Chapter 87 Osteochondritis Dissecans
Osteochondritis dissecans (OCD) is an acquired, potentially reversible disorder of the subchondral bone and of the overlying articular cartilage. Initially, softening of the overlying articular cartilage is noted with an intact articular surface (Fig. 87-1), which can progress to early articular cartilage separation, partial detachment of an articular lesion, and eventual osteochondral separation with loose bodies.* Osteochondritis dissecans is a relatively common cause of knee pain and dysfunction in the child and adolescent. The cause of OCD is unknown; however, repetitive microtrauma is often implicated.13,17,30,58,74 OCD of the knee is subcategorized into a juvenile form and an adult form, depending on the status of the distal femoral physis, and is classified on the basis of anatomic location, surgical appearance, scintigraphic findings, and age.† Juvenile OCD (JOCD) has a much better prognosis than adult OCD, with more than 50% of cases demonstrating healing within 6 to 18 months from nonoperative treatment.15,31,34,66,70 Adult OCD, on the other hand, frequently requires operative intervention for healing.6,15 Adult OCD and juvenile OCD lesions that do not heal have the potential for later sequelae, including osteoarthritis.48,69

Figure 87-1 Probe demonstrates softening of a femoral condyle osteochondritis dissecans (OCD) lesion.
History and Causes of JOCD and OCD
Several factors have been implicated in the origin of OCD: inflammation, genetics, ischemia, accessory centers of ossification, and repetitive trauma. In 1887, König suggested an inflammatory origin, using the name “osteochondritis dissecans.”44 Further study, however, did not support inflammation as a primary cause of OCD. Ribbing ascribed OCD to an ossification abnormality of the distal femoral epiphysis in 1955.64 Although abnormalities in ossification do not account for most cases of OCD, some incidentally found lateral femoral condylar lesions in younger children that resolve spontaneously may represent an ossification variant. Based on their anatomic and histologic findings, Green and Banks31 proposed that ischemia was implicated in OCD, although additional studies have failed to find avascular necrosis of the OCD fragment or a relative ischemic watershed of the lateral aspect of the medial femoral condyle.16,40,62,65 Some investigators have suggested a genetic predisposition to OCD. Petrie60 found OCD in only one of 86 first-degree relatives, although as many as 12 instances of family members with OCD over the course of four generations have been reported by Mubarak and Carroll.54 It is widely believed that the common form of OCD is not familial. Endocrinopathies, ligamentous laxity, malalignment, apophysitis, epiphyseal dysplasia, and other osteochondropathies have not been described in association with OCD.
In 1933, Fairbanks24 suggested that OCD might be due to a “violent rotation inwards of the tibia, driving the tibial spine against the inner condyle.” Although anterior tibial spine impingement may not be the cause of lesions in the most common location of the posterolateral aspect of the medial femoral condyle, the frequent occurrence of OCD in patients who are involved in sports with repetitive impact supports a repetitive trauma etiology.25 OCD may begin after repetitive trauma causes a stress reaction, which then may further progress to a stress fracture of the underlying subchondral bone. Without a reduction in repetitive loading, the ability of the subchondral bone to heal is exceeded, necrosis of the fragment occurs, and eventual fragment dissection and separation develop.
OCD lesions may resemble acute osteochondral fracture, chondral injury, or osteonecrosis. The estimated incidence of OCD ranges from 15 to 29 cases per 100,000.35,47 The mean age of patients with OCD appears to be decreasing, and more girls seem to have involvement.13 The widespread use of magnetic resonance imaging (MRI) and arthroscopy in the pediatric population has likely resulted in greater recognition of OCD lesions. Trends in youth sports such as loss of free play, early sport specialization, multiple leagues in a single sport, and intensive training may be contributing factors.
Diagnosis
Clinical Presentation
Physical examination findings are often subtle. Children and adolescents with stable OCD lesions may walk with a slight antalgic gait. With careful palpation through varying amounts of knee flexion, a point of maximum tenderness can often be located over the anterior medial aspect of the knee. The tender area will correspond to the lesion, usually on the lateral aspect of the distal medial femoral condyle. With stable lesions, knee effusion, crepitus, and extreme pain are rarely observed through a normal range of motion. Wilson’s sign may be helpful but often is not present.18,76 Wilson’s test is performed by starting with the knee flexed to 90 degrees. The tibia is then internally rotated as the knee is extended from 90 degrees toward full extension. A positive Wilson’s test will elicit pain at about 30 degrees of knee flexion located over the anterior aspect of the medial femoral condyle. This pain is thought to result from contact of the medial tibial eminence with the OCD lesion. Ipsilateral quadriceps atrophy may be noted if the patient has been having pain for longer than a few months.
Imaging Studies
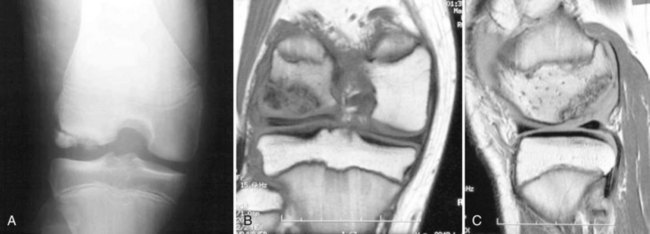
Imaging protocols have received close attention in the literature because of the varied success of nonoperative treatment. The goals of imaging are to characterize the lesion, determine the prognosis of nonoperative management, and monitor healing of the lesion (Fig. 87-2A through C).
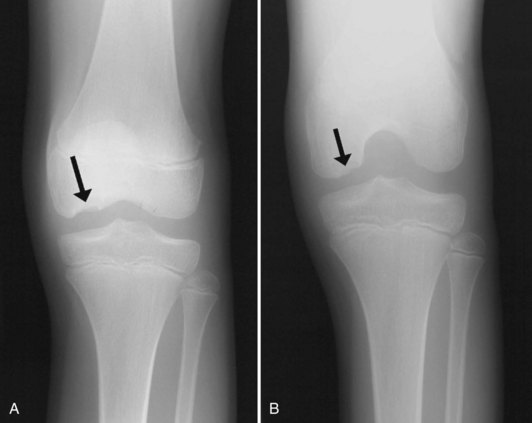
Imaging workup begins with plain radiographs: anteroposterior (Fig. 87-3A), lateral, and tunnel views. The tunnel view is particularly valuable because the typical OCD lesion is located on the lateral portion of the medial femoral condyle (see Fig. 87-3B). Because patellar OCD lesions also occur, a Merchant or skyline view should be included as well. Plain radiographs usually characterize and localize the lesion and rule out other bony pathology of the knee region. In children 6 and younger, the distal femoral epiphyseal ossification center may exhibit irregularities that simulate the appearance of an OCD. In older children, the status of the physis (open, closing, or closed) should be assessed, as this has major implications in the prognosis for healing. Cahill and Berg14 developed a classification system based on lesion location and size, such that the type of lesion can be determined on plain films.
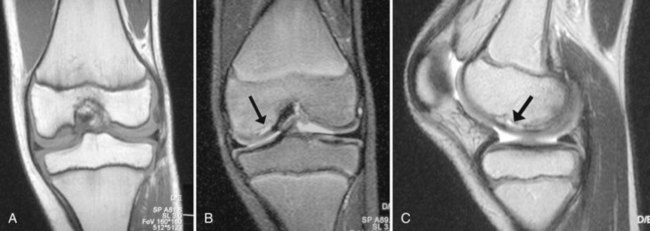
MRI is most useful for determining the size of the lesion and the status of the cartilage in the subchondral bone.41,73 The extent of bony edema, the presence of a high signal zone beneath the fragment (Fig. 87-4A through C), and the presence of other loose bodies are important findings on the initial MRI (Table 87-1). Routine imaging studies performed during the course of nonoperative treatment in skeletally immature patients can help identify patients at risk for treatment failure. Evidence suggests that a high signal line on T2-weighted images, representing healing vascular granulation tissue or articular fluid beneath the subchondral bone, is a predictor of instability.11,20,56,61 A breach in the cartilage seen on T1-weighted MRI may help predict treatment failure, particularly when seen in conjunction with a high signal line on T2-weighted images.56 Recent investigations of the relationship between gadolinium enhancement and healing have been inconclusive.11,45,72 The healing potential of stable JOCD was studied recently, and it was found that after 6 months of nonoperative treatment, 16 (34%) of 47 stable lesions did not progress to healing. The size of the lesion determined by MRI was the strongest prognostic variable.75
Table 87-1 MRI Classification of Juvenile Osteochondritis Dissecans
| Stage | MRI Finding |
|---|---|
| I | Small change of signal without clear margins of fragment |
| II | Osteochondral fragment with clear margins, but |
| without fluid between fragment and underlying bone | |
| III | Fluid visible partially between fragment and underlying bone |
| IV | Fluid completely surrounding the fragment, but the fragment is still in situ |
| V | Fragment completely detached and displaced (loose body) |
Data from Hefti F, Berguiristain J, Krauspe R, et al: Osteochondritis dissecans: a multicenter study of the European Pediatric Orthopedic Society. J Pediatr Orthop 8B:231–245, 1999.
Technetium bone scans have been used to obtain information about the biologic capacity of an OCD lesion to heal (Table 87-2).14,48,57 Although some authors have found that serial bone scans indicate the extent of healing, this imaging technique has not been widely accepted, most likely because of the length of the test, the need for intravenous access, and the perceived risk of the radiotracer injection.
Table 87-2 Bone Scan Classification of Juvenile Osteochondritis Dissecans Lesions
| Stage | Bone Scan Finding |
|---|---|
| 0 | Normal radiographic and scintigraphic appearance |
| I | Lesion visible on plain radiographs, but bone scan reveals normal findings |
| II | Bone scan reveals increased uptake in the area of the lesion |
| III | Increased isotopic uptake in the entire femoral condyle |
| IV | Uptake in the tibial plateau opposite the lesion |
Data from Cahill BR: Osteochondritis dissecans of the knee: treatment of juvenile and adult forms. J Am Acad Orthop Surg 3:237–247, 1995.
Nonoperative Management
Nonoperative management is the treatment of choice for skeletally immature children.70 Because of the vague origin of OCD, debate is ongoing about whether immobilization or bracing is therapeutic or detrimental. Because a primary goal is regeneration of injured subchondral bone, casting or knee bracing is favored by many to provide immobilization or to help unload an affected area. Other clinicians have sought to reach the same goals by using algorithms that include lesser forms of intervention such as restriction from high-impact sports; others have used partial weight-bearing or non–weight-bearing treatments. The common denominator in all programs is a structured therapy regimen to ensure the return of appropriate strength and flexibility.
Options for immobilization include casting, bracing, and standard knee immobilization. Partial weight bearing in slight flexion minimizes shear, while preserving a limited amount of compression across the lesion. Selecting an immobilization protocol can be difficult. Casts present children with the inconvenience of more restricted range of motion, but can be useful in children who are noncompliant with bracing. Recent data have shown that casts are efficacious for healing and allow maintenance of motion and strength during treatment.71
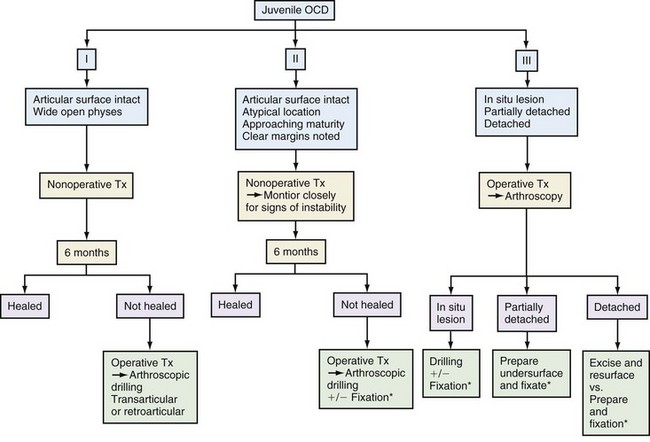
Although immobilization is often successful in JOCD, it may not be the ideal treatment option for a young athlete and his or her parents. Patients and their parents should be informed of the risks and benefits of nonoperative treatment relative to those presented by surgical management (Fig. 87-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree