Fig. 1
This image shows a morphologically normal hip with adequate coverage of the femoral head

Fig. 2
This image shows the shallow acetabulum and decreased coverage consistent with skeletally mature acetabular dysplasia
Pathoanatomy of the Dysplastic Hip
Normal development of the hip joint is determined by numerous factors that are present during both the gestation and postpartum periods of a child’s life. The major driving force for proper morphologic development is concentric reduction of a spherical femoral head into the concave acetabulum. The femoral head provides a foci around which the acetabulum is shaped while the properly contained femoral head is in turn molded by the native acetabulum. Failure to achieve this interdependent concentric reduction will influence the ability of the native hip to develop appropriately.
Surrounding the edge of the femoral-acetabular junction is the labrum of the hip. This cartilaginous structure serves multiple functions in the healthy hip. It effectively increases the contact area between the acetabulum and the femoral head providing a greater surface area for force distribution. The labrum also creates a tight seal for the hip joint, which helps maintain a stable hip reduction, allows for smooth motion of the hip, and optimizes the fluid-film mechanics [1–3].
Skeletally mature acetabular dysplasia can prevent proper physiologic function due to the morphologic abnormalities affecting hip joint mechanics. The most common morphologic abnormality in SMAD is the presence of a shallow acetabulum with a lack of both anterior and lateral femoral head coverage; however, different morphologies also exist (Table 1) [4]. Approximately 40 % of patients will present with some degree of retroversion [5]. Dysplastic hips may also be associated with increased femoral anteversion and femoral neck valgus [6].
Table 1
Distribution of acetabular deficiency
Location of deficiency | Percentage (%) |
|---|---|
Lateral | 7 |
Anterior | 8 |
Posterolateral | 18 |
Anterolateral | 72 |
The ramifications of these morphologic abnormalities on the soft tissues of the hip are what cause the symptomatic nature of the condition. The deficient coverage leads to decreased surface area for force transmission and increased stress across a focused area of the joint cartilage and labrum. Increased loads at these focal areas lead to both physical microtrauma and physiologic changes within the soft tissues that lead to their degeneration [7, 8]. Decreased coverage and increased inclination of the articular surface along with anteversion and valgus of the femur can result in variable degrees of joint instability. Normal repetitive activities such as walking, running, and climbing stairs lead to increased shear forces on the cartilage and labrum in the dysplastic hip. Eventually these repetitive shear forces cause tearing within the labrum itself [9]. The regions of acetabular bone undercoverage correlate anatomically with the location of the labral tear. This repetitive shearing and physical overload may also explain the presence of a hypertrophied labrum in dysplastic hips [10].
As the labrum degenerates, pathologic changes can also be seen in the articular cartilage of the hip joint. Dysplastic hips may already be at a disadvantage as the quality of the cartilage differs from that of a normal hip [11]. The increased loads at the cartilage of the chondrolabral junction in conjunction with a compromised labrum will exacerbate the pathologic process. Early alterations occur at the physiologic level, with cartilage specimens showing increased content of inflammatory cytokines and catabolic enzymes. These alterations lead to cleavage of proteoglycans, decreased water content, and further loss of the mechanical integrity [11]. While abnormal morphology is the root of this physical and physiologic degeneration, it is the injury to the soft tissues that is thought to be the genesis of symptoms in many patients [12].
The process of chondrolabral degeneration is not unique to SMAD. The treating surgeon should be mindful that FAI encompasses a number of femoral and acetabular morphologies. The specific morphology of the pathologic hip will not only affect the location and pattern of chondrolabral damage but will influence the presentation of the patient and will significantly impact the treatment options available. Hip dysplasia represents a focal process generally due to undercoverage in the anterolateral acetabulum; however, unique populations such as cerebral palsy patients will present with focal posterolateral deficiencies. An aspherical femoral head, diminished femoral torsion, or acetabular retroversion may potentiate motion-induced impingement even in the setting of focal insufficient coverage and can result in motion-induced instability. While all of these pathologies lead to differing abnormal forces at the hip joint, the specific morphologic pattern determines presentation and, more importantly, their treatment. Overcorrection of dysplasia may exacerbate an unrecognized or potential impingement.
Epidemiology
The exact prevalence of SMAD is difficult to determine due to the variable nature of symptomatology, access to healthcare, and failure to recognize the problem. Returning to the root of the problem, developmental dysplasia of the hip is estimated to have an incidence of 5.5 % in neonates based on studies performed in the United States (US) [13]. Currently, physical examination screening is performed on the majority of children in the US and this allows for both prompt identification of the problem and early treatment if necessary. This broad-based screening may have decreased the prevalence of SMAD by identifying the problem during infancy. While 80 % of neonatal hip dysplasia will spontaneously resolve, those who require treatment can be confident excellent results can be achieved with the Pavlik Harness [14].
What is difficult to discern is whether a direct correlation or even progression between DDH and SMAD exists. Developmental dysplasia of the hip has been shown to be associated with predominantly female sex, breech presentation, the left hip, and a family history of DDH. Patients with SMAD have a higher proportion of males, bilateral involvement, and a family member who underwent THA before age 65 [15] (Table 2). Larger population-based studies done for FAI are now shedding more light into the prevalence of SMAD and the prevalence of both asymptomatic and symptomatic patients. The rate of SMAD based on lateral center-edge angle (LCEA) places the prevalence at somewhere between 5 % and 20 % of the population having an LCEA <25° and approximately 3–6 % having an LCEA < 20° [16].
Table 2
Comparison of developmental dysplasia and skeletally mature acetabular dysplasia
Developmental dysplasia of the hip | Skeletally mature acetabular dysplasia |
|---|---|
Female sex (98 %) | Female sex (88 %) |
Breech presentation | |
Left hip | Bilateral involvement |
Family history of DDH | Family member with THA before age 65 |
Oligohydramnios |
These studies have also shown that only a small minority of those patients with radiographic abnormalities will go on to develop symptoms. The connection of SMAD to OA is based on studies of small populations or selective cohorts. While decreased LCEA is associated with an increased risk for OA, the cutoff values used to define pathologic LCEA varies from study to study, and therefore, broad conclusions cannot be drawn. Females are thought to be at higher risk for OA than males, but this is based on limited study information [17]. Further complicating the issue is that SMAD represents only a small portion of the large variety of morphologic acetabular anomalies that have been described.
Clinical Evaluation
Clinical diagnosis of the young patient with SMAD can be a difficult task. Most patients will present with the ambiguous complaint of hip pain. “Hip pain” is a vague term that can encompass many pathologies that may or may not be associated with the hip itself. Many patients who present with hip dysplasia have often had a long-standing history of hip pain with one study showing on average 5 years from onset of pain to the time of diagnosis [18]. Most patients had seen a primary care or sports medicine physician and been diagnosed with a variety of pathologic processes. Some will also have tried physical therapy with no improvement or possibly exacerbation of their symptoms with stretching programs [19]. Thus, the surgeon who chooses to evaluate hip pain in the young patient should be fully aware of the range of clinical presentations and how they relate to both intra-articular and extra-articular pathologies.
Evaluation should begin with a thorough history of the presenting complaint. Specific details should be determined including duration of the symptoms and the history of the symptoms. Most patients will present with an insidious onset; however, some will relate it to a traumatic cause [18]. Exacerbating factors should be determined as many patients will complain of pain with activities such as running or sports, but some may notice it with activities of daily living such as getting in and out of a car, prolonged sitting, or rising from a seated position. Pain with prolonged sitting is more often seen with FAI , whereas patients with SMAD may complain of pain with prolonged standing due to chronic abductor weakness [20]. The location of the pain is also variable, but will predictably be present in the anterior groin, the lateral side of the hip, or both. Laterally based pain can be associated with abductor weakness, while groin pain in SMAD may be due to a labral tear or instability. About 75 % of patients will find their pain to be either moderate or severe, and a similar percentage will either report or present with limping when walking even short distances [18, 20]. Nunley and colleagues reported an inability to correlate specific pathology with complaints. The constellation of symptoms seen in SMAD is also seen in FAI and mild osteoarthritis , which may lead to a delay in diagnosis if a thorough evaluation is not performed [18].
The majority of patients with either FAI or SMAD will present with mechanical symptoms during activities specifically those with labral tear s [18, 20]. These mechanical symptoms may be described as snapping or popping and are generally sensations felt in the groin, not in the lateral thigh as is seen in iliotibial band (ITB) syndrome. Most will not be using walking aids. Rest is generally their most reliable method of symptom relief, and many will report having decreased or modified their activities to prevent pain [18, 20].
Thorough investigations should be performed into the patient’s medical history. Specifically, their birth history is important to identify risk factors for DDH such as breech presentation, first born, or pregnancy-related issues such as oligohydramnios. Mode of delivery can also be useful as a patient may have been born via Cesarean section but not know the inciting reason for the non-vaginal delivery. Childhood history should also be evaluated to determine if any interventions were performed such as double diapers, Pavlik harness, brace wear, or any imaging that may have been done. Finally, family history should be explored to determine if there is any history of hip problems in the family. Physicians should specifically ask about family members who may have undergone THA and the ages at which those procedures were performed. Recent evidence shows patients with SMAD are more likely to have a family member who underwent total hip arthroplasty (THA) at an age less than 65 [15].
Physical exam should begin by evaluating the patient’s gait. The presence of a Trendelenburg gait suggests abductor weakness, internal foot-progression angle may indicate increased femoral anteversion, and a limp may be due to pain or limb length equality. Limb lengths should be measured as they may indicate a possible subluxed or dislocated hip. Range of motion, typically evaluated in the supine position, should be documented and assessed for any limitation of abduction, flexion, or internal rotation. Patients with SMAD will generally have a slightly increased range of motion which may help distinguish it from FAI. Pain or clicking at the extremes of motion may be indicative of a labral tear. Patients should be evaluated for ITB tightness (Ober test) or abductor tightness which can occur in the setting of a patient with instability associated with dysplasia [21]. The patient should also be examined for a generalized ligamentous laxity.
A number of provocative maneuvers have been described to evaluate hip pain in the young patient. All patients should be palpated and asked about abdominal or inguinal tenderness to rule out a possible hernia. The anterior apprehension test is performed by having the patient extend their hip while the examiner adducts and external rotates the hip. Recreation of groin pain or guarding can be a sign of instability [21]. The anterior impingement test with flexion, adduction, and internal rotation of the hip has good positive predictive value but low sensitivity for labral tears [22]. The FABER test, with flexion, abduction, and external rotation, was initially described for the assessment of sacroiliitis; however, reproduction of groin pain has high positive predictive value for intra-articular hip pathology.
Finally, the examiner should attempt to reproduce any snapping sensation in the hip or the patient should be asked to reproduce them. Lateral snapping can be due to movement of the anterior border of the gluteus maximus or the posterior border of the tensor fascia lata (TFL) over the greater trochanter. The psoas test, by which one will flex the hip, external rotate, abduct, and then slowly extend the leg with internal rotation, may reproduce snapping associated with the psoas tendon and the iliopectineal eminence.
Radiographic Evaluation
The cornerstone of treatment of SMAD is not only the clinical diagnosis but identification of specific anatomic abnormalities. Perhaps no portion of the workup plays a greater role than imaging. Although the clinical exam can be obvious at times, accurate interpretation of proper radiographs is crucial to determine the specific morphologic abnormalities that may be present and, subsequently, the treatment options that may or may not benefit the patient. Although a patient may present with an exam and history strongly suggestive of a labral detachment, plain films should always be closely scrutinized for morphologic abnormalities, as labral tears rarely in their absence.
All imaging begins with a proper AP pelvis plain radiograph. Patient positioning and beam placement is essential to obtaining an image that has accurate rotation and tilt. Films can be taken in the supine position or the standing position with approximately 120 cm between the tube and the film distance [23]. Standing films may lead to slight extension of the hip that can effect pelvic tilt and diminish the acetabular retroversion appreciated on supine films [24–26]. Both legs should be internally rotated approximately 15° to take into consideration femoral anteversion. In males, the proper tilt is obtained when the tip of coccyx is approximately 1–3 cm above the top of the pubic symphysis. In females, up to 4 cm of space may be seen in a normal AP pelvis radiograph [23]. The film should then be inspected for proper rotation. Rotation can be assessed by the symmetry of the obturator foramen, the teardrop, and the iliac wings [27]. The tip of the coccyx should also be centered over the pubic symphysis (Fig. 3).


Fig. 3
Proper AP pelvis radiographs should have the tip of the coccyx centered of the pubic symphysis and within 2 cm. Additionally, the obturator foramen should appear symmetric
After confirming that an appropriate film has been obtained, the physician should look for obvious pathology that could result in pain such as frank osteoarthritis, fracture, or any sclerosis or bone reaction in the region of the femoral head or neck that may signal a stress fracture or other pathologic process. The femoral head should be evaluated for possible subchondral radiolucency or collapse as seen in avascular necrosis. Subluxation can be assessed using Shenton’s line. Joint space narrowing, osteophyte formation, subchondral cysts, and subchondral sclerosis should all be evaluated with respect to the Tonnis grading system for osteoarthritis of the hip.
Concurrent use of the joint space width (JSW) of ≥2 mm or <2 mm has been used to help dichotomize patients into those with Grade 0 or 1 changes and JSW >2 mm compared to a second group of patients with Grade 2 or 3 changes and JSW <2 mm [28–30]. Radiographic grading is important as the presence of Grade 2 or 3 changes have been associated with inferior outcome, following joint preservation procedures.
Next, parameters of the hip are determined to define any pathomorphologies. The lateral center-edge angle (LCEA) of Wiberg evaluates the lateral coverage of the hip. A line, which is perpendicular to the inter-teardrop line, is drawn through the center of the femoral head to the acetabulum, and a second line is drawn from the center of the femoral head to the lateral margin of the acetabulum. The angle created by this arc is the LCEA, and normal values range from 25° to 40°. Less than 20° is considered acetabular undercoverage, while greater than 40° indicates overcoverage [16] (Figs. 4 and 6).
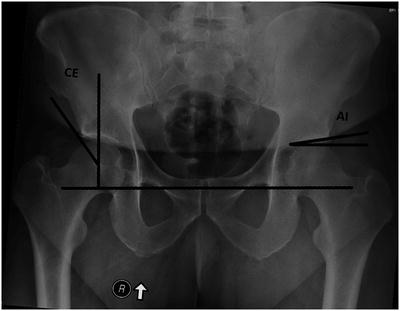
Fig. 4
This illustration shows the lateral center-edge angle of Wiberg (Reprinted with permission from Delaunay, S., RG Dussault, PA Kaplan, and BA Alford. “Radiographic Measurements of Dysplastic Adult Hips.” Skeletal Radiology 26.2 (1997): 75–81.)
Fig. 5
This illustration shows the acetabular index or tonnis angle (Reprinted with permission from Delaunay, S., RG Dussault, PA Kaplan, and BA Alford. “Radiographic Measurements of Dysplastic Adult Hips.” Skeletal Radiology 26.2 (1997): 75–81.)
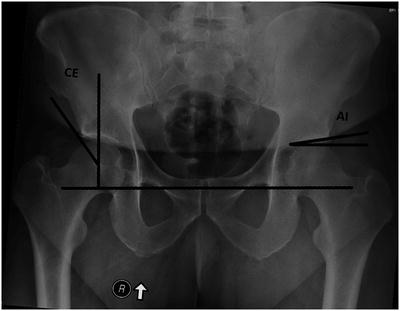
Fig. 6
A radiograph outlined with the radiographic measurements of the lateral center-edge angle and acetabular index
The acetabular index of Tonnis assesses the slope of the weight-bearing surface. A line that is parallel to the inter-teardrop line is drawn across the top of the femoral head. A second line is then drawn from the medial aspect of the sourcil to the lateral aspect of the sourcil. An angle greater than 10° is commonly associated with dysplasia (Figs. 5 and 6).
A common finding in SMAD is lateralization of the hip center due to a shallow acetabulum. The amount of hip joint lateralization should be quantified to not only compare to the contralateral hip but also as a marker for how much medialization is needed at the time of surgery. Lateralization is commonly associated with subluxation, defined by a break in Shenton’s line. The distance between the medial aspect of the femoral head and the ilioischial line is measured. A normal value is generally less than 10 mm [31].
Careful evaluation of acetabular version is important as this may indicate an isolated pathology and may be associated with posterior superior coverage deficiencies or a more classic lateral and anterior deficiency with concomitant retroversion. First the anterior acetabular rim should be evaluated in its relationship to the posterior acetabular rim. In a normal hip, the anterior rim is at all times medial to the posterior rim with both originating at the superior aspect of the acetabulum. If the anterior rim is seen to cross over the posterior rim, this is suggestive of acetabular retroversion (Fig. 7). In SMAD, the crossover is generally seen in the cranial third of the acetabulum [32]. Concurrently, the posterior wall sign must be evaluated as the normal posterior wall will intersect or be lateral to the center of the femoral head. Deficient posterior coverage is defined as the rim being medial to the center of the femoral head [33]. Another indicator of acetabular retroversion is the ischial spine sign which is demonstrated as any portion of the ischial spine projecting into the pelvic on an AP pelvis image [34]. Retroversion must be evaluated prior to undertaking surgery as failure to recognize and address its presence can lead to acetabular malposition and impingement symptoms even after acetabular redirecting surgery [35].


Fig. 7
This radiograph shows a prominent right ischial spine, crossover sign , and a large iliac wing consistent with focal acetabular retroversion
Lateral views of the hip will provide additional information on associated femoral morphologies. The 45° Dunn lateral has been shown to be the most sensitive for evaluating femoral CAM deformity [36]. The image is obtained with the patient supine, the hip flexed to 45° and abducted 20° with neutral rotation. The beam should be aimed at a point between the anterior superior iliac spine (ASIS) and the pubic symphysis [23]. Cross-table lateral images may help determine femoral torsion in addition to femoral head neck abnormalities, but commonly advanced imaging will be necessary to better define this highly variable parameter.
The false profile view is used to determine anterior acetabular coverage of the femoral head [37]. It is obtained by having the patient stand against the film with the cassette at the side of their hip. The patient then turns 25° posterior and away from the coronal plane. The radiographic beam should be centered on the femoral head (Figs. 8 and 10) [23]. Similar to the LCEA, the anterior center-edge angle (ACEA) is determined on the false profile. A value less than 20° is suggestive of deficient anterolateral coverage, while values greater than 40° indicate possible overcoverage (Figs. 9 and 10). Furthermore, a prominent anterior inferior iliac spine is profiled on this view.