Chapter 53 Rehabilitation of the Surgically Reconstructed and Nonsurgically Treated Anterior Cruciate Ligament
The anterior cruciate ligament (ACL) serves a number of roles within the knee. The ACL is the primary restraint to anterior tibial translation relative to the femur. It also assists in varus and valgus knee stability, provides proprioceptive feedback, guides the screw-home mechanism that occurs during knee extension, and prevents knee hyperextension.43 Consequently, ACL injuries may result in significant functional deficits. Recurrent episodes of joint instability have been associated with meniscal injury and damage to the articular cartilage. Furthermore, ACL injuries, whether treated surgically or nonsurgically, predispose to the development of knee osteoarthritis.24,26,78 Whether a patient chooses surgical or nonsurgical management, rehabilitation is an integral part of the treatment program. Rehabilitation techniques have evolved substantially over the past 25 years. The goals of nonoperative and postoperative ACL rehabilitation programs include return of neuromuscular control, strength, power, and functional symmetry.77 This chapter will discuss current recommendations for nonoperative and postoperative rehabilitation of ACL injuries.
Nonoperative Rehabilitation of Anterior Cruciate Ligament Injuries
Traditionally, nonoperative management of ACL injuries has been offered primarily to those participating in International Knee Documentation Committee (IKDC) level III or IV activities (Table 53-1).62 A number of studies have reported poor outcomes and limited success in returning to IKDC level I and II sports with nonoperative treatment of ACL injuries.* Furthermore, other studies have demonstrated that the incidence of medial meniscal tears increases over time in ACL-deficient knees, which may predispose to early-onset knee osteoarthritis.† A study by Levy and Meier66 found the incidence of meniscal tears in chronically ACL-deficient patients to be 40% at 1 year, 60% at 5 years, and 80% by 10 years postinjury. The ACL has been referred to as “the guardian of the meniscus.”87 Ultimately, the goal of treatment following ACL injury is to provide the patient with the best functional outcome and to minimize the risk of future injury and/or development of knee osteoarthritis.
Table 53-1 International Knee Documentation Committee Activity Levels
| Level | Sports Activity | Occupational Activity |
|---|---|---|
| I | Jumping, cutting, pivoting | Jumping, cutting, pivoting |
| II | Lateral movements, but less pivoting than level I sports | Heavy manual labor on uneven surfaces |
| III | Linear activities with no jumping or pivoting | Light manual work |
| IV | Sedentary activities | Activities of daily living |
Adapted from Haggmark T, Eriksson E: Cylinder or mobile cast brace after knee ligament surgery: a clinical analysis and morphological and enzymatic study of changes in quadriceps muscle. Am J Sports Med 7:48–56, 1979.
For individuals with an isolated ACL injury who lead a sedentary lifestyle, do not experience instability during activities of daily living (ADLs), and have no concomitant injury requiring surgical intervention, nonoperative treatment is an appropriate option. However, in patients who participate in IKDC level I or II activities, correct identification of individuals who can dynamically stabilize their knee (copers) is imperative to meet the goals of optimizing functional outcome and minimizing the risk of future knee injuries and knee osteoarthritis. There is evidence that individuals who meet specific post-ACL injury screening criteria and successfully complete a rehabilitation program involving perturbation training and a sport-specific functional progression can return to cutting, pivoting, and jumping types of sports 63% to 79% of the time without subsequent episodes of instability, injury, or reduced functional status.27,35,56,57
Dynamic knee stability can be defined as the ability to stabilize the knee during the rapidly changing loads created by activity.57 Dynamic knee stability is dependent on neuromuscular control when static restraints (e.g., the ACL) are absent. Also affecting the ability to regain dynamic knee stability are the proprioceptive deficits that occur in the knee following an ACL injury.6,7,10,112 Correction of proprioceptive deficits has become a focus of modern nonoperative and postoperative rehabilitation programs following ACL injury.17,23,77 This is achieved through controlled stimulation of joint mechanoreceptors and muscle spindles using proprioceptive and balance exercises to increase the sensitivity of mechanoreceptors and muscle spindles and improve the readiness of muscles to respond to destabilizing forces.
There are a number of stabilization strategies used by those who sustain an ACL injury. Patients who tend to experience instability episodes and poor functional outcomes (noncopers) following ACL injury attempt to stabilize their knees through excessive cocontraction of thigh musculature, reduced knee flexion during the load acceptance phase of gait, and a greater posterior tibial displacement when compared with copers and uninjured controls.18,19,94,95 By restricting knee flexion during load acceptance, noncopers maintain a relatively extended position of the knee, which may predispose to future subluxation episodes.53 Noncopers also preferentially recruit their quadriceps during unilateral stance postural perturbations, which may further destabilize the ACL deficient knee.26 Thus, noncopers stabilize the knee through abnormal muscular recruitment patterns and by limiting knee movement whereas copers attempt to normalize knee movement and recruitment patterns.
Based on the earlier work of Eastlack and colleagues,27 Fitzgerald and associates35 have developed a screening examination whereby potential copers and noncopers could be distinguished. This screening examination has been used successfully by other investigators.57,58 According to these criteria, patients were not considered candidates for the screening examination and were referred to an orthopedic surgeon for ACL reconstruction surgery if they had any of the following: a fracture, reparable meniscal tear, multiligament knee injury, or full-thickness articular cartilage lesion. They also could not have experienced more than one instability episode since sustaining the ACL injury. Prior to the screening test, patients participated in a rehabilitation program to resolve their knee effusion, restore full knee range of motion (ROM), strengthen their quadriceps muscle to 70% or more of the isometric strength of their contralateral extremity, and improve their weight-bearing status to the point at which they could hop on the injured leg without pain. Patients who did not meet these criteria after 1 month of rehabilitation were not considered candidates for the screening examination and were referred for ACL reconstruction surgery.
The screening examination included a timed 6-m single-leg hop test, global rating of knee function, and knee outcome survey–ADL rating. Potential copers were identified by hop test scores 80% or more of their contralateral limb, global rating of knee function of 60% or more, and a knee outcome survey–ADL score of 80% or more. Patients who met these criteria were enrolled in a physical therapy program that involved exercises for strength, endurance, agility, balance, and proprioception. A sport-specific functional progression was also included in the physical therapy program. Approximately two thirds of individuals identified as copers were able to return to IKDC level I or II sports without subsequent episodes of instability, injury, or reduced functional status after completing the physical therapy program.27,35,56,57
Using the screening test of Fitzgerald and coworkers,35 Hurd and colleagues56,57 were able to identify several additional characteristics that assist in differentiating ACL deficient copers from noncopers. A timed single-leg hop test demonstrating less than 10% difference between the injured and uninjured sides was the greatest predictor of a high level of self-assessed global function postinjury. In addition, noncopers were more likely to be female, to have sustained an ACL injury via a noncontact mechanism, and to have less quadriceps strength than copers. Furthermore, noncopers participated in fewer hours of IKDC level I or II sports preinjury.
For patients with isolated ACL injuries who have not experienced a postinjury subluxation episode and who only participate in IKDC level III or IV activities, we suggest a trial of nonoperative management. We recommend ACL reconstructive surgery for the following individuals: patients who participate in IKDC level I or II activities or who have experienced at least one postinjury subluxation episode, have sustained a multiligament knee injury, or have a concomitant repairable meniscal and/or significant chondral injury. If a patient who participates in IKDC level I or II activities sustains an isolated ACL injury and requests a trial of nonoperative treatment, we recommend performing the screening examination outlined by Fitzgerald and associates.35 If the patient does not pass the screening examination, we recommend ACL reconstructive surgery. If the screening examination is passed, the patient is enrolled in a nonoperative ACL injury rehabilitation program. The following is a description of this nonoperative ACL injury rehabilitation program (Table 53-2).
Table 53-2 Nonoperative ACL Rehabilitation Summary
| Examination Phase | Goals |
|---|---|
| Prescreening | |
| Postscreening |
Prescreening Examination Rehabilitation Phase
Pain can be reduced through local physical modalities such as cryotherapy and electrical stimulation and the judicious use of analgesic medications.112 Resolution of any knee effusion facilitates knee ROM, improves the patient’s ability to ambulate, and reduces reflex quadriceps inhibition.25,60,107 Active contraction of the calf musculature with active ankle ROM exercises also facilitates edema reduction and may prevent complications of venous stasis. Knee ROM exercises include heel slides, active knee ROM, active assisted knee flexion with the arms or uninvolved leg, stationary bicycle–assisted knee flexion, towel stretches, overpressure knee extension with 2.5 to 10 pounds of weight, prone hangs, and passive knee extension while propping the heel up on a towel.
Isometric quadriceps-strengthening exercises can be initiated immediately following the injury and include quadriceps setting and straight leg raises. If the patient is unable to contract their quadriceps muscle actively either because of reflex inhibition from a large knee joint effusion or significant pain, high-intensity neuromuscular electrical stimulation can be applied to the quadriceps musculature to facilitate quadriceps contraction.105 Closed kinetic chain (CKC) exercises can also be safely used during the prescreening phase of rehabilitation and will produce minimal anterior tibial displacement forces across the knee.11,49,80,81,116 CKC exercises promote normal muscle activation patterns, enhance joint stability through muscular cocontraction, provide proprioceptive input through joint compressive forces and mechanoreceptor stimulation, mimic normal functional movements, and assist in strengthening the quadriceps muscles and ACL antagonist muscles (e.g., gastrocnemius and hamstrings).42 Open kinetic chain (OKC) exercises for the quadriceps can also be used during the prescreening examination phase of rehabilitation, but should be limited to the ROM within 90 to 45 degrees of knee flexion because of the increased anterior displacement of the tibia at lower knee flexion angles.12,76 OKC hamstring exercises can be performed through the entire knee ROM.
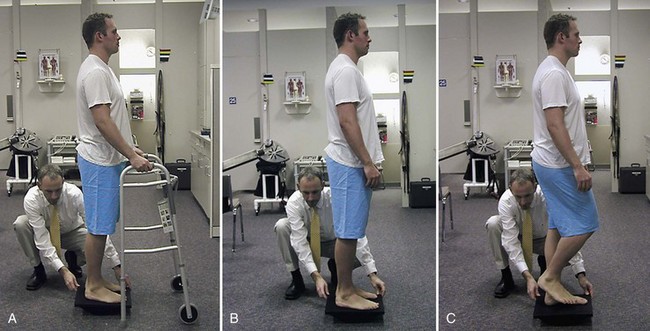
Proprioceptive exercises begin in this phase of rehabilitation. Early proprioceptive exercises can be accomplished with a combination of joint repositioning drills and with CKC exercises, such as weight shifts and joint repositioning exercises.114 A compressive sleeve used for edema control may also improve knee proprioception and should be worn during rehabilitation exercises.65 Minisquats can be progressed to be done on an unstable surface, such as a foam pad, based on the patient’s functional improvements. Functional activities, such as three-way lunges, step-ups, and cone step-over drills can also be incorporated into the rehabilitation program. As the patient’s ability to bear full weight and sense of knee stability improve, progression to single-leg balance exercises while standing on a stable surface can be attempted. Initially, single-leg balance exercises can be performed between parallel bars so that the subject can use the arms for support, if needed. Eventually, the patient can begin moving the non–stance leg in adduction-abduction and flexion-extension directions, and the upper extremities in flexion, extension, abduction, adduction, and diagonal patterns with or without weight, while maintaining knee stability.112 The amount of extremity excursion, rate of movement, and amount of resistance can be manipulated to alter the level of challenge posed by the exercise. The patient can eventually progress to standing on an unstable surface such as a foam pad (Fig. 53-1).
Finally, during the prescreening examination rehabilitation phase, the patient should maintain cardiovascular fitness through low-impact aerobic conditioning, progressing from a stationary bike to an elliptical machine. Running should not occur during this phase. The patient should also incorporate trunk and hip girdle strengthening exercises. In particular, the hip extensors, external rotators, abductors, and flexors should be strengthened to provide concentric (hip extensors, external rotators, and abductors) and eccentric (hip flexors) control of femoral adduction and internal rotation motions, which have been implicated as potential contributing factors to ACL injuries.52
Postscreening Examination Rehabilitation Phase
A key component to this phase of the patient’s rehabilitation program is the addition of perturbation training. Perturbation training has been shown to improve the functional outcomes in ACL-deficient patients when compared with rehabilitation without perturbation training.38 Perturbation training may be performed on a roller board and a tilt board (Fig. 53-2), and should occur two or three times/week. The speed, direction, and amplitude of perturbations should be varied by the therapist and applied in a random order as the patient becomes more proficient with the exercises. When the patient is able to perform all perturbation exercises in a single-limb position on the tilt board and roller board, with minimal disturbance in balance, sport-specific and functional tasks should be added to the program with the goal of creating learned compensatory responses to sport-specific and functional activities (Figs. 53-3 and 53-4). By performing perturbation training during sport-specific and functional tasks, improved carryover to real life situations may occur, thereby minimizing the chance of a subluxation episode or recurrent knee injury.
The patient should continue strengthening exercises focusing on the quadriceps, hamstring, gastrocnemius-soleus complex, hip girdle, and trunk. The principles of progressive resistance exercises and periodization are applied during this phase of rehabilitation. A periodized resistance training program may be divided into three phases.109
Rehabilitation After Anterior Cruciate Ligament Reconstructive Surgery
Surgical Considerations
Graft healing following ACL reconstruction is a complex biologic process influenced by a number of surgical and postoperative variables.28 These include graft type, graft position, graft tensioning and fixation, and individual patient factors. In general, the graft healing process following ACL reconstruction occurs in several phases. An initial inflammatory response occurs almost immediately.64 Graft revascularization occurs over the next several months and originates primarily from the infrapatellar fat pad, posterior synovial tissue, and endosteal vessels within the femoral and tibial tunnels.4 Over the ensuing months to years, remodeling or ligamentization of the intra-articular portion of the graft occurs, which is characterized by cellular repopulation, collagen remodeling, and ligament maturation.71
In general, options for graft type in ACL reconstruction include bone-patellar tendon-bone (BPTB) autograft, quadruple hamstring autograft, quadriceps tendon bone autograft, BPTB allograft, Achilles tendon bone allograft, and tibialis anterior allograft. The rates and characteristics of the graft healing process among these grafts clearly differ, and the specifics of these differences are not well understood. Several animal models have shown slower bone tunnel incorporation with soft tissue autograft and allograft compared with BPTB autograft.28,92 Although complete incorporation at the bone-tunnel interface has been shown to occur at 6 to 8 weeks with the use of patellar tendon autograft,83 the incorporation of soft tissue graft has been shown to be considerably longer, at 12 weeks.41,92 Although allograft tissue appears to heal in a similar manner to autograft tissue, this occurs at a much slower rate.44 In addition, compared with autograft tissue, allografts lose more of their time zero strength during remodeling. ACL reconstruction with allograft tissue has not been definitively shown to be associated with a poorer prognosis.52 Nonetheless, these differences should be taken into account when designing a rehabilitation program. Although a prospective randomized trial14 has shown that an accelerated rehabilitation program produces no difference in knee laxity, functional performance, synovial fluid biomarkers, or articular cartilage metabolism in patients reconstructed with a BPTB autograft, insufficient evidence exists regarding the safety of an accelerated rehabilitation program for patients undergoing ACL reconstruction with allograft tissue.
Secure mechanical fixation is required in the early postoperative period. A number of different fixation devices are available and include metallic and bioabsorbable interference screws for femoral and tibial fixation, suspensory and transfixion devices for femoral fixation, and combinations of aperture and augmentation devices for tibial fixation. A large number of studies have examined differences in biomechanical properties between various fixation devices at time zero; however, few studies have explored differences in biologic incorporation of grafts relative to individual fixation methods.28 Graft fixation is influenced by various physical properties, including graft material, bone density, fixation device, and fixation site.46 Although most fixation techniques have been demonstrated to perform well in clinical studies, it is important that the surgeon be familiar with the biomechanical properties of the individual system being used because the rehabilitation program may need to be adjusted accordingly.
Anatomic tunnel placement has recently been emphasized to achieve physiologic graft loading, promote bone graft healing, and restore knee stability.28 In particular, a more anatomic femoral graft placement has been shown to offer significant biomechanical advantages.119 With respect to graft tension, both excessively low tension and excessively high tension have been postulated to reduce the biomechanical properties of the graft. Further study is required to determine the optimal tension that should be applied relative to each graft type and fixation method. Delayed graft healing and tunnel enlargement have been postulated to occur secondary to excessive graft tunnel motion.54 Motion between the graft and bone tunnel has been correlated with the type of fixation used and the postoperative rehabilitation program. Although early knee ROM and weight bearing are considered to be beneficial, an early aggressive rehabilitation protocol may increase graft tunnel motion, thus affecting healing of the graft to bone. This phenomenon may be more likely to occur in the setting of nonanatomic femoral tunnel placement. Further study is required to determine the optimal load and optimal timing of the loads required for successful graft healing after ACL reconstruction.
Timing of Surgery and General Rehabilitation Considerations
Prior to undergoing surgery, the patient should demonstrate minimal knee effusion, and full symmetrical extension to minimize the postoperative complications of arthrofibrosis.73,102 The patient is allowed sufficient time to cope with the injury psychologically and prepare for the surgery and postoperative rehabilitation process, which requires significant commitment from the patient to optimize surgical outcome. Postoperatively, it has been reported by Shelbourne and Klotz103 that reestablishment of symmetrical knee ROM is a critical factor related to patient satisfaction. Thus, reestablishment of full symmetrical knee ROM should be a primary focus of the early postoperative rehabilitation program.
Cryotherapy
Several studies have demonstrated that cryotherapy reduces pain, edema, and inflammation in the postoperative setting.95,109 In an experimental knee swelling model, cryotherapy was found to be effective in reducing arthrogenic muscle inhibition induced by swelling.88 In a meta-analysis of cryotherapy following ACL reconstruction, it was found that cryotherapy has a statistically significant benefit in postoperative pain control.86 The study concluded that because cryotherapy is fairly inexpensive, easy to use, has a high level of patient satisfaction, and is rarely associated with adverse events, its use is justified.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree