Proximal Biceps Injury—Open Versus Arthroscopic Tenodesis
James R. Romanowski
Mark W. Rodosky
INDICATIONS/CONTRAINDICATIONS
Despite the minor contributions to shoulder stability and function, the long head of the biceps tendon (LHBT) may contribute to significant shoulder pain and disability (7). Rarely does primary biceps pathology occur independently, with 95% of biceps tendinitis, tears, and degeneration related to secondary causes (6). The long head of the biceps tendon is torn in 5% of all shoulder arthroscopies, most commonly associated with rotator cuff tears (75%) and anterior instability (7.5%) (4). Synovitis resistant to conservative treatment evolves into fraying with cellular infiltration and fibrosis as part of the degenerative process (2). The anatomic constrictions of the bicipital tunnel provide little room for tendinitis and adhesions, with pain typically the end result.
Both primary and secondary biceps tendinitis are initially treated with rest, activity modifications, and anti-inflammatory medications. Steroid injections into the bicipital sheath may be helpful; however, the risk of iatrogenic damage to the tendon precludes this modality and should be performed only by experienced physicians or with ultrasound guidance. Given the high association of concomitant shoulder pathology, physical therapy modalities should focus on the rotator cuff, labrum, instability, and impingement as indicated.
Failure of conservative therapeutic modalities is an indication for operative intervention of biceps-related dysfunction. Arthroscopy allows for global assessment of the glenohumeral joint, including the LHBT. Age, activity, and degree of LHBT damage are considerations for performing débridement, tenotomy, or tenodesis. Débridement may remove synovitis and partial tearing; however, the possibility for progressive
LHBT degeneration exists and should be reserved for only the most minor of biceps damage. A tenotomy of the tendon is recommended for tears in older, sedentary patients who accept the potential cosmetic “Popeye” deformity. Cramping and fatigue of the biceps brachii may result, but is rarely reported in individuals >60 years old (5).
LHBT degeneration exists and should be reserved for only the most minor of biceps damage. A tenotomy of the tendon is recommended for tears in older, sedentary patients who accept the potential cosmetic “Popeye” deformity. Cramping and fatigue of the biceps brachii may result, but is rarely reported in individuals >60 years old (5).
Tenodesis is an attractive option because the anatomy is relatively preserved while removing the diseased segment. The length, tension, and cosmesis of the biceps brachii are maintained with minimal loss of strength and shoulder function. The disadvantages are the increased complexity of the intervention and longer postoperative immobility and rehabilitation. Surgical candidates include all patients with >25% biceps tears, particularly in younger, active individuals. In cases of LHBT instability, subluxation, and dislocation, tenodesis is recommended given the poor results of reflection pulley reconstruction.
Contraindications for biceps tenodesis include medical instability, active infection, or in patients with true pseudoparalysis of the shoulder with rotator cuff tears.
PREOPERATIVE PLANNING
Patient Evaluation
Critical to the evaluation and preoperative planning of patients with suspected LHBT dysfunction is a thorough history and physical examination. The association of multiple concomitant shoulder issues makes isolated biceps disease an exception rather than the norm. Identification of all the pathology is necessary for the patient to make an informed decision about surgical intervention and to allow the surgeon to maximize patient outcome by addressing all the potential pain and dysfunction generators.
Patients often complain of anterior shoulder pain that is focused over the proximal humerus. Pain with overhead activities is common, however nonspecific as compression at the coracoacromial arch affects multiple shoulder structures. Pain related to the LHBT may be referred distal to the shoulder into the anterior arm. Occasionally with chronic cases, and rarely in the acute traumatic cases, the patient may complain of a “Popeye” deformity related to a complete tear and retraction of the LHBT.
Physical examination begins with inspection and visualization of both shoulders. Biceps specific maneuvers include Speed, Yergason, and Biceps Instability tests, but none have a particularly high sensitivity or specificity. Direct palpation of the bicipital groove often will illicit pain and is a more sensitive test (4). A complete shoulder exam should be performed given the association of additional shoulder pathology and subsequent influence on surgical planning.
Imaging
Radiographs play a minor role in the evaluation of patients with biceps-related complaints. Standard x-rays include true anterior-posterior (AP), axillary, and outlet views. Additional radiographic techniques (Fisk view) allow for visualization of the bicipital groove that may demonstrate spurring or narrowing (1). X-rays primarily rule out other causes of shoulder pain including fractures, arthritis, and glenohumeral dislocation.
Magnetic resonance imaging (MRI) provides valuable information concerning the biceps tendon. The ability to view the LHBT in multiple planes readily identifies both inflammation and tears of the tendon (10). As a sensitive diagnostic modality, MRI allows for identification of additional contributors to shoulder pathology, which improves preoperative planning. The addition of contrast may increase imaging sensitivity, but is rarely necessary.
Decision Making
Once it has been decided to proceed with surgical intervention and all the pathologic contributors to the patient’s shoulder pain and dysfunction have been identified, it is necessary to select a surgical approach to the long head of the biceps tenodesis. For the majority of patients, arthroscopic techniques are readily employed and open approaches are rarely needed. For surgeons comfortable with basic arthroscopy, an arthroscopically assisted, miniopen approach is a reasonable alternative to an all inside soft tissue or bony biceps tenodesis. When the preoperative evaluation reveals a substantial subscapularis tendon tear and/or dislocation of the LHBT, then an open deltopectoral approach is a good option for both fixation of the rotator cuff and bony tenodesis of the biceps tendon.
SURGICAL TECHNIQUE
Anesthesia
An anesthetic regimen is determined after discussion between the patient, anesthesiologist, and orthopaedic surgeon. Depending on the skill and comfort of the anesthesiologist, patients may elect to undergo regional or general anesthesia. Regional nerve blocks provide the added benefit of less postoperative pain, earlier discharge,
and lower admission rates (8). Interscalene blocks, expertly performed under ultrasound guidance and a nerve stimulator, provide adequate anesthesia of the upper extremity when appropriately placed. Patients should be well informed of the potential rare complications including, but not limited to, pneumothorax, Horner syndrome, recurrent laryngeal nerve and phrenic nerve paralysis. The operative site is identified, initialed by the surgeon, and marked “yes” prior to entry into the operating room.
and lower admission rates (8). Interscalene blocks, expertly performed under ultrasound guidance and a nerve stimulator, provide adequate anesthesia of the upper extremity when appropriately placed. Patients should be well informed of the potential rare complications including, but not limited to, pneumothorax, Horner syndrome, recurrent laryngeal nerve and phrenic nerve paralysis. The operative site is identified, initialed by the surgeon, and marked “yes” prior to entry into the operating room.
Setup
Shoulder arthroscopy is typically performed in either the “Beachchair” or lateral decubitus position depending on the training and comfort of the orthopaedic surgeon. Regardless of the position, it is essential that the patient is appropriately placed with all susceptible neurovascular structures and bony prominences well padded. The eyes must also be protected from inadvertent maneuvers or instrumentation during the procedure. An advantage of regional nerve blocks is that the patient may be positioned and questioned about comfort prior to the start of the procedure. Both arthroscopic and miniopen biceps tenodesis may be performed in either the beachchair or lateral decubitus position. Open biceps tenodesis should be performed in the beachchair position; however, if a diagnostic arthroscopy is not part of the procedure, it may be performed supine.
Beachchair Position
The patient is placed supine on the operating table with a head support. The table is then flexed at the waist to approximately 80 degrees, the hips flexed 20 degrees, the knees flexed 30 degrees, and 15 degrees of Trendelenburg. Several attachments are available for the operating table that allow for securing the patient’s head or gaining increased access to the shoulder by removing a posterior support. Regardless of the table, the patient’s head, neck, and torso should be secured in a natural, neutral position. The nonoperative arm is padded and secured to the waist or arm holder (Fig. 7.1).
Lateral Decubitus
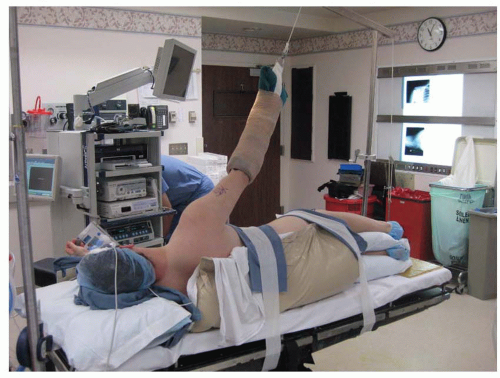
The patient is placed supine on a supportive beanbag on the operating table. After induction of anesthesia, the patient is placed in the lateral decubitus position with the operative extremity toward the ceiling. An axillary roll is placed just distal to axilla under the thorax of the nonoperative arm that is supported on an armboard. The head and neck padded and secured in a neutral position. The beanbag is insufflated to the contour of the patient’s body with particular padding in the breast and the genital area. The operative extremity is placed into the foam arm sleeve, abducted 30 to 45 degrees, and attached to the traction tower. No more than 15 lb. of traction weight should be applied as to minimize strain on the brachial plexus (Fig. 7.2).
Surface Landmarks/Portal Placement/Diagnostic Arthroscopy
The anatomic landmarks of the shoulder are identified and include the borders of the clavicle, acromion, and scapular spine (Fig. 7.3). The coracoid process is also marked. An exam under anesthesia is performed for all cases, but has limited value for primary pathology of the LHBT. The patient is sterilely prepped and draped. The glenohumeral joint is insufflated with 60 mL of Lactated Ringer solution using a No. 18 gauge needle through the posterior shoulder. Filling the joint allows for easier arthroscopic trochar placement and helps avoid damage to the articular cartilage.
The posterior viewing portal is established using a No. 11 blade scalpel 2 cm medial and inferior to the posterolateral corner of the acromion. The trochar is inserted and the joint viewed. A diagnostic arthroscopy is performed to not only evaluate the biceps tendon, but also to assess the surrounding structures including the capsule, rotator cuff, labrum, and articular cartilage that is not easily accessible through a single incision open approach (Fig. 7.4). After assessment of the glenohumeral joint, an anterior working portal is established.
A No. 18 gauge spinal needle is placed into the rotator interval anteriorly, at the level of and just lateral to the coracoid process to plan the portal. A No. 11 blade scalpel is used to make the skin incision and a cannula is inserted. Cannula sizes vary by manufacturer but need to be large enough (>6.0 mm) to accommodate the various arthroscopic instruments and anchors that the surgeon typically uses. Larger-sized or additional cannulas may be required based on the pathology that needs addressed. When only a biceps release or tenotomy is performed, it is possible to avoid using a cannula and create a smaller capsulotomy with a blunt 4.5-mm obturator or trochar that allows the arthroscopic synovator, grasper, and scissors to enter the joint with little damage to the capsule. The proximal LHBT may be further inspected for disease by pulling the tunnel portion into the joint with an arthroscopic grasper.
A No. 18 gauge spinal needle is placed into the rotator interval anteriorly, at the level of and just lateral to the coracoid process to plan the portal. A No. 11 blade scalpel is used to make the skin incision and a cannula is inserted. Cannula sizes vary by manufacturer but need to be large enough (>6.0 mm) to accommodate the various arthroscopic instruments and anchors that the surgeon typically uses. Larger-sized or additional cannulas may be required based on the pathology that needs addressed. When only a biceps release or tenotomy is performed, it is possible to avoid using a cannula and create a smaller capsulotomy with a blunt 4.5-mm obturator or trochar that allows the arthroscopic synovator, grasper, and scissors to enter the joint with little damage to the capsule. The proximal LHBT may be further inspected for disease by pulling the tunnel portion into the joint with an arthroscopic grasper.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree