Chapter 70 Special Hand Disorders
Aneurysm, Thrombosis, and Embolism in Radial, Ulnar, and Digital Arteries
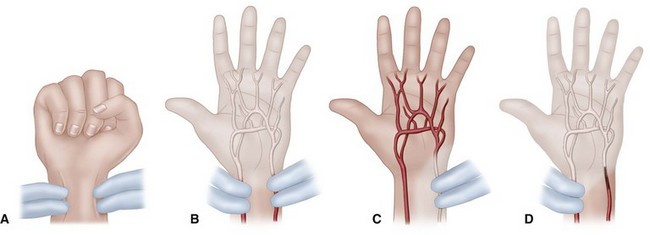
Symptoms of ischemia, pain, sensory changes, skin discoloration, ulceration, and necrosis can be aggravated by smoking, activity, and exposure to cold. Physical findings include hand or digital pallor or cyanosis, skin ulceration, necrosis distal to areas of occlusion, sensory and possibly motor changes of affected nerves, coolness to palpation, tenderness over an aneurysmal or thrombotic mass, a palpable thrill through an aneurysm, and lack of flow through the affected artery, which is shown by the Allen test (Figs. 70-1 and 70-2). Because of spasms in the distal vessels, this condition can be confused with other conditions, such as Raynaud disease. Plain radiographs, Doppler flow assessment, ultrasonography, pulse volume recordings, segmental arterial measurement, skin temperature measurement, radionuclide scanning, magnetic resonance angiography, and contrast angiography are helpful diagnostic measures. Angiography provides definitive information about the location and extent of the principal lesion and the presence of other circulatory problems in the upper extremity.
Although aneurysms may have atherosclerotic, mycotic, metabolic, and congenital origins, aneurysms seen in the hand and wrist usually are the result of trauma. Blunt trauma can cause true and false aneurysms (see Fig. 76-12), whereas penetrating trauma usually causes false aneurysms to form. Preoperative and intraoperative evaluations of the anatomy of the palmar vascular arch and of the quality of distal circulation are important when deciding between aneurysm excision alone and aneurysm excision with end-to-end repair and reversed vein graft arterial reconstruction. If the palmar arterial arch is complete, and distal circulation is adequate, as determined by pink distal skin color after release of the tourniquet or by pulse volume recordings showing a digital-brachial index of more than 0.7, repair or reconstruction usually is unnecessary. Conversely, if the palmar arterial arch is incomplete, or if the distal circulation is inadequate, the artery should be repaired or reconstructed with a reversed segmental vein graft (Fig. 70-3).
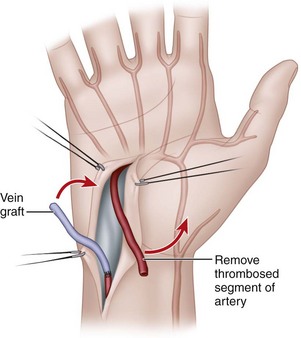
FIGURE 70-3 Resection of thrombosed segment and replacement with reversed vein graft.
(Redrawn from Koman LA, Urbaniak JR: Thrombosis of ulnar artery at the wrist. In American Academy of Orthopaedic Surgeons: Symposium on microsurgery: practical use in orthopaedics, St. Louis, 1979, Mosby.)
Although usually related to occupational or recreational trauma, arterial thrombosis in the wrist, palm, and fingers also can result from arterial cannulation in the forearm. The ulnar artery is the vessel most commonly affected by trauma-related thrombosis, probably because of a relative lack of protection at the wrist and its exposure to repeated forceful impacts, such as when the ulnar side of the wrist is used as a hammer. Sometimes the pain is severe, and sensibility is lost over the distribution of the ulnar nerve in the hand. Tenderness is present over the artery, and occasionally a feeling of fullness is described in the wrist and hand. Although the Allen test (see Figs. 70-1 and 70-2) is helpful in diagnosing thrombosis, arteriography is diagnostic.
Treatment options include exploration of the artery and resection of the entire thrombotic mass, arterial reconstruction with artery or vein grafts, local and regional sympathectomy, and palliation with medical and psychological methods. The history, physical examination, and Allen test determine the initial diagnosis. If the Allen test is positive, thermography, temperature probes, Doppler studies, and pulse volume recordings are used to confirm the diagnosis. If a stellate ganglion or brachial block relieves symptoms, treatment is observation. A stellate or brachial block may relieve vasospasm in acute thrombosis threatening digital survival. If symptoms are not relieved, arteriography is done, and, at the same time, intraarterial medications (reserpine or tolazoline) usually are given. Arteriography establishes the diagnosis, identifies the extent of the thrombosis and vascular disease, and determines the probable success of surgery. Symptomatic treatment is indicated if vascular disease is generalized. If symptoms diminish after arteriography, the patient can be observed. Surgery is indicated if symptoms persist and if digital survival is in question. After the thrombosed segment has been resected, the proximal end is clamped and the tourniquet is released. If backflow is good and pulse volume recordings of the ulnar digits are normal, the vessel is ligated, and the wound is closed. If backflow is poor, with no pulsatile flow on digital plethysmography, vein grafting should be considered. Contraindications to vein grafting include erythrocytosis, patient refusal to modify the environment, and patient refusal to discontinue smoking. If vein grafting is indicated, the entire thrombosed segment should be resected until normal intima is seen with the operating microscope. A reversed vein graft harvested from the forearm is inserted (see Fig. 70-3). Vein grafting is contraindicated if there is inadequate peripheral “runoff” on the arteriogram. Persistent symptoms after surgery can be controlled conservatively by cessation of smoking, biofeedback techniques, and intermittent administration of intraarterial medications; sympathectomy can be used as a last resort.
Arterial lacerations in the wrist and hand are discussed in Chapters 63 and 65. Arterial emboli in the upper extremity account for 15% to 20% of all emboli. About 70% of emboli in the upper extremity are believed to be of cardiac origin (e.g., through atrial fibrillation or as post–myocardial infarction mural thrombi); the remainder are related to the subclavian artery. Usually, acute arterial embolism is signaled by pallor, cold sensation, ischemic pain, paresthesia, occasional paralysis, and loss of palpable or Doppler-sensed pulses. Treatment includes intravenous administration of heparin, Fogarty catheter embolectomy, and warfarin (Coumadin) therapy. If the embolus significantly obstructs flow and cannot be removed, intraarterial administration of streptokinase has been effective if given within 36 hours of thrombosis and if not contraindicated. Newer thrombolytic agents, such as reteplase, may prove effective in the management of this problem.
Thermal Burns
Evaluation of patients with multiple burns proceeds as for patients with multiple acute injuries (see Chapter 65). Life-threatening injuries and extensive body burns take precedence over hand burns. Assessment for inhalation injury is essential because mortality from burns with associated inhalation injury approaches 35%, whereas mortality from burns without inhalation injury is only approximately 2%. Other measures essential to early management include taking appropriate radiographs, establishing intravenous lines, administering tetanus prophylaxis and antibiotics, preparing for blood transfusion, and conducting a careful physical examination. Preserving viable tissue, preventing infection, controlling fibrosis, and avoiding deforming contractures also take high priority in the management of a burn injury in the hand.
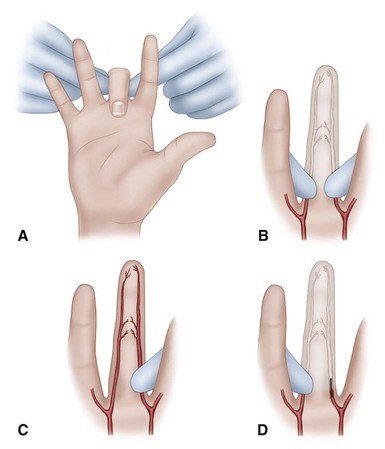
Although the initial examination may be difficult because of pain and other injuries, an estimation of burn depth is necessary (i.e., superficial, deep, full thickness, joint or tendon involvement) (Fig. 70-4). The judgment of the treating surgeon usually determines the estimation of burn depth. Other methods used for determination of burn depth range from wound biopsy to MRI. Although most techniques have limitations, noncontact laser Doppler imaging was found to be an accurate method to predict burn depth. Superficial burns (first degree) produce no blisters; although they are erythematous, capillary refill is good, sensation is intact, and the dermis is unharmed. Partial-thickness burns (second degree) are subdivided, depending on the extent of dermal injury, into superficial and deep. In superficial partial-thickness burns, some of the dermis is left intact, blisters may form, and capillary refill and sensation usually are present. Deep partial-thickness burns usually involve the entire dermis. Capillary refill may not be present, sensation usually is not intact, and thrombosed veins may be seen. In deep burns (third and fourth degree) with dermal and subcutaneous necrosis, the skin appears leathery, brown to black, and no circulation or sensation to the skin is present. The most important determination is the adequacy of distal circulation, especially if the burn has a circumferential component.
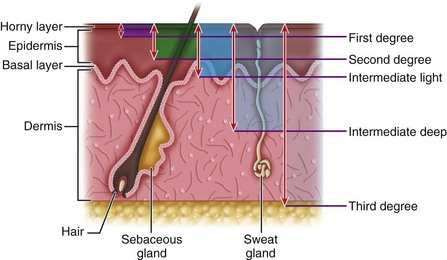
FIGURE 70-4 Classification of burns by anatomical depth.
(From Baux S: Thermal and chemical burns. In Tubiana R, editor: The hand, vol 3, Philadelphia, 1988, Saunders.)
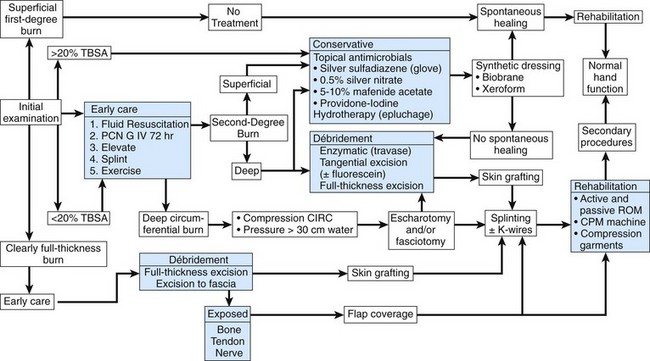
The depth of the burn, infection, and early management are major determinants of the functional and cosmetic outcome of hand burns. Other important factors are the location of the burn, the patient’s age, and the patient’s compliance with a rehabilitation program. There is agreement regarding the management of superficial hand burns and full-thickness and deeper burns. Superficial burns, if protected from additional injury and infection, should heal within 14 to 21 days with no significant impairment of hand function or cosmesis. Outpatient treatment usually is appropriate for these injuries. For partial-thickness burns (deep dermal, superficial full thickness), two approaches are advocated: (1) a “wait-and-see” method, with conservative treatment consisting of hydrotherapy, topical chemotherapy, and physiotherapy, and (2) an “operative” approach (in the first 3 to 5 days, as soon as practical), with tangential or full-thickness burn excision and early skin grafting (Fig. 70-5). Advocates of conservative treatment believe that with close follow-up and good patient cooperation patients who are treated with topical antimicrobials (silver nitrate, silver sulfadiazine, mafenide acetate, povidone-iodine), hydrotherapy, and an organized rehabilitation program may achieve long-term functional and cosmetic results similar to patients who undergo early surgical treatment. The risks and discomfort of the surgical route are avoided. Falcone and Edstrom proposed an algorithm for management of hand burns that allows flexibility for appropriate, timely treatment, depending on burn depth and apparent wound healing (Fig. 70-6).
For deep full-thickness burns (third and fourth degree), primary full-thickness excision of the burn wound with skin grafting is the appropriate treatment (Fig. 70-7). When tendons, nerves, vessels, ligaments, bones, and joints are damaged by thermal injury, measures in addition to burn wound excision and split skin grafting may be required. Stabilization of bones and joints with Kirschner wires, arthrodesis of destroyed joints, local and remote pedicled skin flaps, and free tissue transfers may be needed to preserve a viable, functioning hand. (For additional information, see Chapter 67 for fractures, Chapter 73 for arthrodesis, Chapter 65 for flaps, and Chapter 63 for microvascular flaps.)
Escharotomy
 Prepare the patient preoperatively for blood transfusion.
Prepare the patient preoperatively for blood transfusion.
 With the patient supine, usually under general anesthesia and with the upper extremity extended on the hand table, thoroughly clean the extremity with an antiseptic and drape it.
With the patient supine, usually under general anesthesia and with the upper extremity extended on the hand table, thoroughly clean the extremity with an antiseptic and drape it.
 Make medial and lateral midaxial longitudinal incisions through the eschar using an electrocautery cutting current. At the elbow, make the medial incision anterior to the medial epicondyle to avoid the ulnar nerve. Stop the incisions at the metacarpophalangeal joints.
Make medial and lateral midaxial longitudinal incisions through the eschar using an electrocautery cutting current. At the elbow, make the medial incision anterior to the medial epicondyle to avoid the ulnar nerve. Stop the incisions at the metacarpophalangeal joints.
 If muscle compartments are tense, or if intracompartmental pressures are elevated, perform fasciotomies on the forearm and hand compartments (see Chapters 74 and 75).
If muscle compartments are tense, or if intracompartmental pressures are elevated, perform fasciotomies on the forearm and hand compartments (see Chapters 74 and 75).
 Evaluate the adequacy of distal perfusion (skin color, warmth, and pulsatile flow in the hand and digits with the Doppler probe). If finger perfusion is unsatisfactory, perform digital escharotomies on the involved fingers, using pinpoint electrocautery along only the ulnar sides of the digits from the distal phalanges to the finger web spaces.
Evaluate the adequacy of distal perfusion (skin color, warmth, and pulsatile flow in the hand and digits with the Doppler probe). If finger perfusion is unsatisfactory, perform digital escharotomies on the involved fingers, using pinpoint electrocautery along only the ulnar sides of the digits from the distal phalanges to the finger web spaces.
 Make a longitudinal incision between the digital neurovascular bundles and the extensor tendons.
Make a longitudinal incision between the digital neurovascular bundles and the extensor tendons.
 Make the incision for thumb escharotomy along the radial side of the thumb from the distal phalanx to the base of the thumb, avoiding the digital neurovascular bundle.
Make the incision for thumb escharotomy along the radial side of the thumb from the distal phalanx to the base of the thumb, avoiding the digital neurovascular bundle.
 Additional dorsal longitudinal intermetacarpal incisions between the index-middle and the ring-little metacarpals allow access for release of the interosseous fascia, if needed.
Additional dorsal longitudinal intermetacarpal incisions between the index-middle and the ring-little metacarpals allow access for release of the interosseous fascia, if needed.
 Obtain meticulous hemostasis with electrocautery.
Obtain meticulous hemostasis with electrocautery.
 Use a Doppler probe to assess distal flow.
Use a Doppler probe to assess distal flow.
 Apply a nonadhering, medicated gauze and a bulky, nonconstricting dressing.
Apply a nonadhering, medicated gauze and a bulky, nonconstricting dressing.
Tangential Excision
(RUOSSO, WEXLER, BRCIC, MODIFIED)
 After inducing general anesthesia, place the patient supine and support the upper limb on the hand table. Apply a well-padded pneumatic tourniquet. Thoroughly clean the limb with antiseptic soap solution, with attention to the nails and removal of blebs and loose surface debris. The tourniquet can be used intermittently to control bleeding and to allow inspection for bleeding during the excision.
After inducing general anesthesia, place the patient supine and support the upper limb on the hand table. Apply a well-padded pneumatic tourniquet. Thoroughly clean the limb with antiseptic soap solution, with attention to the nails and removal of blebs and loose surface debris. The tourniquet can be used intermittently to control bleeding and to allow inspection for bleeding during the excision.
 Suspend the hand to an overhead pulley if needed for excision of the forearm and arm wounds. Usually this is unnecessary for hand excision.
Suspend the hand to an overhead pulley if needed for excision of the forearm and arm wounds. Usually this is unnecessary for hand excision.
 Exsanguinate the limb, and inflate the tourniquet.
Exsanguinate the limb, and inflate the tourniquet.
 Using a guarded knife or a dermatome, shave the burned areas tangentially in layers about 0.010-inch thick until punctate bleeding is encountered when the tourniquet is deflated. Shave the dermal and subcutaneous tissues containing venous thrombosis until healthy, bleeding tissue is encountered.
Using a guarded knife or a dermatome, shave the burned areas tangentially in layers about 0.010-inch thick until punctate bleeding is encountered when the tourniquet is deflated. Shave the dermal and subcutaneous tissues containing venous thrombosis until healthy, bleeding tissue is encountered.
 Deflate the tourniquet, and obtain hemostasis by electrocautery.
Deflate the tourniquet, and obtain hemostasis by electrocautery.
 Apply topical thrombin, and cover the hand with warm, saline-soaked sponges.
Apply topical thrombin, and cover the hand with warm, saline-soaked sponges.
 If satisfactory hemostasis has been achieved, and if there are no areas of questionable viability, apply a split-thickness skin graft as a sheet or meshed and unopened.
If satisfactory hemostasis has been achieved, and if there are no areas of questionable viability, apply a split-thickness skin graft as a sheet or meshed and unopened.
 Place darts in skin folds at the interdigital webs and in the thumb-index web.
Place darts in skin folds at the interdigital webs and in the thumb-index web.
 Suture or staple the graft in place.
Suture or staple the graft in place.
 Apply a dressing of nonadherent gauze covered with a synthetic compress (Acrilan) soaked in saline or glycerin.
Apply a dressing of nonadherent gauze covered with a synthetic compress (Acrilan) soaked in saline or glycerin.
 Support the hand in a fiberglass or plaster splint with the wrist extended, the metacarpophalangeal joints flexed, the interphalangeal joints slightly flexed, and the thumb in palmar abduction.
Support the hand in a fiberglass or plaster splint with the wrist extended, the metacarpophalangeal joints flexed, the interphalangeal joints slightly flexed, and the thumb in palmar abduction.
 If excessive bloody oozing occurs, or if tissue viability is uncertain, apply a saline-moistened dressing or a biological dressing (Biobrane, heterograft, allograft), and support the hand with a splint. Repeat the process in 24 to 48 hours.
If excessive bloody oozing occurs, or if tissue viability is uncertain, apply a saline-moistened dressing or a biological dressing (Biobrane, heterograft, allograft), and support the hand with a splint. Repeat the process in 24 to 48 hours.
Full-Thickness Excision
 Position and prepare the patient as for tangential excision. Inflate the pneumatic tourniquet just before excision, and deflate it when the excision is completed. Cleanse the limb, including the nails, with antiseptic soap.
Position and prepare the patient as for tangential excision. Inflate the pneumatic tourniquet just before excision, and deflate it when the excision is completed. Cleanse the limb, including the nails, with antiseptic soap.
 With the limb supported on a hand table, identify the boundaries of the burn wound to be excised. Mark the boundaries of burn excision with a skin pencil, making a pattern that conforms to the skin creases, avoiding tension lines at the skin-graft and graft-graft junctures. Extend the excision pattern into the finger and thumb-index webs to prevent finger scar syndactyly and thumb-index web contracture.
With the limb supported on a hand table, identify the boundaries of the burn wound to be excised. Mark the boundaries of burn excision with a skin pencil, making a pattern that conforms to the skin creases, avoiding tension lines at the skin-graft and graft-graft junctures. Extend the excision pattern into the finger and thumb-index webs to prevent finger scar syndactyly and thumb-index web contracture.
 Exsanguinate the limb with an elastic wrap, and inflate the pneumatic tourniquet.
Exsanguinate the limb with an elastic wrap, and inflate the pneumatic tourniquet.
 Incise through the marked borders of the burn wound into the subcutaneous tissues. Identify and dissect in an edematous plane superficial to the dorsal veins and extensor tenosynovium dorsally and superficial to the flexor tenosynovium and digital neurovascular bundles on the palmar surface.
Incise through the marked borders of the burn wound into the subcutaneous tissues. Identify and dissect in an edematous plane superficial to the dorsal veins and extensor tenosynovium dorsally and superficial to the flexor tenosynovium and digital neurovascular bundles on the palmar surface.
 After all necrotic skin has been removed, apply topical thrombin to the wound and wrap the hand in warm, saline-moistened gauze sponges.
After all necrotic skin has been removed, apply topical thrombin to the wound and wrap the hand in warm, saline-moistened gauze sponges.
 Deflate the tourniquet, and remove it from the arm to prevent a venous tourniquet effect.
Deflate the tourniquet, and remove it from the arm to prevent a venous tourniquet effect.
 Maintain the hand under compression and elevation for a sufficient time to achieve hemostasis or to minimize significant bleeding—usually 10 to 15 minutes or longer.
Maintain the hand under compression and elevation for a sufficient time to achieve hemostasis or to minimize significant bleeding—usually 10 to 15 minutes or longer.
 Remove the wrap, and obtain hemostasis with electrocautery.
Remove the wrap, and obtain hemostasis with electrocautery.
 If satisfactory hemostasis can be achieved, position the metacarpophalangeal joints in flexion with transarticular Kirschner wires, if necessary, for dorsal burns and apply a sheet of split-thickness skin graft or mesh the graft (1 : 1 or 1 : 1.5) and apply it unopened to the dorsum of the hand. Suture the graft with interrupted 5-0 chromic gut suture or with small skin staples.
If satisfactory hemostasis can be achieved, position the metacarpophalangeal joints in flexion with transarticular Kirschner wires, if necessary, for dorsal burns and apply a sheet of split-thickness skin graft or mesh the graft (1 : 1 or 1 : 1.5) and apply it unopened to the dorsum of the hand. Suture the graft with interrupted 5-0 chromic gut suture or with small skin staples.
 If the burn is on the palmar surface, the metacarpophalangeal joints can be splinted in extension to avoid flexion contractures.
If the burn is on the palmar surface, the metacarpophalangeal joints can be splinted in extension to avoid flexion contractures.
 Apply a nonadhering gauze pad covered with a soft compression bandage of synthetic material (Acrilan).
Apply a nonadhering gauze pad covered with a soft compression bandage of synthetic material (Acrilan).
 Support the hand with a plaster or fiberglass splint or, if conditions permit, a previously fabricated thermoplastic splint with the wrist extended, the metacarpophalangeal joints flexed (dorsal burn), the interphalangeal joints slightly flexed, and the thumb in palmar abduction.
Support the hand with a plaster or fiberglass splint or, if conditions permit, a previously fabricated thermoplastic splint with the wrist extended, the metacarpophalangeal joints flexed (dorsal burn), the interphalangeal joints slightly flexed, and the thumb in palmar abduction.
 If the bleeding cannot be satisfactorily controlled, wrap the wound with a saline-moistened dressing or biological dressing (Biobrane [UDL Laboratories, Rockford, IL], heterograft, allograft) and return in 24 to 48 hours to apply a graft.
If the bleeding cannot be satisfactorily controlled, wrap the wound with a saline-moistened dressing or biological dressing (Biobrane [UDL Laboratories, Rockford, IL], heterograft, allograft) and return in 24 to 48 hours to apply a graft.
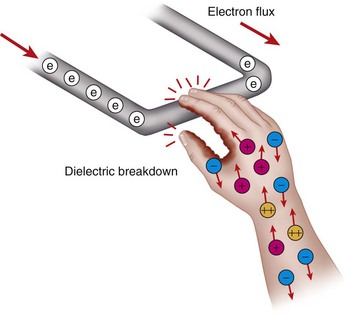
Electrical Burns
Electrical burns frequently involve the upper extremity. The dominant hand frequently is injured, and 50% of these injuries result in amputation. Tissue damage can result from a combination of thermal, electrical, and metabolic cellular factors. The extent of injury is determined by the characteristics of the injuring current, including the voltage, amperage, and resistance of the tissues; the duration of contact with the current; and the patient’s susceptibility to it (Fig. 70-8). Although the skin damage caused by electrical injury may be the most impressive presenting finding, significant deep injury may be present as determined by the route the electrical current takes through the body. Electrical injuries may involve the central and peripheral nervous systems, the cardiopulmonary and peripheral vasculature, the musculoskeletal system, the kidneys, and the skin. Initial management is directed at resuscitation. Appropriate diagnostic measures include radiographs of potential fractures and dislocations; electrocardiogram; and serum chemistries to assess electrolytes and liver, renal, cardiac, and skeletal muscle injury. Urine myoglobin levels and arterial blood gases are measured as well. The extent of injury to all systems should be evaluated, ensuring satisfactory hydration and urinary output, because patients with electrical burns may require more fluid resuscitation than might be calculated based on the injury to the total body surface area. Urinary output of 50 to 100 mL/hr is preferable. Recognizing, stabilizing, and reversing the effects of cardiac injury and the nephrotoxic effects of myoglobinuria and hemoglobinuria also are important. Because of the potential for hemorrhage from damaged vessels, a tourniquet should be kept near the patient’s bedside.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree