Resurfacing Hip Arthroplasty
Evolution, Design, Indications, and Results
Michael L. Caravelli and Thomas Parker Vail
Key Points
Introduction
Modern total hip arthroplasty is considered one of the most successful surgical treatments ever developed. Its current form resulted from an evolution of ideas starting in the late 19th century. Resurfacing hip arthroplasty (RHA) is one adaptation along the course of this evolution. RHA was conceptualized and then championed as a technique that better replicated the normal anatomy of the hip and conserved host bone. In its early clinical application, RHA was met with unanticipated complications including femoral fracture, osteonecrosis, materials failure, and implant loosening. Today, with the advent of bearing material improvements and better understanding of tribology as related to large-diameter hip bearings, RHA remains a viable option for hip reconstruction in properly indicated patients. Issues and concerns associated with patient selection, risks associated with metal bearings, and exacting surgical techniques continue to limit wide adoption of the technology.
History and Evolution
Before 1900, treatment for osteoarthritis of the hip was dominated by joint excision and amputation. Toward the end of the 19th century, interest developed in interpositional materials that were founded on the successes of Heinrich Helferich, who used interpositional tissue successfully to treat temporomandibular joint arthritis.1 The lack of reliable results of interposition forced the development of other techniques. Marius Smith-Petersen, in Boston, Massachusetts, is credited with the development in 1923 of the concept of mould arthroplasty, a technique that may be considered the grandparent to resurfacing hip arthroplasty (RHA). Smith-Petersen conceptualized mould arthroplasty as the introduction of a biologically inert material that would be removed after it successfully served to “guide nature’s repair so that defects would be eliminated.”2 Unfortunately, because of the formation of fibrocartilage beneath the mould, the material was not mechanically stable; thus this procedure did not become the expected panacea. In most cases, the mould was left in place, serving as a permanent rather than a temporary interpositional graft. From these origins, the procedure, which was initially conceived as a temporary interposition, evolved into a more permanent femoral hemiresurfacing. The mould arthroplasty concept came to be referred to in the literature as cup arthroplasty. The cup substrate material evolved over time, starting with the original glass and transitioning through viscaloid, pyrex, and vitallium. Outcomes for these devices did show some early benefit in terms of pain control, but gait, motion, material performance, and consequently implant survival were unpredictable.3–9
Parallel to the development of cup arthroplasty was the introduction of a femoral endoprosthesis. The Judet brothers, in 1950, garnered popularity for their published resection-reconstruction technique, which involved implantation of a femoral component made from an acrylic resin. Their favorable early results set the stage for further development of resurfacing implants, but limited ability to withstand stresses at the hip joint and acetabular erosion caused by the articulation with acrylic material posed significant problems.10
Sir John Charnley was given credit for developing the first total resurfacing arthroplasty. He had developed a two-piece low-friction resurfacing device made of Teflon (polytetrafluoroethylene) that unfortunately failed rapidly as the result of wear. Although Teflon had very favorable low-friction characteristics, it proved vulnerable to shear loading and abrasive wear. After Charnley’s attempt to resurface the proximal femur, a number of devices came to the foreground. In 1960, Townley introduced the total articular resurfacing arthroplasty (TARA), a metal-on-polyurethane bearing with a stemmed resurfacing femoral component. Townley changed the socket to polyethylene, but his rate of failure from aseptic loosening due to frictional torque or osteolysis from the large-diameter head still was unacceptably high.11,12 In 1967, Maurice Muller created a metal-on-metal (MOM) surface replacement. Reportedly, he abandoned the MOM device in favor of the low-friction metal-on-polyethylene (MOP) total hip arthroplasty in 1968, also because of problems of loosening attributed to high frictional torque through the bearing, which caused untimely disruption of the bone-cement interface.13 Gerard, in 1970, took a different approach, unifying the concepts of hemiresurfacing of the femur and “mould arthroplasty.” He resurfaced the femur with a Luck cup and inserted it into an Aufranc cup that approximated the diameter of the host acetabulum. Treatment of pain over the short term was acceptable, but after 2 years, complications due to resorption of femoral bone, femoral fracture, and acetabular medialization were seen.14 RHA implant systems, also referred to in the literature as socket-cup devices, out of Japan with MOP bearings were reported over short-term to mid-term time periods. Furuya, in 1971, created a socket-cup arthroplasty that, despite alterations in bearing materials, required revision to total hip arthroplasty in 7 out of 12 cases.15 Nishio, in 1972, designed an uncemented socket and cup replacement of the hip. He reported that 86% of patients had pain relief and only 3 of 67 hips required revision.16 Tanaka’s hybrid arthroplasty with a cemented polyethylene acetabulum and uncemented femoral component yielded pain relief in 97% of patients, and no component revisions were required at the time of publication.17 In Italy, the Paltrinieri-Trentani surface arthroplasty was implanted, with 12% of cases failing as the result of neck fracture or component loosening.18 The efforts of Freeman, Wagner, Eicher and Capello, Amstutz, and Buechel and Pappas were comparable.19–23
Cumulative review of the results of first-generation resurfacing devices revealed two main complications. First, the interaction of the large bearing surfaces caused high frictional torque, presumably causing loosening of the socket, and the hard-on-soft articulation led to higher levels of volumetric wear and acetabular osteolysis. Second, there was a high incidence of femoral neck fracture presumably due to notching of the superior neck—a practice that was accepted because of the contemporary teaching that the femoral component should be in 140 degrees of valgus for proper stress transfer through the components. With the guarded results of RHA and the international success that Charnley enjoyed with his low-friction arthroplasty concept, the orthopedic community weighted the effort of innovation toward optimizing the MOP total hip arthroplasty (THA). Although these first-generation resurfacing devices differed in form, the consistent rationale in this era was the belief that these procedures were bone conserving and were indicated for patients younger than 60 years, in whom a Charnley low-friction THA was relatively contraindicated because of the greater difficulty and likelihood of future revision. Charnley’s low-friction THA had become the preferred procedure for patients older than 60 years; however, a predictable solution for treating the young patient with hip osteoarthritis still was not clear. Experience gained during these years did help build an appreciation for the meticulous technique and sound design required for successful use of RHA.
Metal-on-metal (MOM) bearings were introduced during the early development of hip arthroplasty as a low-wear, low-friction, durable, and biologically stable bearing combination. The Muller, McKee-Farrar, Ring, Wiles, Stanmore, and Sivash total hip systems and various hemiarthroplasty combinations were being used at the time. Results with MOM bearings in these first-generation implants were not satisfactory.13 A high rate of component loosening due to frictional torque, equatorial seizing of matched bearings, fatigue fracture of the acetabulum, and infection; concern about systemic effects of metal ions; and the early success of the Charnley THA played a role in sidelining the MOM bearing. A rejuvenation of interest in MOM bearings emerged in the late 1980s. Published comparative studies between the McKee-Farrar and Charnley implants demonstrated comparable mid- to long-term survival of MOM bearings, stimulating discussion and further development of the technology.24,25 From 1983 to 1988, Bernard Weber and Sulzer Orthopaedics manufactured the Metasul bearing. The design consisted of a CoCrMo alloy bearing with a 28-mm or 32-mm metal head articulating with a metal socket as an inlay in polyethylene. RHA components were designed by Heinz Wagner and Derek McMinn. The Wagner RHA, introduced between 1990 and 1992, had an inlay-forged CoCrMo articulating surface with a grit-blasted titanium surface coating at the bone interfaces. The McMinn prosthesis, introduced between 1991 and 1993, had a cast CoCrMo design with an acetabular component with hydroxyapatite (HA) coating and peripheral fins for rotational stability. Both designs led to improved results in terms of loosening, and neither was associated with femoral fracture.23,26
Concurrently, efforts were being made to improve acetabular component fixation in total hip arthroplasty. Aseptic loosening of cemented acetabular components was a considerable problem at mid-term follow-up.27,28 Jones and Hungerford and Jasty and associates published early works on the pathophysiology of this problem.29,30 Porous-coated acetabular components that would achieve biological fixation were developed. The Harris-Galante cup and the porous-coated monatomic (PCA) cup were two of the early prototypes. By the mid-1990s, sufficient evidence and positive survivorship data supported the durability of porous-coated acetabular components.28,31-33
With advanced knowledge of large bearing function and the possibility of a durable biological cementless acetabular fixation, the stage was now set for development of the RHA systems that are currently in use. An evolution over four decades resulted in improvements in materials, acetabular fixation, bearing function, and implant technique. Figure 63-1 illustrates an evolution from femoral hemiresurfacing to MOP bearings to the current MOM bearings.
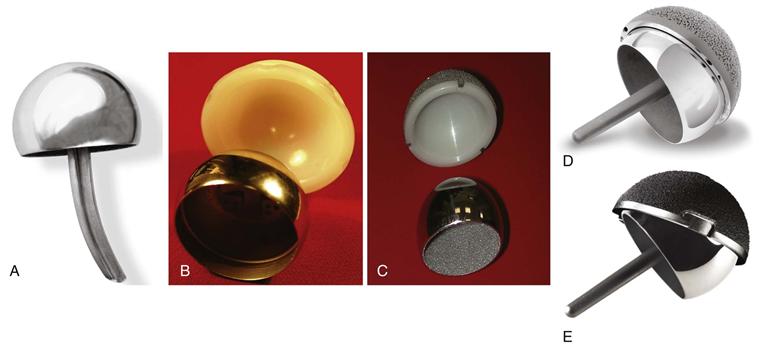
Figure 63-1 A, Total articular resurfacing arthroplasty (TARA) hemiresurfacing component. B, Total hip articular replacement by internal eccentric shells (THARIES) resurfacing components. C, Porous surface replacement (PSR). D, Birmingham resurfacing components. E, Conserve Plus (Wright Medical Technology, Arlington, TN) resurfacing components.
The Wagner prosthesis was manufactured by Protek AG (Bern, Switzerland), a company founded by Maurice Muller. The McMinn prosthesis underwent a series of evolutions through Corin Medical to become the Cormet 2000 (Corin Medical, Cirencester, Glos, United Kingdom) and subsequently the Birmingham Hip (Smith and Nephew, London, United Kingdom). Harlan Amstutz after his initial work with the THARIES (total hip articular replacement by internal eccentric shells) resurfacing components developed the Conserve Plus system with Orthomet (Minneapolis, Minn), a company that was purchased by Wright Medical (Clarion, Iowa). Biomet (Warsaw, Ind) designed the ReCap system. DePuy (Warsaw, Ind) designed the articular surface replacement (ASR) system. Zimmer (Warsaw, Ind) designed the Durom system. The final common system was a hybrid design with a cementless acetabular component and a cemented femoral component. This is the current standard.
Design
Tribology is the study of interacting surfaces in tangential motion. The main principles that define this interaction are friction, lubrication, and wear. Its study, therefore, includes material properties of the bearing surfaces, bearing geometry, joint kinematics, and load patterns. These properties are then modified by the dynamic interaction between surfaces manifested by joint lubrication, joint kinematics, and contact area. A brief review of these material properties facilitates understanding of the evolution of design of RHA components.
Friction is an extrinsic force that develops from the interaction of two moving solid objects. Its magnitude is a result of the physical and chemical microstructure of the contacting surfaces. Early MOM components were believed to have failed early as the result of high frictional torque that disrupted the skeletal fixation, clinically manifested by early acetabular loosening.34,35 In an acetabular bearing, frictional torque (Q) is determined by the formula Q = µRr, where µ is the friction coefficient, R is the vertical component of the load in the plane of measurement, and r is the radius of the femoral head.36 In simplistic terms, the frictional torque is proportional to the coefficient of friction between articulating surfaces, the load, and the radius of the femoral head. A catastrophic example of excessive frictional torque would be instantaneous cup displacement or fracture of the cement mantle or host bone, but frictional torque in an MOM implant has been shown to be an order of magnitude less than would be required for this to occur in a metal-on-polyethylene bearing.37,38 Lower levels of frictional torque over time, however, can be quantified by progressive component loosening and wear, defined as erosion of material from a solid surface due to its interaction with another surface.
The measurement of wear is of much greater importance in evaluating these articulating materials because of the clinical implications of osteolysis and subsequent aseptic loosening. The dominant wear modes seen in hip arthroplasty are adhesive, abrasive, and corrosive. Specifically, with MOM implants, adhesive wear, because of the self-polishing ability of CoCrMo alloys and matched bearing hardness, is less prominent than that seen in unmatched bearing couples. Wear in MOM bearings, as determined in hip simulator studies, is characterized by an initial “running-in” period followed by a “steady-state” over the remaining lifetime of the implant. Conclusions from the literature have demonstrated that high carbon content CoCrMo alloys (>0.20% C), femoral heads greater than 28 mm, and the lowest practical diametric clearance lead to the lowest quantitative volumetric wear.39–41 With regard to carbon distribution in the high-carbon alloy, however, there have been contradictory results that still need to be worked out.42,43 Another concern with the resurgence of MOM bearings is the effect of corrosion, especially with higher levels of Co2+ systemically. In vitro analysis by Yan and colleagues suggests that high-carbon alloys have sufficient corrosion resistance to limit the total volumetric wear produced by the bearing.44
Lubrication conditions seen in MOM bearings exert a significant influence on volumetric wear. Lubrication regimens include boundary lubrication, mixed lubrication, and fluid film lubrication. Boundary lubrication relies on physicochemical interactions between lubricating fluid, any additives, and contacting solid surfaces. Fluid film lubrication occurs with entrainment of lubricant between interacting solid surfaces, preventing their contact. Mixed lubrication demonstrates characteristics of both. Theoretical predictions of the predominant lubrication regimen are made with the lambda ratio: Λ = Theoretical minimum film thickness/Composite surface roughness. A Λ ≤ 1 leads to boundary lubrication, 1 ≤ Λ ≤ 3 leads to mixed lubrication, and Λ ≥ 3 leads to fluid film lubrication.36 Modern manufacturing techniques have succeeded in producing accurate bearing geometry and highly polished bearing surfaces that optimize the potential for articulation in the fluid film lubrication regimen. Fluid film thickness is influenced by diametric clearance of the bearing, defined as the distance between the outer diameter of the convex surface and the inner diameter of the concave surface. Recommended diametric clearances typically are based on in vitro data, but the smallest practical clearance that will not lead to equatorial seizing, along with a femoral articulating surface that deviates less than 10 µm from sphericity and surface roughness less than 0.05 µm, maximizes the potential for the articulation to operate in the fluid film lubrication regimen. It is also important to point out the need for a durable acetabular component that undergoes minimal deformation with implantation, as this can alter the expected clearance.45,46
Aside from the tribologic requirements for a successful RHA bearing are biological considerations including the potential for biological fixation. As was discussed earlier, first-generation RHA components and MOM bearings with large-diameter heads experienced short-term failure from acetabular component loosening. The cause of these early failures likely was multifactorial and included inferior component fixation with early-generation cement techniques, high levels of wear particles caused by a large-diameter metal head articulating with conventional polyethylene, and higher frictional torque than was seen with the 22-mm articulation used by Charnley. With the evolution of porous-coated sockets, biological fixation of the acetabular component has become more predictable. Yet the challenge of positioning and properly seating a monoblock acetabular shell remains. The experience with cemented femoral components in hemiarthroplasty47 and the experience reported in hybrid total hip resurfacing26,48 suggest that femoral fixation is durable in the first decade but seems to have a slightly increasing incidence of loosening over time. Hypothesized causes of femoral component loosening include selection of cases with structurally inadequate host bone, osteolysis from particulate debris, stress shielding causing undesirable femoral neck remodeling, host bone necrosis related to thermal properties of cement or damage to the blood supply, and fracture. If local bone necrosis is related to the cement, there may be some theoretical advantage of using a cementless femoral component, provided that biological fixation could be achieved. Several groups have published their early results on cementless femoral resurfacing prostheses, but no consensus has been reached on their clinical application or durability at this time.49–51
Indications
RHA is indicated as an alternative to total hip replacement in a select group of patients with good proximal femoral bone quality for whom a metal-on-metal bearing is an acceptable risk. The key to defining proper indications for RHA is to identify when the risk-to-benefit ratio for RHA is more favorable than the risk-to-benefit ratio for THA. Current indications include the patient for whom the benefits of bone conservation are maximal. Thus, the ideal candidate is generally younger and consequently has a higher likelihood of ipsilateral revision, desires a high-activity lifestyle, and possesses good proximal femoral bone quality. Registry data suggest that smaller size, female gender, and age over 70 years may predispose to greater risk of complications or reoperation, and younger, larger male patients may be the better candidates.52,53
The most difficult challenge associated with THA performance has traditionally been associated with the young and active male patient. Lower component survivorship rates in this population due to wear and osteolysis have been hypothesized to be a result of insufficient ability of the bearing material and implants to tolerate increased activity levels and an extended life span.54 The young patient after any arthroplasty, therefore, has a significantly greater probability of requiring revision hip reconstruction in the future, although low risk in the first decade, periprosthetic fracture, bone loss due to stress shielding, infection, and substrate failure remain long-term concerns with total hip replacement. The typical patient for whom RHA is considered has symptomatic hip osteoarthritis, is between 30 and 60 years of age (average age 49, compared with 67 for THA),55 and is still employed and physically active. Current data from the Central Intelligence Agency estimate average life expectancy in the United States to be 78.11 years.56 This would require many of these young patients to get well more than 20 years from the time of receiving their implants—an achievement that cannot be reliably expected based on current survivorship results. Unfortunately, results of revision hip reconstruction are inferior to those of primary reconstruction. Higher rates of dislocation, perioperative and postoperative complications, lower functional scores, and decreased implant survivorship have been demonstrated after revision hip reconstuction.57–60 RHA offers a potential alternative to the failed total hip scenario in that the femoral resurfacing component can be revised to a stemmed femoral component—a procedure that is less demanding, technically, than a standard femoral component revision. Conversion of resurfacing to a total hip has been shown in small series to be a stable, durable alternative to THA over the short and mid-term that does not appear to limit the effectiveness of THA.61,62 Nevertheless, it must be recognized that the complexity of revising a hip resurfacing device is related to the diagnosis at the time of revision. Patients with uncomplicated fracture or aseptic loosening can be more easily revised with higher functional expectations than patients revised because of an adverse soft tissue reaction that causes local tissue destruction with muscle necrosis.
Not all of the proposed advantages of hip resurfacing have been proved. Proposed advantages of RHA include femoral bone preservation, uncomplicated revision in most cases, a low dislocation rate, durability of the metal-bearing couple, and a more physiologic reconstruction as measured by an improved gait pattern and fewer activity limitations. Risks associated with RHA, on the other hand, are not theoretical and have been well described in the literature. Some complications of hip resurfacing have been related to early experience and a “learning curve.”63–65 Higher rates of component loosening, primarily on the femoral side, may be due to patient selection and technical issues such as cement technique and component malposition. Causes of aseptic loosening of the acetabular component differ little from those of THA and include failure to achieve primary fixation, full component seating, and impingement. Progressive femoral neck narrowing, femoral neck fracture, femoral head-neck necrosis, acetabular and femoral component loosening, and sequelae from metal particles are the most frequent complications associated with RHA. Acetabular malposition in RHA such as a high lateral opening angle or increased anteversion may predispose to edge loading, which has been shown to elevate wear rates and both systemic and local ion levels.66 The consequences of metal particles and ions have yet to be fully and conclusively elucidated. However, it is clear that a spectrum of local tissue reactions from benign to severe is associated with exposure to metal ions. These reactions have been described as having features of hypersensitivity, as demonstrated by perivascular lymphocytic infiltration. More dramatic clinical presentations with pain and local fluid accumulation, fibrosis, and muscle and tendon necrosis have been described in association with high local levels of chromium and cobalt ions. This potential led to a medical device alert in April and May of 2010 from the Medicines and Healthcare Products Regulatory Agency, an agency of the Department of Health in the United Kingdom.67–70
RHA is an acceptable option when there does not exist a major biomechanical problem such as leg length discrepancy, coxa vara, or a severe sequela of a childhood hip disorder such as developmental dysplasia (DDH) or Perthes disease. Although it is possible to make some minor changes in the location of the hip center when placing the acetabular component during hip resurfacing, it is not possible to lengthen the leg or increase the offset substantially. Success rates with resurfacing have been lower with DDH, Perthes, and osteonecrosis of the femoral head than with osteoarthritis, in part because of the biomechanical limitations of a resurfacing construct. Abnormal femoral morphology described as a head-to-neck ratio less than 1.2, short neck length, femoral head cysts larger than 1 cm, and decreased bone density increases the risk of femoral neck fracture.71,72
Absolute contraindications to RHA, similar to THA, include active infection of the hip joint and the presence of systemic infection. Patients with known metal hypersensitivity should be avoided, although presently no test is predictive of clinical problems for a joint implant related to metal sensitivity. Patients with renal insufficiency are not good candidates for resurfacing because ions released from the bearing surface are cleared through the kidneys. Women of childbearing age should be approached with caution or eliminated from consideration for hip resurfacing because of known potential for fetal exposure by metal ions and lack of complete understanding of potential adverse effects to a fetus of ion exposure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








