CHAPTER 20 Small to Medium Rotator Cuff Tears
Arthroscopic rotator cuff repair (ARCR) has become the gold standard for treatment of the vast majority of rotator cuff lesions.1–16 Early concerns about repair integrity and durability have led to the anticipated evolution in anchors, suture material and, most importantly, surgical technique. We now have at our disposal an armamentarium of anchors made not only of metal, but poly-L-lactic acid, self-reinforced poly-DL-lactic acid, and polyetheretherketone (PEEK). Suture material has been vastly improved as a result of the introduction of Fiberwire and the many comparable enhanced strength suture materials.
PREOPERATIVE CONSIDERATIONS
With this infomation, the patient is appropriately counseled on the advisability of surgery, including its associated risks and potential outcomes. There has been ongoing debate regarding the need for surgical intervention in these smaller tears; however, most surgeons recognize the potential for enlargement of any tear over time, especially those with a traumatic cause. Currently, for any patient with a well-defined traumatic event, and otherwise normal shoulder function prior to that event, the recommendation is for immediate repair. Those individuals with no history of substantial trauma, yet ongoing symptoms and MRI confirmation of a tear, conservative nonsurgical care is offered, with the recommendation for follow-up and possible repeat MRI at 4 to 6 months. If symptoms are persistent, or are unrelieved with conservative measures, surgery and repair are recommended. Also, those patients with significant comorbidities that could strongly affect healing and/or rehabilitation, and those with compliance issues, are treated with conservative modalities, and surgery is reserved for those with increasing symptoms.
ARTHROSCOPIC ROTATOR CUFF REPAIR
Setup
All cases are performed with the patient in the lateral decubitus position, allowing ready access to the posterior, anterior, and superior aspects of the shoulder while holding the arm in a position of slight abduction, thereby facilitating approximation of the free tendon edge to the region of the greater tuberosity (Fig. 20-1). The arm is rotated as needed to optimize anchor placement and reduce tension during suture tying. In most patients, 10 pounds of traction at approximately 30 to 40 degrees of abduction is more than adequate to provide the proper shoulder position. Anesthesia is moved out of the immediate operative field to allow unimpeded access to the entire shoulder region.
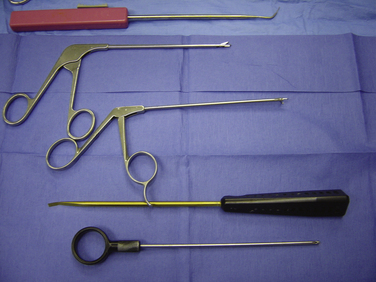
Every procedure begins with a basic set of instruments, including a simple knot pusher, ring grabber or crab claw device for retrieving individual sutures, set of cannulated suture passers, cannula for fluid management, and various suture retrievers (Fig. 20-2). Additional instruments can be added as neededs.
Portals
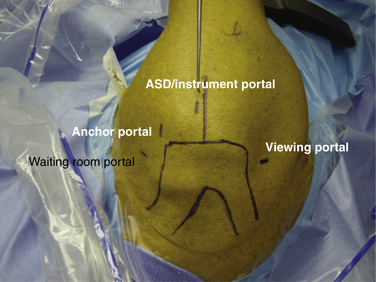
All arthroscopic repairs require three principal portals and an additional ancillary anterior portal. The viewing portal is located 1 cm medial and 2 cm inferior to the posterolateral corner of the acromion (Fig. 20-3). The arthroscopic subacromial decompression (ASD) instrument portal is located immediately anterior to the finish line, a line drawn perpendicular to the lateral margin of the acromion, beginning at the posterior extent of the acromioclavicular joint and 2 to 3cm lateral to the lateral margin of the acromion. The anchor portal location is determined during subacromial viewing using the needle localization technique; it is typically at the anterolateral corner of the acromion. An additional fourth portal may be made anterior to the acromion, called the waiting room portal. I use this for large tears in which three or more anchors and six or more sutures are involved. This portal allows me to dock sutures that are not being worked with anteriorly to free up the viewing area while posterior sutures are tied. This aids greatly in suture management.
Once the need for a repair has been determined, all portals are secured with cannula. The size of the cannula is dependent on the anticipated use of that portal. For example, the posterior portal is often used also for instrument access with the Spectrum (Conmed Linvatec, Largo, Fla) cannulated suture passer. This device requires at least an 8-mm opening and thus an 8-mm cannula. The anchor portal, however, is used almost exclusively for anchor insertion and knot tying, so a smaller 5-mm cannula is adequate. The lateral, or instrument portal, is sized according the instrument to be used for that repair. In most cases, and with most instruments, a 6- to 7-mm cannula is acceptable. Use of a cannula greatly diminishes fluid extravasation into the soft tissue, minimizes overall fluid requirements, and enhances visualization by maintaining hydrostatic pressure in the subacromial space. Cannulas also allow the surgeon to move the scope freely from portal to portal to improve visualization and prevent soft tissue from being entangled with sutures during passage and tying.
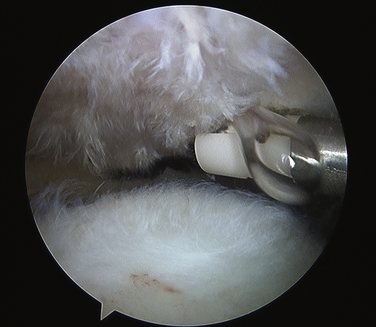
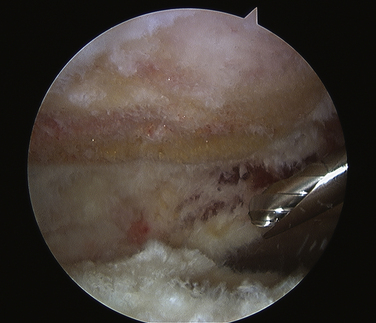
Acromioplasty
Although there has been debate regarding the need and efficacy of ASD in ARCR,17–19 an acromioplasty allows for enhanced visualization during the repair and increased room for instrumentation, and lessens the likelihood of later impingement of the repaired cuff. The ASD should require no more than 10 to 15 minutes to complete. To that end, in all chronic and many acute full thickness rotator cuff tears, I routinely perform a concomitant ASD. Viewing from the posterior portal, a bursectomy is performed to visualize the inferior surface of the acromion. If a large rotator cuff tear has been identified, the bursectomy is carried around the anterior, lateral, and posterior gutters to improve visualization and facilitate instrumentation of the subscapularis and/or infraspinatus tendons. When the bursectomy is complete, a radiofrequency (RF) device removes all residual soft tissue from the under surface of the acromion and releases the coracoacromial (CA) ligament from its attachment on the anteroinferior aspect of the acromion (Fig. 20-4). This is only a CA ligament release, not a resection. The burr is introduced from the lateral portal and the decompression begun at the anterolateral corner, working both medial and posterior (Fig. 20-5). An adequate decompression is achieved when the acromioplasty is tapered and terminates at or about the finish line (the line drawn at the time of initial portal placement; see earlier). Finally, the decompression is completed by moving the arthroscope to the lateral portal, bringing the burr in from the posterior portal and finished with a cutting block technique.