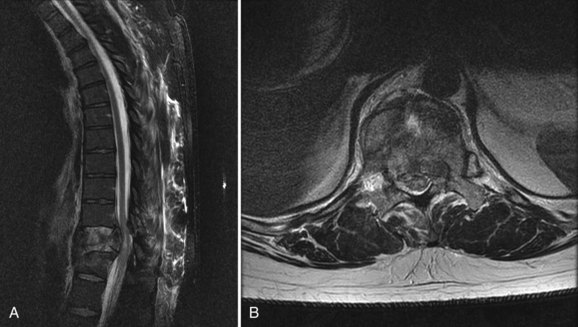
Traumatic dural injuries are typically the result of a traumatic mechanism and subsequent laceration of the thecal sac. These injuries occur relatively frequently in patients with thoracolumbar fractures secondary to the high-energy forces required to create these injuries (Figs. 95-1 and 95-2). Aydinli and colleagues1 reported traumatic dural injuries in 9 of 47 (19% of) lumbar burst fractures that were confirmed intraoperatively. Cammissa and colleagues2 reported a similar incidence of dural injuries in 11 of 60 (18% of) surgically treated thoracolumbar burst fractures. In a review of 60 patients with thoracolumbar and lumbar burst fractures, Carl and colleagues3 reported an anterior dural laceration in 6 of 60 (10% of) patients. In a survey of 28 lower lumbar burst fractures with posterior lamina “greenstick” fractures, dural tears were detected in seven (25% of) patients.4 In a traumatic setting it is important to recognize that an association between dural tears and neurologic deficit has been consistently reported likely due to either avulsion of the nerve root or entrapment of the neural elements in the fracture.2,5–7
Incidental Dural Injuries
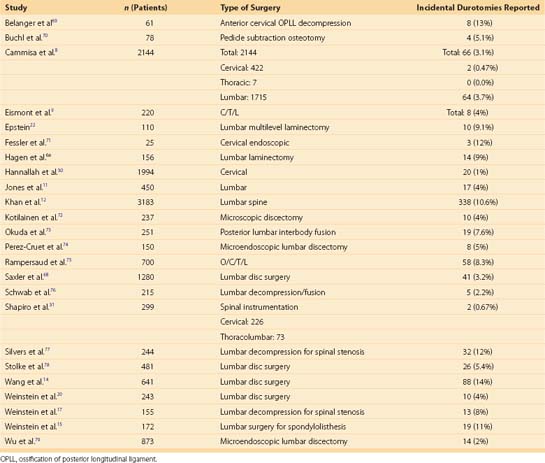
The current literature reports a wide variation in rates of dural injuries in spinal surgery. In surgery involving the lumbar spine, the incidence of dural tears is reported to be between 1% and 17%. The incidence of durotomy varies by series and type of surgical procedure performed (Table 95–1).8–17 Deyo and colleagues evaluated postoperative complications including dural injuries in a large series of elective lumbar spinal procedures.18 Of the patients with dural injuries, the overall morbidity was lower for younger patients and patients receiving lumbar discectomy. Conversely, the dural complication rate was greater with increased age and with procedures involving spinal stenosis or reoperations.
The increased incidence of dural injury with revision surgeries has been noted by numerous surgeons. A European survey of British spine surgeons revealed a durotomy incidence of 3.5% for primary discectomy, 8.5% for spinal stenosis surgery, and 13.2% for revision discectomy procedures.19 In a large review of 3183 patients, Khan reported iatrogenic surgical dural injuries were approximately twice as frequent (15.9% vs. 7.6%) in revision degenerative lumbar spine surgery as compared with primary cases.12 Further, in the multicenter, randomized Spine Patients Outcome Research Trials (SPORT) evaluating surgical decompression for lumbar discs, lumbar stenosis, and spondylolisthesis, the investigators found the risk of incidental durotomy increased 4% to 8% to 11% across these respective procedures.15,17,20
Dural disruption and subsequent cerebrospinal fluid leak occur via various mechanisms. They often result from dissection of adherent, fibrotic, or calcified tissue to the thecal sac; absence of dural tissue; or bone spikes produced during the laminectomy. Most commonly, direct trauma or laceration causes dural tears during spinal surgery. Dural entry is much more common in revision procedures, usually because of adhesions in the epidural space, dural scarring, fibrosis, and loss of surgical landmarks. Furthermore, in revision procedures there may be an absence of dural lining due to prior injury or chronic compression. Conditions that increase the risk of a dural injury during primary spinal procedures include eroded or thin dura, adhesions and fibrosis, or dural redundancy in patients with severe spinal stenosis.21 In a series of geriatric patients undergoing multilevel laminectomy, Epstein identified ossification of the yellow ligament, synovial cysts, and postoperative scarring as the main risk factors for intraoperative durotomy.22 Lack of surgical expertise and improper technique are believed to be independent risk factors for dural tears and have been reported to be correlated inversely to the surgeon’s experience.23,24 Excessive traction on severely herniated discs and anatomically incorrect screw placement have also been described as causative factors for dural laceration.25
Most dural injuries reported in the literature occur in the lumbosacral region. However, several studies have reported the occurrence of incidental durotomy in the thoracic and cervical spine.8,26–32 In a large series evaluating cervical spine surgery, durotomy was noted in 20 of 1994 (1% of) patients.30 Hannallah and colleagues30 reported the largest risk factor for the development of a cerebrospinal fluid leak in this series was the presence of an ossified posterior longitudinal ligament. The variation in the incidence rates of durotomies in the cervicothoracic spine and the lumbosacral spine has been attributed to both anatomic variation and the frequency of surgical site distribution.33
Clinical Diagnosis
Although many opportunities for effective treatment of incidental durotomy may exist, prompt diagnosis and repair are most important for management.25 Detection of dural tears may occur in both the intraoperative and postoperative settings, exposed by a CSF leak. Intraoperatively, fluid extravasation will typically be visualized directly in the operating theater after incidental durotomy as a rush of clear spinal fluid through the dural rent. Unexplained excessive epidural bleeding or a collapsed thecal sac could be an indirect sign of dural opening. Occasionally, the dural opening will go unnoticed until the postoperative period, where detection may become more difficult.25 Late-presenting dural tears are much less common, having a frequency of 0.28%.8 It has been suggested that these dural openings may not be recognized intraoperatively secondary to an incomplete breech of the arachnoid membrane, and CSF leakage will occur postoperatively with increases in intradural pressure. Persistently clear or serosanguineous wound drainage following spinal surgery may suggest a dural tear and CSF fistula formation. CSF fistulas typically occur in the immediate postoperative period (1 to 7 days). If the diagnosis is in question, laboratory evaluation through electrophoresis for β-2-transferrin can be performed. This test has been shown to be a sensitive and specific test for the presence of cerebrospinal fluid.34–36 If a fluctuant mass is noted over the site after spine surgery, the diagnosis of pseudomeningocele must be considered. Pseudomeningoceles are believed to be formed by direct extravasation of CSF into soft tissues with eventual development of a fibrous capsule.37
Clinical Implications
Intraoperatively, dural injuries may complicate surgical progression. The loss of CSF will decrease the hydrostatic pressure and turgor of the thecal sac, leading to a collapse of the natural tamponade of the local epidural veins. This may lead to increased bleeding of sites that had been controlled previously.21 Dural openings are also associated with damage to the underlying neural elements. The mechanism of these injuries is similar to crush injuries leading to radicular and cauda equina type symptoms.33
Signs and symptoms of incidental durotomy are directly related to the continuous egress of CSF and the loss of dural turgor. Severe postural headache is a classic symptom of CSF overdrainage and dural injury. Decreased CSF pressure leads to a caudal displacement of neural contents, which stretches the meninges, thus resulting in a severe headache.38 Other potentially related sequelae also include vertigo, blurred vision, nausea, vomiting, fevers, and infection. Incidental durotomy has been demonstrated to have an association with intracranial hypotension, tonsillar herniation, and subdural hematoma or hygroma formation.39–43
Despite the frequency of dural tears in spinal surgery, meningitis is a rare complication reported to occur with a frequency of 0.18% of all spinal procedures.44 In the setting of a persistent CSF fistula, the risk of meningitis, epidural abscess, arachnoiditis, delay of wound healing, or wound infection are all significantly increased.25,45,46 With pseudomeningocele formation, localized nerve root entrapment or adhesions may produce radicular symptoms.47–49 Therefore postural headaches combined with increased sciatic pain may suggest the presence of a pseudomeningocele.48 These collections have also been reported to calcify49 and may result in spinal cord compression.51,52
Imaging
Imaging studies are able to verify the presence of a CSF leak and may potentially locate the site of dural injury postoperatively. Magnetic resonance imaging (MRI) is the study of choice due to the resolution of soft tissue structures and fluid. It is sensitive to the presence of a cerebrospinal fluid accumulation and pseudomeningoceles.33 Johnson and colleagues53 compared open surgical findings with MRI in 24 patients with suspected cerebrospinal fluid fistulas and found MRI was accurate in all 24 patients (100%). Cisternography, myelogram computed tomography (CT) scans, and gadolinium-enhanced magnetic resonance cisternography may be used in more complex cases, when a cerebrospinal fluid fistula is suspected clinically but not apparent on initial MRI. Additionally, a myelogram has the ability to detect the site of the CSF egress with real-time imaging.
Treatment
The most important aspect of treating a CSF leak is prevention. Careful preoperative planning and meticulous surgical technique should be exercised, particularly in patients at high risk for dural tears such as those with surgical revisions and spondylolisthesis.25 The optimal treatment of incidental durotomies remains primary repair. Dural openings discovered intraoperatively should undergo prompt, watertight primary repair.9,13,14,21 Adequate exposure of the tear and surrounding normal dura is necessary for the proper repair of a dural opening. Primary repair is typically obtained by 5-0 silk, Prolene, or Gore-Tex sutures. Eismont and colleagues9 report the use of running locked stitch, whereas most other authors advocate simple running or simple interrupted sutures 2 to 3 millimeters apart. In addition to sutures, adjuvant use of collagen matrix, fibrin glue, and Dermabond has been well-documented by various authors in the literature.14,54,55 For tears that cannot be closed without undue tension on the thecal sac, the use of a patch graft is recommended. Fat, fascial, and muscle grafts are also frequently used.8,14,56 After repair, the Trendelenburg position should be reversed to refill the dural sac in the area of the repair and a Valsalva maneuver should be performed to simulate an increase in intrathecal pressure. Finally, a tight fascial closure with nonabsorbable suture material is of extreme importance.25 The use of subfascial drain placement after an intraoperative durotomy is controversial, but recommendations vary by author. Eismont and colleagues9 reported on their experience with five patients and cautioned against their use to avoid possible formation of fistulous tracts. However, in more recent, larger series, authors advocate primary suture repair, a subfascial drain, and roughly 1 to 3 days of bed rest.8,12,14 Postoperative bedrest and analgesia are commonly used as adjuvant therapy, but one report suggests their use only in the event that the patient develops postoperative symptoms.54
Given the fact that not all dural tears will be recognized and repaired adequately intraoperatively, the need for postoperative treatment strategies still exists.25 Surgical reopening and reclosure of incidental durotomies have traditionally been considered the definitive treatment.57 With respect to the morbidity associated with reoperation under general anesthesia, several successful conservative methods have been described in an attempt to avoid a surgical revision procedure in the patient with a suspected postoperative CSF leak. Bedrest is frequently the first step in their conservative management. Abdominal binders and focal compression have been shown to be helpful in the conservative treatment of pseudomeningocele.58 By decreasing the CSF pressure differential between the intradural and extradural space, closed subarachnoid drainage has been successful in the treatment of CSF fistulas and pseudomeningoceles. Lumbar drainage of 120 to 360 mL/day for 3 to 5 days has been associated with a complete resolution in 90% to 92% of cases.13,59,60 Studies have shown complete resolution of a CSF fistula with bedrest, a watertight skin closure, and some form of ancillary CSF diversion.59,61 Epidural blood patching, which is frequently used for spinal headache, has been reported to successfully treat postoperative CSF fistulas and pseudomeningoceles.62–64 Patel and colleagues65 described successful treatment in which three of six cases with postoperative CSF fistulas were treated with a percutaneous fibrin sealant. Hughes and colleagues57 reported in a small series that when faced with a difficult and/or tenuous dural repair, a subfascial epidural drain can be used to successfully allow the dura to heal primarily with prolonged drainage. Surgical dural repair should be quickly undertaken in patients with a profuse CSF leak, a symptomatic pseudomeningocele, or those that failed conservative management.66