Fig. 1
Greater trochanteric bursa injection. The needle is inserted perpendicular to the skin and directed at the point of maximal tenderness at the greater trochanter (GT)
Gluteus Medius Tendon Injection Technique
Position the patient in the lateral decubitus position on the unaffected side. Clean the area in the typical sterile fashion. Palpate the area of localized tenderness. Place the ultrasound probe in an oblique coronal plane using the long axis for needle advancement and medication placement. First, anesthetize the skin and subcutaneous affected area, using the ultrasound. Once the superficial area is anesthetized, slowly advance the 25-gauge needle to the lateral part of the tendon at the attachment on the greater trochanter using continuous ultrasound (Fig. 2). Position the needle tip and inject the corticosteroid solution under real-time ultrasound. Remove the needle and cover with a sterile dressing.
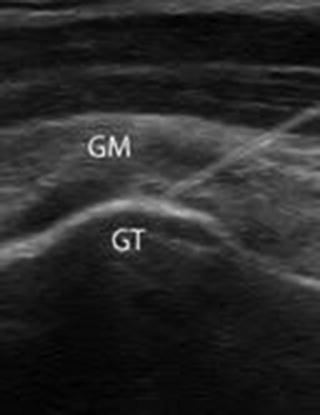
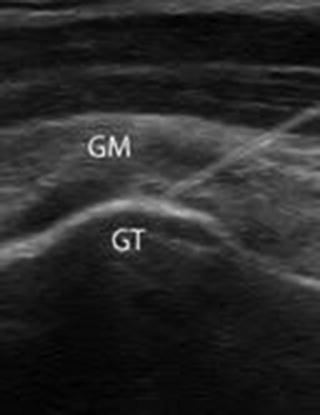
Fig. 2
Ultrasound imaging of a gluteus medius tendon injection. GM gluteus medius, GT greater trochanter
Aftercare
Avoid causative activity for 1 week and then gradually increase activity. Stretching of the iliotibial band and strengthening of the hip abductors should be encouraged. At times the addition of modalities, formal physical therapy for focused hip stretching and strengthening, NSAIDs – oral or local – and modified exercise can be helpful.
Gluteal Bursitis
Gluteal bursitis can occur as a result of acute trauma such as a direct fall onto the buttocks or repetitive overuse activities such as running. Typically, the patient will complain of pain over the upper outer quadrant of their buttock. The patient may complain of difficulty sleeping on the involved side.
Physical exam findings will reveal pain when palpating the upper outer quadrant of the affected buttock. Pain may be reproduced by passive flexion and adduction and resisted extension and abduction of the extremity.
The gluteal bursae vary in number and location and are located between the layers of the gluteal muscles and between the muscles and the surface of the ilium. When planning the placement of the injection, palpate the area and identify the location of the painful site.
Gluteal Bursa Injection Technique
Position the patient in a recumbent position on the unaffected side. Extend the lower leg and flex the upper leg. Identify and mark the tender area in the upper outer quadrant of the buttock. Cleanse the injection site in typical sterile fashion. Insert a 22- or 25-gauge needle perpendicular to the skin at the point of maximal pain until it touches the ilium (Fig. 3). Once the needle is positioned, aspirate. If no blood or paresthesias is noted, inject the contents of the syringe. There should be minimal resistance to injection flow. If paresthesias are noted during the procedure, immediately relocate the needle as it may have come into contact with the sciatic nerve. Remove the needle and place a sterile dressing over the site.


Fig. 3
Gluteal bursa injection. Positioned on the unaffected side. The needle is inserted at the point of maximal pain in the upper outer quadrant of the affected buttock
Aftercare
The patient should be instructed to observe for any signs of irregularity at the injection site. The patient should be instructed to modify activity to avoid excessive use of the lower extremities for 1 week and then gradually resume normal activities. Physical therapy may be indicated to address the etiology of the bursitis.
Iliopsoas Bursitis
The iliopsoas muscle is composed of the iliacus, psoas major, and psoas minor. The iliopsoas tendon inserts on the lesser trochanter and acts as a hip flexor. The iliopsoas bursa is positioned between the distal iliopsoas tendon and the anterior aspect of the femoral neck.
Iliopsoas bursitis and tendonitis are due to overuse and can be a source of hip and groin pain. These conditions are seen in activities that require repeated hip flexion. Runners, hurdlers, and ballet dancers are examples of athletes that may present with iliopsoas bursitis or tendonitis. Iliopsoas bursitis may occur after acute trauma, a total hip arthroplasty, or in rheumatoid arthritis patients [17, 18].
Patients likely will complain of groin pain and may note radiation of pain down the anterior thigh toward the knee. Pain is worsened by activities such as running or daily activities such as walking up stairs.
Physical examination may note tenderness in the area of the inguinal ligament. Pain may be elicited by passive hip flexion, adduction, abduction, and at times extension. Resisted hip flexion or passive hyperextension may reproduce pain. A snap may be heard or felt in the inguinal area when the hip is flexed, abducted, and externally rotated, and then the hip is extended.
Conservative treatment includes anti-inflammatories, modified activities, stretching, and physical therapy. If symptoms persist despite this management, then a corticosteroid anesthetic injection could be considered.
Iliopsoas Bursa Injection
Proper injection technique is critical since the bursa lies deep to the femoral vein, artery, and nerve. The use of ultrasound can allow for accurate placement of the injection [19].
Technique – Position the patient supine. Palpate the femoral artery. Cleanse the injection site in a typical sterile fashion. Place the ultrasound transducer in an oblique orientation that is parallel to the femoral neck. Use a lateral to medial approach and real-time ultrasound to insert a 22- or 25-gauge spinal needle at the level of the iliopectineal eminence. The bursa lies between the iliopsoas tendon and the anterior hip capsule. Confirm proper placement by real-time ultrasound as the bursa fills (Fig. 4). When injecting the solution, no resistance should be noted. If resistance is met, withdraw further until fluid flows uninhibited. Remove the needle and place a sterile dressing over the injection site.


Fig. 4
Iliopsoas bursa injection. Note the bursa is distended (Photo courtesy of John Hill, DO, University of Colorado)
Aftercare
The patient should be instructed to observe for any signs of irregularity at the injection site. Instructions should be provided to limit causative activity for a week or longer depending on symptoms.
Potential Complications
Although uncommon, anesthesia of the lateral branch of the femoral nerve may occur. If this occurs the patient will experience temporarily anesthesia of the quadriceps. Keeping the injection lateral as described above will help avoid this rare complication. Additionally, it is advisable to have the patient report immediately any symptoms of tingling or nerve sensation while performing the injection. If these symptoms are reported, reposition the needle prior to injecting the solution.
Adductor Tendonitis
The adductor muscles of the hip include the adductor longus, adductor brevis, and the adductor magnus. This tendon group originates along the pubis and ischial tuberosity and is responsible for hip adduction. The tendon group is susceptible to developing tendonitis from overuse and traumatic stretching injuries. The tendon can be injured along the proximal tendon or at the more common area at the site of the attachment at the pubic area. Tendinitis can occur with repetitive overuse activity. The adductor longus muscle is most frequently injured. This muscle is susceptible to injury with activities that require sprinting with sudden directional changes such as basketball, soccer, or hockey.
Acute injuries typically occur at the muscle-tendon junction but can occur at the bone-tendon attachment [20] (Fig. 5). A partial or full thickness tears can occur and inspection of the region may demonstrate bruising on the inner aspect of the thigh.
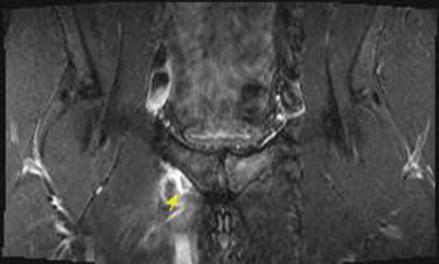
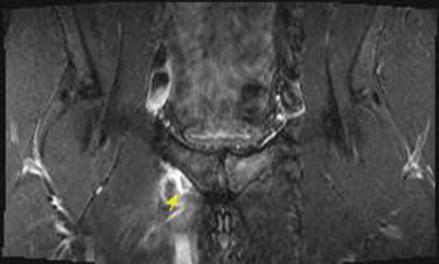
Fig. 5
Full thickness tear with retraction of the adductor longus and brevis muscle in a semiprofessional hockey player
Individuals with adductor injuries will complain of localized pain at the origins of the tendons and along the muscle with palpation. The pain can be sharp, constant, and severe. Pain is elicited with passive abduction or resisted adduction of the affected leg.
Initial treatment includes rest, ice, compression, and nonsteroidal anti-inflammatory medications [21]. Physical therapy may be helpful to assist with stretching, correct biomechanical abnormalities and functional deficits, and progress strengthening [22].
If chronic adductor pain persists despite conservative management, then a corticosteroid injection at the base of the tendon or at the site of inflammation may be considered. Schilders et al. [23] reported that a single entheseal pubic cleft injection provided short-term improvement, mean of 5 weeks, in a competitive athlete with evidence of enthesopathy on magnetic resonance imaging (MRI). They reported improved outcomes in recreational athletes even when abnormalities were found on MRI [23].
Adductor Tendon Injection Technique
Position the patient supine with the affected leg slightly abducted and externally rotated. Cleanse the area in the typical sterile fashion. Palpate the origin of the tendon. Insert the 25-guage needle directed at the pubic bone (Fig. 6). Once the needle touches the bone, pepper the solution into the area. Ultrasound or fluoroscopic guidance can be used for this procedure.


Fig. 6
Adductor tendon injection. Insert the 25-guage needle directed at the pubic bone. Once the needle touches the bone, pepper the solution into the area
Aftercare
Educate the patient on the signs and symptoms of an infection. Activity should be limited following the injection and gradually increase as tolerated as prescribed by the treating physician. A combination of stretching and strengthening exercises should be incorporated to overcome any weakness or existing muscle imbalances.
Hamstring Tendon Injuries
Hamstring injuries are common [20]. Although the muscle-tendon junction is a common site for the hamstring to tear [20, 24], proximal hamstring injuries can occur and be a source of acute or chronic pain (Fig. 7). Proximal hamstring pain can be acute in sudden tendon rupture or chronic from overuse resulting in tendinosis [25].
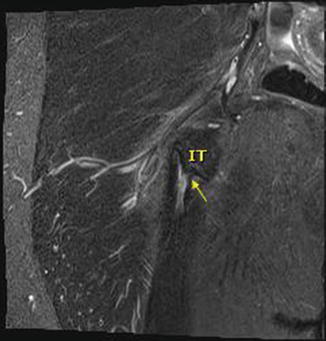
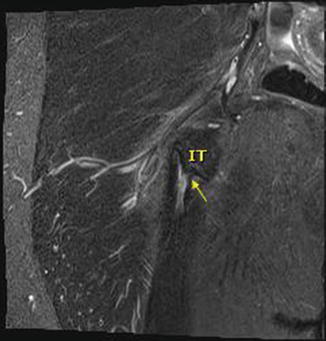
Fig. 7
Proximal hamstring tendinosis with a partial tear (arrow). Ischial tuberosity (IT)
The hamstring tendons originate on the ischial tuberosity. The conjoint tendon consisting of the biceps femoris and semitendinosus inserts posterior and inferior on the tuberosity, while the semimembranosus tendon attaches more proximal and anteriorly just medial to the sciatic nerve. Hamstring injuries can mimic sciatic-type symptoms and may coexist with sciatic nerve irritation. The ischial bursa can be found between the ischial tuberosity and the gluteus maximus and can be a source of pain.
Pain arising from the proximal hamstring tendon can occur suddenly, as in an acute eccentric strain or direct trauma, resulting in an acute rupture or incomplete tear. Chronic hamstring tendinosis is seen in overuse and repetitive activity such as running.
Patients typically present with activity-related soreness in the ischial region or inability to participate in sports secondary to pain. Sitting can become difficult especially noted with prolonged car rides or sitting for long periods. Pain is elicited on exam by palpation of the ischial tuberosity, passively stretching the hamstring, resisted flexion of the knee, or hip extension.
Treatment is nonoperative unless there is an indication for surgical treatment such as proximal hamstring avulsion fracture or failed conservative management [25–27]. Initially, treatment includes rest, ice, compression, and elevation. Physical therapy can be utilized for modalities, soft tissue mobilization, and gradual strengthening [28].
An MRI can be performed if symptoms persist despite conservative management or the clinical examination indicates a need for further evaluation of the tendon. If the MRI findings do not suggest that surgery is indicated, a corticosteroid injection can be considered [29].
Hamstring Injection Technique
Place the patient either in the prone position or on the unaffected side. Palpate and mark the affected area. Clean the area in typical sterile fashion. Using real-time ultrasound guidance in the long axis, insert the 22- or 25-gauge needle directed at an angle to the ischial tuberosity staying medial to the sciatic nerve (Fig. 8). Continue to insert the needle until the tuberosity is touched and then pepper the solution into the peritendinous-osseous region. If bursitis is suspected, deposit the solution into the bursa. If trauma preceded the pain, such as a hard fall onto the area, an aspiration of blood may be required prior to the injection of the steroid solution.
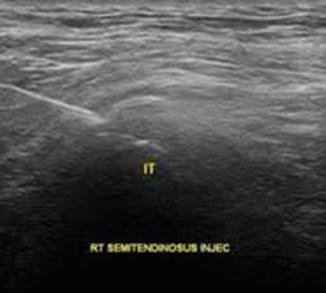
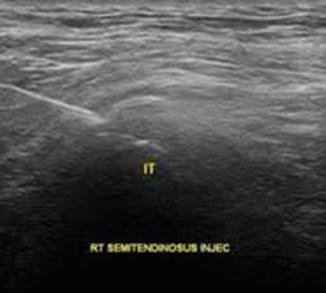
Fig. 8
Ultrasound-guided right semitendinosus injection. The needle is just superior to the ischial tuberosity (IT) (Photo courtesy of John Hill, DO, University of Colorado)
Aftercare
Educate the patient on the signs and symptoms of an infection. Avoid prolonged sitting or offending activities for at least a week. Thereafter, activity should be gradually increased as tolerated as prescribed by the treating physician.
Intra-articular Hip Conditions
Hip pain can be caused by numerous conditions including osteoarthritis, rheumatoid arthritis, labral tears, and, less commonly, collagen vascular disease, infection, and avascular necrosis and referred from the lumbar spine [30]. The most common of these diagnoses is osteoarthritis. The clinician should consider the differential and perform a diagnostic work-up based on the patient’s history and presenting symptoms. Plain radiographs can help in the diagnosis. At times further imaging with MRI or MRI arthrogram may be needed in determining the diagnosis [30].
The majority of patients with intra-articular pathology present with hip or groin pain; however, some report thigh and/or knee pain. The clinician should do a thorough evaluation of the lumbar spine, hip, and knee when determining the source of the pain.
Common complaints of patients include symptoms of stiffness and pain after inactivity such as rising from bed, prolonged standing, or walking and transitional pain such as rising after sitting for a prolonged time. Rest typically relieves the pain. If pain is related to arthritis, patients may report gradual decrease in their functional activity. Over time range of motion will be diminished and they may report difficulty crossing their legs or putting on their shoes and socks.
Physical examination findings include limited hip range of motion, pain with flexion, and internal rotation (IR). Hip abduction and extension may also elicit pain.
Plain radiographs can help determine joint space, inflammatory changes, avascular necrosis, and other deformities such as hip dysplasia and hip impingement. However, further imaging with MRI or MRI arthrogram may be indicated based on clinical history and examination.
Intra-articular Hip Injection Technique
The use of fluoroscopic guidance or ultrasound assures the placement of the medication solution in the joint.
Position the patient on his back. Position either the fluoroscope or the ultrasound probe in the proper position to visualize the joint. Cleanse the area using sterile technique. Identify the landmarks of the ASIS and the greater trochanter. Palpate the femoral artery. Insert the needle along the line directed medially at the midportion of the femoral head. Advance the needle until the bone is touched. Aspirate to confirm no blood and then inject a few milliliters of air into the hip. Confirm placement with the joint using an air arthrogram, and then inject the steroid solution (Fig. 9). Remove the needle and place a sterile dressing over the site.


Fig. 9
Right intra-articular hip injection. Air arthrogram confirms the needle is intra-articular
Aftercare
Educate the patient on the signs and symptoms of an infection. Limit activities for approximately 1 week to activities of daily living. Encourage stretching and strengthening activities. Participation in aerobic activities especially non-weight-bearing may be found to be helpful. Weight loss, when appropriate, should be encouraged.
Sacroiliac Joint Dysfunction
Sacroiliac (SI) pain has a variety of potential causes including ligamentous strain, joint hypomobility or hypermobility, degenerative arthritis, trauma, inflammatory arthritis, muscular imbalances, infection, stress or insufficiency fracture, and/or abnormal shear forces resulting in joint inflammation and pain [31]. Pregnant patients or patients with prior lumbar spinal fusion may develop SI pain that may be related to the transfer of stress to the joints. The clinical history and presentation will determine if and when additional testing is required to determine the cause (i.e., imaging and cultures). A fluoroscopy-guided injection into the SI joint that relieves the patient’s pain is considered diagnostic [32].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








