Soft Tissues about the Hip
Christopher O. Bayne
Adam G. Suslak
Shane J. Nho
Bryan T. Kelly
Introduction
The hip is a multiaxial, highly congruous, diarthrodial ball and socket joint comprised of the femoral head and its articulation with the acetabulum. It is a joint that allows for motion within three rotational axes, but its unique anatomic features also allow for great stability (1). The knowledge of the anatomy of the hip is of paramount importance to the physician interested in treating hip pathology. To help understand the anatomy of the hip and the related etiologic factors contributing to pain, Hammoud (2) has described the “layered approach” to the hip joint and hemipelvis.
Layer 1 is the osteochondral layer, whose structures include the femur, pelvis, and acetabulum. These structures define the mechanical alignment of the hip joint, provide joint congruence, and contribute to normal joint kinematics (2). The orientation of the hip’s osseous anatomy is such that the femoral head is largely contained within the bony confines of the socket, and the conformation of the femur within the acetabulum helps maintain a high degree of articular congruency. Abnormalities in this layer lead to: (1) dynamic impingement disorders secondary to femoral-sided cam impingement, acetabular-sided rim impingement, and angular and rotational deformities of the proximal femur including femoral varus and femoral retroversion; (2) static overload disorders secondary to acetabular deficiency (classic dysplasia), femoral valgus, and femoral anteversion.
In addition to its bony anatomy, the hip has an associated complex of soft tissue structures that contribute to articular congruency and impart additional stability. Layer 2 has been named the inert layer of the hip. The structures of this layer include the labrum, joint capsule, ligamentous complex, and the ligamentum teres (2). These structures contribute additional stability to the hip joint. Direct injury to these structures can occur secondary to osseous abnormalities or structural malalignment defined by the layer 1 anatomy. Layer 3 is known as the contractile layer of the hip and hemipelvis. It consists of 27 muscles crossing the hemipelvis and is responsible for the dynamic stability and muscular balance of the hip, pelvis, and trunk.(2). The fourth layer of the hip is the neurokinetic layer, and comprises the thoracolumbosacral plexus, lumbopelvic tissue, and lower extremity tissues. This layer is responsible for functional control of the entire lower limb (2).
The focus of this chapter will be on the soft tissue structures of layer 2 and layer 3 of the hip.
Layer 2
The structures of this layer include the labrum, joint capsule, ligamentous complex, and the ligamentum teres.
Labrum
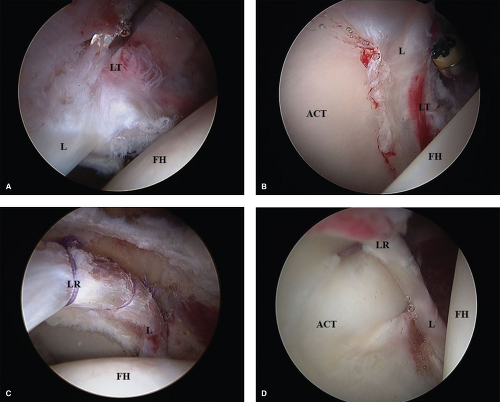
The labrum is a fibrocartilaginous extension of the bony acetabulum that nearly circumferentially attaches to the acetabular rim. It is a C-shaped structure opening distally, where its inferior insertions are contiguous with the transverse acetabular ligament (3). Functionally, the labrum deepens the acetabulum and increases the containment of the femoral head. The labrum also enhances joint stability through the restriction of synovial fluid flow into and out of the joint space, creating a resistance to the distraction of the femoral head from the acetabulum (4). It has been postulated that loss of the labral seal is often the critical event leading to destabilization of the hip (5) (Fig. 7.1).
Capsule
The hip capsule is a strong, dense, fibrous structure encapsulating the hip joint, providing stability, protection, and blood supply. It extends laterally from its acetabular attachment to surround the femoral head and neck. It is attached anteriorly to the intertrochanteric line and superiorly to the base of the femoral neck. Posteriorly it is attached approximately 1.25 cm superomedial to the intertrochanteric crest, and inferiorly it is attached to the femoral neck near the lesser trochanter (3,6). It is thickest anterior-superiorly and thinnest posterior-inferiorly. In patients with femoroacetabular impingement, the anterosuperior capsule is often a location for focal rim impingement and loss of femoral offset (6).
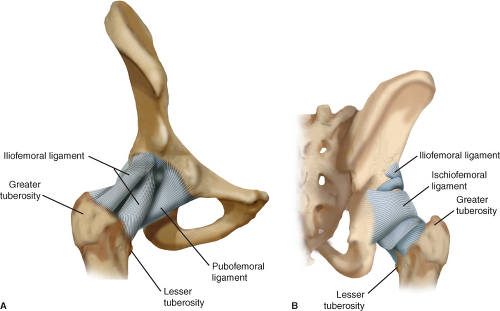
Morphologically, the capsule is composed of internal and external fibers (6). The internal fibers are composed of the synovium-lined and circumferential zona orbicularis fibers (3,7,8). The external fibers are longitudinally oriented and made up of the iliofemoral, ischiofemoral, and pubofemoral ligaments (3,7,8). Each of these ligaments has distinct functions that are important to the capsule and
along with the osseous structures constrain the dynamic range of motion of the joint (Fig. 7.2).
along with the osseous structures constrain the dynamic range of motion of the joint (Fig. 7.2).
Iliofemoral Ligament
Situated anteriorly, the triangular-shaped iliofemoral ligament (Y ligament of Bigelow) is the strongest of the capsular ligaments. It arises from the anterior inferior iliac spine (AIIS) of the pelvis and extends distally and laterally along the femoral neck to attach to the intertrochanteric line of the anterior femur. The iliofemoral ligament is composed of a medial and lateral arm. The medial arm originates between the AIIS and the iliac portion of the acetabular rim and inserts on a bump, or knob on the distal intertrochanteric line (9). The lateral arm originates proximal to the medial arm, closer to the AIIS. It inserts on the anterior greater trochanteric crest. It traverses more horizontally along the neck of the femur than the medial arm, covering the orbicular ligamentous fibers that run perpendicular to the lateral arm at its distal aspect (9) (Fig. 7.2).
The iliofemoral ligament is taut in positions of extension and external rotation of the hip and loose in flexion and internal rotation (10). Functionally, it resists anterior translation of the femoral head from within the acetabulum. The lateral arm of the iliofemoral ligament limits internal rotation in extension (9). During hip arthroscopy, part of the medial arm of the iliofemoral ligament making up the reflected capsule is resected off the acetabulum for rim trimming and labral reattachment. Hewitt et al. (6,7,11) demonstrated the ability of the iliofemoral ligament to withstand greater force than the other extrinsic ligaments, suggesting that iliofemoral insufficiency is associated with anterior hip instability and hip dislocations. Therefore, preservation or repair of the iliofemoral ligament may be of particular importance during arthroscopic and open hip procedures, particularly for patients with underlying instability or laxity (6).
Pubofemoral Ligament
Also located anteriorly is the weaker, triangular-shaped pubofemoral ligament. It is a sling-shaped structure that extends from the posterior iliopectineal eminence, superior ramus of the pubis, obturator crest, and obturator membrane to blend with the capsule and iliofemoral ligament. Proximally, it originates from the pubic portion of the acetabular rim and the obturator crest of the pubic bone. Distally, it attaches to the femoral neck, and its fibers blend with those from the medial arm of the iliofemoral ligament (Fig. 7.2). The sling of the pubofemoral ligament also courses inferiorly around the neck of the femur. It inserts inferior to the ischiofemoral ligament along the posterior intertrochanteric crest (Fig. 7.2). Functionally, its anatomic position serves to resist hyperextension and hyperabduction forces. It also controls external rotation in extension in conjunction with the medial and lateral arms of the iliofemoral ligament (9).
Ischiofemoral Ligament
Posteriorly situated along the femoral neck is the spiral-shaped ischiofemoral ligament. It extends from the posterior ischium, follows the spiral of the iliofemoral ligament as it crosses the joint, and attaches to the fibers of the posterior joint capsule and the posterior trochanteric crest (3,11,12) (Fig. 7.2). It does not extend the full length of the neck. As such, the posterior basocervical and intertrochanteric regions remain extracapsular (3). The ischiofemoral ligament crosses the hip capsule in two bands. The more superior band arches across the femoral neck to blend with the zona orbicularis, and the inferior band inserts more posteriorly along the intertrochanteric crest (9).
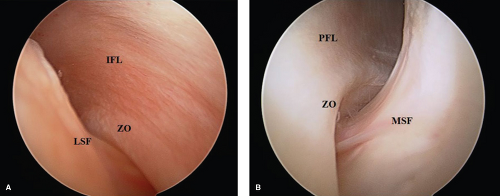
Zona Orbicularis
Although the majority of the fibers of the hip capsule are longitudinally oriented, the zona orbicularis is a circular ligamentous component of the capsule that circumferentially surrounds the femoral neck at its distal aspect (Fig. 7.3). The zona orbicularis separates the proximal and distal zones of the peripheral compartment (13). Ito et al. (8) looked at the contribution of the zona orbicularis and found the zona acted as a locking ring around the femoral neck to resist joint distraction.
In addition, a recent study by Field and Rajakulendran used dynamic magnetic resonance arthrograms of the hip to show the role of the zona orbicularis in synovial fluid circulation between the peripheral and central compartments. The bellows-like movement of the zona orbicularis during hip flexion causes a unidirectional flow of synovial fluid from the peripheral to central compartment (13). Extensive distal capsulotomies to the level of the intertrochanteric line may disrupt the zona orbicularis and may therefore need capsular repair to maintain hip stability and synovial flow.
Vascular Supply to Capsule
In addition to its structural role and contribution to the stability of the hip, the capsule also harbors the blood vessels to
the femoral head and acetabulum. Kalhor et al. (14) demonstrated that the blood supply to the hip arises from four main vessels. These are as follows: the superior gluteal artery, the inferior gluteal artery, the medial femoral circumflex artery, and the lateral femoral circumflex artery. Although the medial femoral circumflex artery is the main supplier of the femoral head, Kalhor et al. (14) noted an anatomic variation in which the inferior gluteal artery was the main supplier of the femoral head in 2 of 20 cadaver specimens. The superior and inferior gluteal arteries enter the capsule proximally and supply the posterior and posterior-superior aspect of the hip capsule. The medial and lateral femoral circumflex arteries enter distally and supply the anterior capsule (14,15).
the femoral head and acetabulum. Kalhor et al. (14) demonstrated that the blood supply to the hip arises from four main vessels. These are as follows: the superior gluteal artery, the inferior gluteal artery, the medial femoral circumflex artery, and the lateral femoral circumflex artery. Although the medial femoral circumflex artery is the main supplier of the femoral head, Kalhor et al. (14) noted an anatomic variation in which the inferior gluteal artery was the main supplier of the femoral head in 2 of 20 cadaver specimens. The superior and inferior gluteal arteries enter the capsule proximally and supply the posterior and posterior-superior aspect of the hip capsule. The medial and lateral femoral circumflex arteries enter distally and supply the anterior capsule (14,15).
Capsular Management During Hip Arthroscopy
Capsular management during hip arthroscopy is critical for adequate exposure while not compromising stability. Approaches for capsulotomy have included limited and extensile capsulotomy, and capsulectomy. The selected approach must take into consideration all symptomatology and pathoanatomy including central compartment and femoral side lesions, baseline hyperlaxity, and capsular adhesions.
Evaluation and treatment of the central compartment requires at minimum a limited capsulotomy. Standard anterolateral and anterior portals are established. Capsular releasing incisions with a beaver blade allow improved maneuverability (16,17). Further exposure for rim resection and treatment of labral pathology can be obtained by completing an interportal capsulotomy. Capsule management becomes even more important when addressing peripheral compartment lesions. Capsulectomy involves resecting the anterior capsule for exposure of the proximal femoral head–neck junction. This technique has been criticized because of potential anterior instability (18,19). The most common reason for revision surgery was inadequately treating CAM lesions (20,21). In addition, Matsuda (22) recognized the limits of preoperative imaging and therefore recommended arthroscopic surveillance of the proximal femur in all cases. Based on these findings we present our preferred method for capsular management.
Author’s Preferred Method
The patient is anesthetized and placed on a traction table with a well-padded perineal post. Traction is established by adduction and cantilever force over the perineal post. Image intensifier confirms appropriate joint distraction. Under fluoroscopic visualization, a standard ALP is utilized just proximal to the greater trochanter and anterior to the iliotibial band. Needle localization is utilized to establish an anterior portal with an outside-in technique. The ALP is approximately 1 cm lateral to the ASIS and in line with the ALP. A capsulotomy is then performed connecting the two portals. The reflected capsule on the superior acetabular rim is released from the level of the chondrolabral junction to the AIIS and indirect head of the rectus femoris insertion proximally. The central compartment is visualized and all indicated procedures are performed.
We routinely utilize a peritrochanteric distal anterolateral accessory portal (DALA) for anchor placement and later for peripheral compartment work. The arthroscope is placed in the ALP and needle localization is utilized to establish a DALA portal. This portal is in line with the ALP and approximately 4 to 6 cm distal.
The arthroscope is switched to the anterior portal. The light source is directed distally and laterally along the femoral neck. The traction is released and the hip is flexed approximately 30 degrees to release tension on the anterior capsule and increase peripheral compartment volume. An arthroscopic blade is introduced through the DALA portal.
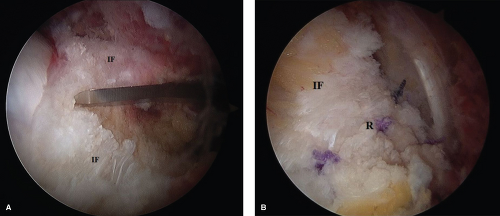
The capsule is incised perpendicularly from interportal capsulotomy to the intertrochanteric line. The capsular cut should be made along the center of the femoral neck. Skiving the blade in either direction can lead to injury to the femoral vessels (Fig. 7.4).
The capsule is incised perpendicularly from interportal capsulotomy to the intertrochanteric line. The capsular cut should be made along the center of the femoral neck. Skiving the blade in either direction can lead to injury to the femoral vessels (Fig. 7.4).
Once the capsulotomy is complete, a switching stick is introduced in the ALP. The switching stick is used as a retractor of the superior and inferior leafs of the capsule to improve visualization of the cam lesion. Fluoroscopic images taken at 45-degree angle to obtain a Dunn lateral view of the hip are frequently utilized to assess the extent of the cam lesion and retractor placement. The resector is inserted through the DALA portal for cam resection. Improved exposure superiorly and inferiorly can be obtained with repositioning of the switching stick either above or below the femoral neck. Increasing hip flexion angle to 45 degrees allows improved access to the distal femoral neck for larger cam lesions and visualization of the entire osteochondroplasty. Rotation of the hip in conjunction with fluoroscopic images helps improve access to anterior and posterior extents of the cam lesion. This technique provides 180-degree visualization of the cam lesion and osteochondroplasty without extensive capsulectomy. After the femoral head–neck osteochondroplasty is complete, a dynamic arthroscopic examination of the hip is performed. The hip is flexed to 60 degrees and rotated internally and externally ensuring there is no impingement on the labrum or subluxation of the femoral head. The medial extent of the resection should not violate the suction seal of the hip joint. Fluoroscopic images are used to assess anatomic recontouring of the femoral head–neck junction.
We routinely repair the capsule after the capsulotomy. This is done with the arthroscope in the anterior portal. A suture passer is utilized through the DALA portal. The longitudinal portion of the T capsulotomy is repaired to the level of the proximal osteochondroplasty, and the interportal capsulotomy is left open (Fig. 7.4).
Ligamentum Teres
The ligamentum teres is a pyramidal band ensheathed in a synovial membrane (3) (Fig. 7.5). It has a broad origin within the cotyloid fossa and pulvinar, blending with the entire transverse acetabular ligament. It extends to the periosteum of the ischium and capsule posteroinferiorly (23). It inserts on the fovea capitus, which is a bare area devoid
of articular cartilage, on the femoral head slightly posterior and inferior to its center. The mean length of the ligamentum is between 30 and 35 mm, with some variability in the literature (24). Within the ligamentum teres lies the acetabular branch of the obturator artery. The artery of the ligamentum teres offers a limited contribution to the vascularity of the femoral head.
of articular cartilage, on the femoral head slightly posterior and inferior to its center. The mean length of the ligamentum is between 30 and 35 mm, with some variability in the literature (24). Within the ligamentum teres lies the acetabular branch of the obturator artery. The artery of the ligamentum teres offers a limited contribution to the vascularity of the femoral head.
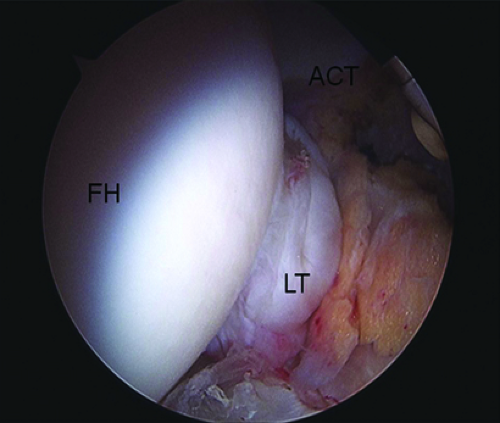 Figure 7.5. Arthroscopic photo of ligamentum teres illustrating its relationship with the femoral head and acetabulum. FH, femoral head; LT, ligamentum teres; ACT, acetabulum. |
The role of the ligamentum teres as a source of hip pain continues to be a debated topic because of its unclear role in hip stability (16). Despite improved radiographic imaging, arthroscopy remains the optimum technique for evaluation. The incidence of ruptures on arthroscopic findings has ranged from 4% to 15% (16,25). Byrd and Jones (16) found it was the third most common problem in his personal review of hip arthroscopy cases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree