Revision Anatomic Anterior Cruciate Ligament Surgery
Todd M. Swenson
Darren L. Johnson
Over the past 3 decades, the incidence of anterior cruciate ligament (ACL) reconstruction has increased to a significant degree. This increase has likely occurred for a variety of reasons: an enlarging population base participating in competitive and recreational sporting activities; the explosive increase in the numbers of female athletes participating in ACL-dependent, high-velocity sports; improved means of diagnostic assessment and increased awareness on behalf of physicians; amplified exposure of orthopaedic surgeons, during their training and thereafter, to the surgical management of the ACL-deficient knee; and heightened knowledge and expectations from the ACL injured patient/athlete in our information-age society.
Performing ACL reconstructive surgery has become a very common component of many orthopaedic surgeons’ practices (1). Incident to a larger number of primary ACL reconstructions being performed on an annual basis is an increasing need for revision procedures to address those reconstructions where failure has occurred. At present, we see this trend continuing and therefore anticipate that the number of revision ACL procedures will continue to rise.
A renewed appreciation, understanding, and study of native ACL bony insertion site anatomy and kinematic function have been rekindled in recent years (2, 3, 4, 5, 6, 7); from this has grown the concept of “anatomic ACL surgery.” Concerns exist that the popular transtibial arthroscopic technique will frequently not allow for complete anatomic placement of the femoral tunnel, often resulting in a vertically oriented ACL graft (8,9). When utilizing the transtibial technique, the placement and positioning of the femoral tunnel is limited and dictated by the position of the tibial tunnel; a nonanatomic location of the femoral tunnel will commonly result. This has led the authors and a growing number of other surgeons to modify their technique for primary ACL reconstruction. As an alternative to the transtibial technique, a variety of methods exist for creation of bone tunnels that match the native ACL femoral origin and tibial bony insertions; the use of these techniques can be employed during an anatomic single-bundle or double-bundle ACL reconstruction, depending upon surgeon preference and patientspecific anatomy. We carry these same principles forth in our approach to revision ACL surgery. Our goal is to provide the patient the means by which we may most effectively eliminate pathologic ligament laxity and restore anterior translational as well as rotatory stability with normal Kinematics; in our opinion, we feel this is best accomplished via a double-bundle anatomic ACL reconstruction. The procedure involves placement of two distinct and separate grafts representing the anteromedial (AM) and posterolateral (PL) components of the native ACL. Femoral tunnels are not drilled via the tibial tunnel, and greater flexibility exists to accommodate for patient-specific anatomy. Independent tensioning and fixation of the two grafts is performed in an attempt to maximally replicate the normal contribution each functional bundle has to knee stability throughout the arc of knee flexion.
Having familiarity with a variety of techniques for creation of bone tunnels and graft fixation as well as comfort working with several graft materials and configurations are important surgeon attributes for those performing revision ACL surgery. The ultimate function and success of a reconstructed ACL is dependent upon a combination of mechanical and biologic factors. Optimal interplay between a technically sound surgical procedure, a proper healing response, and a well-constructed rehabilitation process is needed in order to realize the best potential outcome. The goal of a primary ACL reconstruction is to replicate the anatomic position and kinematic function of the native ACL as closely as possible so as to allow the patient to return to their preinjury
state of comfort and function; these same goals, although proven more difficult to attain, are also sought in the revision setting.
state of comfort and function; these same goals, although proven more difficult to attain, are also sought in the revision setting.
The major focus of this chapter will center on the revision procedure performed for the patient who presents with recurrent instability after a failed previous ACL reconstruction; we will present and outline the details of our “optimal” revision technique. When appropriate, treatment of concomitant limb malalignment, acquired loss of motion, early degenerative changes, or compromise of secondary stabilizing constraints will serve to allow the most favorable outcome following the revision ACL procedure. Thorough discussion of the details surrounding the means by which each of these associated conditions would also be addressed, although important and not to be neglected is beyond the scope of this chapter.
INDICATIONS/CONTRAINDICATIONS
Surgical “failure” following an ACL reconstruction may be defined as loss of knee motion, persistent pain, dysfunction of the extensor mechanism, residual laxity (anterior translation and/or rotatory), recurrent functional instability, or a combination of factors. The true incidence of “failure” or “success” following reconstruction of the ACL is impossible to ascertain given the lack of broad-based acceptance regarding how each is defined. In high-demand athletes who perform at maximal performance levels, their subjective evaluation of their postsurgical knee may not match your objective evaluation. With respect to postsurgical ligament laxity and functional status, many objective measurements of our surgical results appear to inaccurately reflect patients’ satisfaction and functional stability following reconstruction of their ACL (10,11). The presence or the absence of a pivot shift appears to be a better measure of functional stability than instrumented knee laxity (i.e., KT-1000 arthrometer) or Lachman examination and has a strong correlation with patients’ perception of satisfaction, stability, and outcome (10, 11, 12).
From a structural standpoint, recurrent instability can lead to an overburdening and compromise of the secondary static restraints of the knee. Damage to the menisci, chondral surfaces, and possible progressive degenerative changes may also occur. Functionally, the patient may be unable to resume desired recreational or competitive sports participation and, at times, have difficulty with certain aspects of normal daily activities. Determining the nature and extent of the patient’s presenting disability will allow an appropriate approach for treatment to be formulated and a realistic discussion of anticipated outcomes and expectations to follow.
Graft failure resulting in persistent increased knee laxity and/or recurrent functional instability may occur on the basis of technical, biological, or mechanical factors; a combination of etiologies is not atypical (13). Recognizing the possible cause(s) of graft failure is helpful prior to proceeding with a revision ACL reconstruction if the repetition of preventable errors is to be avoided. In our revision experience, errors in prior surgical technique are often the most common identifiable cause found contributing to failure of the previous surgical procedure. A nonanatomic, malpositioned femoral tunnel represents the technical error we most frequently encounter (followed by a posterior tibial tunnel); these tunnels are often vertical and/or excessively anterior in position.
Graft failures can be seen in the presence of prior well-positioned bone tunnels; this has not been a common occurrence in our revision experience. A traumatic event is often described and may represent the sole cause for graft failure; however, the astute clinician must seek other potential causative factors before ascribing “trauma” as the single explanation for loss of graft integrity, particularly when the failure presents <1 year from the index reconstruction. In patients found fitting this particular scenario, one should consider the following as possible contributing etiologies: overly aggressive rehabilitation protocol and/or a too early return to ACL-dependent activities, patient noncompliance, failure of graft fixation, or failure of graft incorporation. Even an optimally performed ACL reconstruction followed by appropriate patient compliance and rehabilitation may fail secondary to a lack of an adequate biologic healing response to the surgery; fortunately, this is not frequently seen. Traumatic failure should only be considered after verification of anatomic graft placement and the patient had truly returned to Level 1 sports at the same level before their primary ACL injury event.
Addressing all ACL revision cases through a single, regimented surgical technique will neither be possible nor necessarily appropriate. When technically feasible, the authors plan for the use of an anatomic, double-bundle ACL reconstruction for our revision ACL procedures. Independently tensioned grafts with abundant collagen tissue within the knee for control of both anterior translation and rotatory stability are sought. At times, patient-specific anatomy will not permit for a double-bundle reconstruction and an anatomic single-bundle technique is performed instead; this occurs infrequently and is not our preference except as mandated by anatomic or technical constraints.
Although this chapter outlines our thought processes with respect to approaching revision ACL surgery, these are simply concepts with accompanying technical suggestions. No single “recipe” will suffice for each patient as each revision procedure is truly unique and presents its own particular technical challenges. An ability to adapt one’s technique to the patient’s anatomy rather than taking a “rigid” approach of making the technique fit the patient is our recommendation.
PREOPERATIVE PREPARATION
A thoughtful and thorough preoperative assessment precedes and directs development of an appropriate surgical plan; both are imperative for achieving a successful outcome. A detailed history, physical examination, and radiographic evaluation are the essential components of the preoperative assessment. The patient is interviewed and a comprehensive history is obtained. It is of critical importance to ascertain the patient’s primary presenting complaint. Limited range of motion or pain, even when found in association with abnormal ligament laxity, is not likely to be resolved through revision reconstruction alone.
Details surrounding any recent acute injury as well as symptoms and functional status of the knee since the time of the index reconstructive procedure are sought. The greater length of time that has transpired since recurrent instability began increases the likelihood of compromise to the secondary static restraints of the knee (posterior horn medial meniscus, collateral ligaments, PL complex). Any documentation from the prior surgery (i.e., operative report, arthroscopic pictures) that can be attained may be extremely useful. Information regarding the type of graft tissue that was used, nature and type of graft fixation utilized, associated procedures performed, and the status of the menisci and articular surfaces can be of significant assistance to the current assessment of the patient and subsequent planning of the revision procedure, as well as expectations the surgeon and patient can discuss.
Physical Examination
The patient is first evaluated in the standing position. Limb alignment and any asymmetry relative to the contralateral extremity are noted. Alterations in normal gait mechanics are sought, with the presence of a bent-knee gait or varus thrust being of particular concern. The location of prior surgical incisions, the condition of the skin, and the presence of any muscle atrophy are carefully assessed and documented. An examination of the neurovascular status of the limb is also completed.
With the limb in a resting, supported position, an evaluation for the presence of an effusion is performed. If an effusion is present, an arthrocentesis showing a hemarthrosis will indicate a new structural injury has likely occurred. If loss of motion is also present as a “new” problem for their usual laxity, one must be concerned about the presence of a large bucket-handle meniscal injury. Synovial fluid without bloody characteristics can be submitted for analysis including cell count and culture. Knee range of motion is assessed and compared to the opposite extremity. The prone position for assessing both passive extension and active and passive knee flexion is the most accurate means by which to document loss of motion relative to the opposite extremity. Loss of motion may be secondary to pain and swelling related to a recent acute event or may be more chronic in nature. When diminished range of motion is related to a recent traumatic event, a period of physical therapy followed by a repeat physical examination is warranted before a more definitive assessment of the knee and subsequent treatment plan are formulated.
Long-standing loss of knee motion can occur secondary to several possible etiologies; these include swelling in or about the joint, reflex sympathetic dystrophy, infection, arthrofibrosis, the presence of a mechanical block (i.e., Cyclops lesion, graft impingement, displaced meniscal tear), or capturing of the knee related to nonanatomic tunnel positions. In the presence of residual diminished motion resulting from a prior operative procedure, particularly lack of full extension, a treatment protocol (surgical and/or nonsurgical) aimed at restoring knee motion takes precedence over performing a revision ACL reconstruction. The revision procedure can be entertained after a functional range of motion has been reestablished.
To evaluate the nature of the abnormal laxity pattern found as a result of an incompetent ACL, the amount of anterior translation (Lachman test) and anterolateral rotatory instability (pivot-shift test) is documented. The ability to elicit a pivot shift in the office and grade its magnitude is inconsistent and variable, depending upon on a multitude of factors. Careful assessment for combined instabilities is sought through critical evaluation of the collateral ligaments (varus/valgus stress at 30 and 90 degrees of flexion) and PL/posteromedial structures (dial test at 30 and 90 degree flexion, PL drawer test, PL external rotation test, Slocum test).
Imaging Studies
Radiographic evaluation begins with standing full-length anterior-posterior (AP), 45-degree flexed weight-bearing posterior-anterior, lateral, and patellar view (i.e., Merchant, sunrise, infrapatellar) roentgenograms. Important information can be gleaned from these films including limb and patellar alignment, the size and location of prior bone tunnels, nature and location of associated graft fixation devices, geometry of the intercondylar notch, and the presence or absence of degenerative changes. If limb malalignment exists, correction via an osteotomy may be necessary, depending upon the clinical scenario. The combination of osteotomy and ACL reconstruction can be carried out as a two-stage procedure, with the osteotomy being done prior to the ligament reconstruction. If the two procedures are accomplished simultaneously, the osteotomy should be completed initially followed by creation of bone tunnels, graft passage, and finally, graft tensioning and fixation. If osteotomy is done, decreasing the slope of the tibia is done concurrently to aid in decreasing anterior pathology translations.
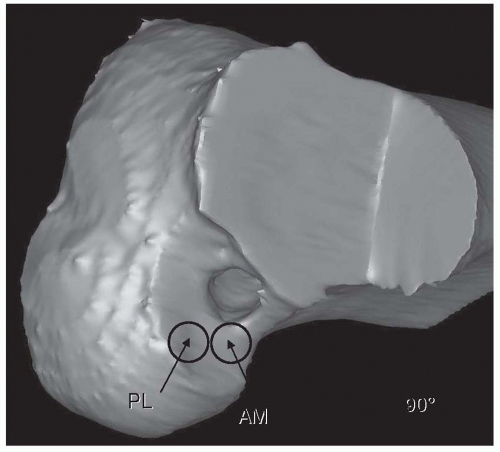
Computed tomography (CT) or three-dimensional CT scans (Fig. 32.1) can be extremely helpful in supplying a more detailed and accurate assessment of prior bone tunnel locations as well as the extent of any tunnel expansion or osteolysis that may be present. Magnetic resonance imaging (MRI) will provide abundant details regarding the integrity of the prior ACL graft, any injury or abnormality of the secondary supporting structures as well as the status of the menisci and articular cartilage; this information can assist the surgeon in planning for any additional procedures that may be performed in conjunction with the revision ACL reconstruction.
SURGERY
Performing a revision ACL surgery necessitates availability of all instrumentation typically utilized by the surgeon for a primary reconstruction. In addition, equipment that may be needed for removal of prior hardware, graft fixation, and possible alternative options for femoral tunnel creation should be present. Hardware removal may or may not be necessary, depending upon the position of the prior femoral and tibial tunnels. We recommend leaving previous hardware in place if it does not impede or obstruct creation of the revision bone tunnels in their desired locations. If removal of a prior fixation device is necessary, it may be accomplished with ease or at times, with great difficulty and significant bone loss. Having a variety of instruments on hand to assist with this task can be of enormous benefit; this should include osteotomes, curettes, trephines, end cutting reamers, and a universal screwdriver system. If “bioabsorbable” material was used for fixation during the prior ACL reconstruction, it does not preclude the possibility of encountering similar potential difficulties to those found in the presence of metal fixation devices. These materials often remain wholly or partially intact and may require removal depending upon their location. At times, these devices have begun to degrade and the process creates bone voids in their place; this may or may not have been appreciated on the presurgical radiographic assessment. We have found this to be problematic because of the poor bone quality around these “biodegradable” implants. The surgeon should be aware of this possibility and its potential implications.
When feasible, secondary incisions required for harvesting graft tissue, creation of bone tunnels, or to perform additional complementary procedures should be accomplished through the utilization or extension of prior skin incisions. When this is not possible, the surgeon should attempt to make any new incisions parallel to the previous incisions and with maximal skin bridges to minimize potential compromise of the vascular supply to the intervening skin.
Examination Under Anesthesia
A general anesthesia is used for all procedures. Preoperative intravenous antibiotics are administered. A padded pneumatic tourniquet is placed about the proximal thigh of the operative extremity. An examination under anesthesia is performed and always compared to the “normal” knee. Range of motion and laxity patterns of the operative and nonoperative extremities are assessed and compared. In the anesthetized state, void of muscular control, grading of ligament laxity, and the quality of endpoints may be different, and frequently underestimated, relative to that which was found during examination in the office setting. If the presence of concomitant ligamentous laxity is not recognized and properly addressed, repeat failure of the reconstructed ACL will likely result. When a combined pattern of ligamentous laxity is identified, options include: (a) staging the surgical procedure, with the secondary restraints addressed initially followed by a later reconstruction of the ACL; or (b) attending to all pathologic laxity through simultaneous surgical correction.
Patient Positioning
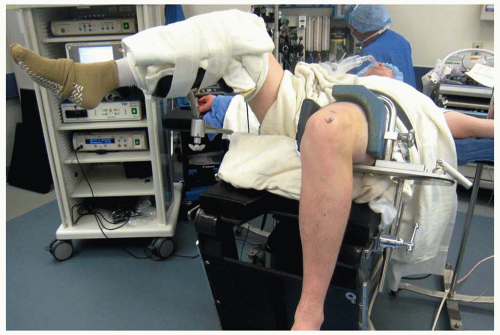
A successful surgical procedure begins with proper patient positioning. An arthroscopic leg holder is placed upon the proximal thigh of the operative extremity and secured to the surgical table at the break point of the bed. This leg holder is then positioned such that it is slightly elevated from the surgical table and angled toward the patient’s head, placing the hip of the operative extremity between 30 and 45 degrees of flexion. The foot of the bed is then removed or maximally flexed. This combination of details for surgical limb positioning is necessary to allow for maximal hyperflexion of the knee, a position that is required during the method of medial portal drilling for creation of the femoral tunnels (Fig. 32.2). The nonoperative extremity is placed in a lithotomy-type position with the leg resting upon a well-padded support in a position of hip and knee flexion (each ˜90 degrees) in addition to hip abduction and external rotation (Fig. 32.3). This position allows the surgeon or an assistant unobstructed access to the medial aspect of the operative extremity should any accessory procedures (i.e., inside-out meniscal repair, MCL/posteromedial capsular plication) be necessary.
Arthroscopy
Following sterile preparation and draping of the operative extremity, the surgical procedure is initiated. We attempt to perform as much of the arthroscopic procedure as is as possible without inflation of the tourniquet. Monitoring and control of the patient’s blood pressure and use of an arthroscopic electrocautery device are beneficial in maintaining a clear field of visualization.
The importance of appropriately placed arthroscopic portals cannot be overemphasized. Poorly positioned portals may obscure adequate visualization and compromise the use of instrumentation during the procedure. We routinely utilize three anterior portals for visualization and instrumentation during all ACL reconstructions (14). These portals are each created with an 11-blade with the knee in a 90-degree flexed position. Depending upon surgeon preference, an additional superior-medial or superior-lateral portal for either inflow or outflow may also be employed. The anterolateral portal, familiar to all arthroscopists, is used solely for visualization during an ACL reconstruction. We place this portal tight to the lateral border of the patellar tendon, just beneath the inferior pole of the patella; this position will typically avoid penetration of the infrapatellar fat pad and
provides excellent access to all three compartments of the knee during diagnostic assessment. This portal also permits the surgeon to look down upon the anatomic location of the ACL tibial insertion, an important view during creation of the tibial tunnel(s). Making this portal to low will not allow one to see the entire ACL tibial footprint in the AP direction.
provides excellent access to all three compartments of the knee during diagnostic assessment. This portal also permits the surgeon to look down upon the anatomic location of the ACL tibial insertion, an important view during creation of the tibial tunnel(s). Making this portal to low will not allow one to see the entire ACL tibial footprint in the AP direction.
 FIGURE 32.2 Arthroscopic leg holder positioned on the operative extremity to allow for maximal knee hyperflexion. |
The central medial portal is established with the assistance of spinal needle localization. The position of this portal is immediately adjacent to the medial border of the patellar tendon and above the medial meniscus directly in line with the ACL tibial footprint. Debridement of a portion of the infrapatellar fat pad may be necessary to improve the ease of using instrumentation entering through this portal. When visualizing through the central medial portal, the surgeon is provided an unobstructed view of the entire lateral intercondylar wall and posterior aspect of the notch. Visualization of the posterior portion of the lateral intercondylar wall and adjacent over-the-top position can be difficult and less than optimal while viewing only through the anterolateral arthroscopic portal. The central medial portal serves as both a working portal and a viewing portal at points during the revision ACL procedure.
The third anterior portal is the accessory AM portal; its location is more medial and slightly inferior relative to the adjacent central medial portal (Fig. 32.4). This portal is created under direct visualization with the arthroscope in the anterolateral portal and viewing in a medial direction. A spinal needle is placed just above the medial meniscus with a superior and laterally directed trajectory; the needle will pass just in front of the medial femoral condyle (Fig. 32.5). This portal will be utilized for drilling of the femoral bone tunnels. The location of this portal is critical; before creating the skin incision, the spinal needle position is adjusted in anticipation of allowing passage of an appropriate diameter single fluted annulated reamer to the lateral intercondylar wall without causing iatrogenic damage to the articular cartilage of the medial femoral condyle.
Following creation of the standard arthroscopic portals, a systematic diagnostic assessment of the entire intra-articular aspect knee is undertaken. Any identified chondral or meniscal abnormalities are addressed accordingly. Attention is then focused upon the revision ACL reconstruction. All remaining previous graft material is carefully resected. Identifying and visualizing the over-the-top position in the posterior aspect of the notch is critical. The intra-articular locations of the prior bone tunnels and the fixation hardware are sought (Fig. 32.6). We recommend that a nonaggressive, methodical debridement be performed so as to minimize bone




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree