Chapter 71 Rheumatoid Arthritis of the Knee
Current Medical Management
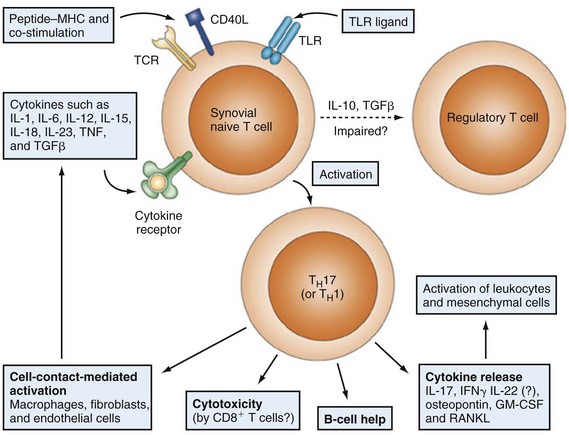
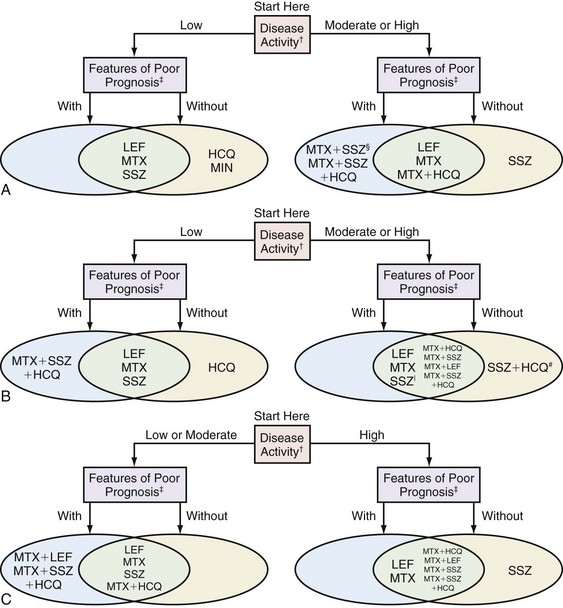
There has been substantial transformation, not without controversy, in the suggested algorithms for the treatment of rheumatoid arthritis (RA) over the past decade.4,6,23 This has been accelerated by increasing understanding of the immune pathways of the disease itself (Fig. 71-1). Most of the nonsteroidal anti-inflammatory drugs (NSAIDs) have more limited use than in the past because of their cardiovascular risks through cyclooxygenase-2 (COX-2) inhibition15 or their risk for gastrointestinal intolerance16 and, in fact, have never appreciably affected the disease process. Corticosteroids reduce symptoms and systemic manifestations of RA, but chronic use is associated with frequent side effects and also does not appreciably prevent disease progression.17 Methotrexate and other disease-modifying antirheumatic drugs (DMARDs; Fig. 71-2) usually yield no immediate relief, but over time can control symptoms and are thought to delay progression of the disease. These remain the most often used agents by rheumatologists throughout the world for the treatment of RA.1
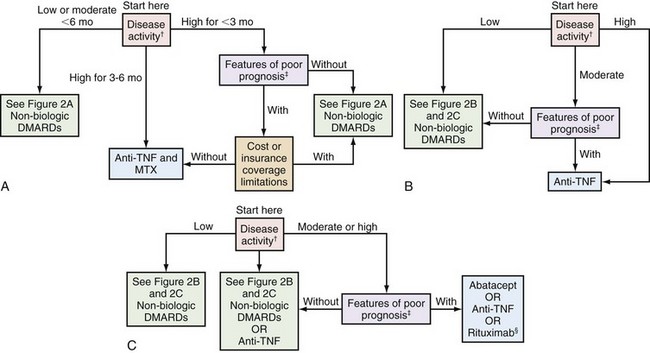
Nevertheless, recent advances by the novel biologic agents (biologics; Fig. 71-3), such as the tumor necrosis factor-alpha (TNF-α) inhibitors and anti-CD20 monoclonal antibodies, have allowed many patients with RA to experience improvement in symptoms, function, and quality of life to a degree they might not have achieved in the past. Etanercept, infliximab, adalimumab, anakinra, golimumab, certolizumab pegol, rituximab, abatacept and most recently, tocilizumab are currently U.S. Food and Drug Administration (FDA) approved for the treatment of rheumatoid arthritis. Thus, therapeutic decision making for this disease has become more complex for clinicians, with many conflicting factors playing increasingly important roles. According to the most objective measures of RA progression, very early intervention with conventional DMARDs is cost-effective whereas that of very early intervention with biologics remains unclear.13 However, more recent data indicate that biologic therapy is associated with increases in workforce participation in patients typically expected to experience progressively deteriorating ability, which could result in significant indirect cost benefits to society.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree