Thirty-two sources of chronic obstructive pulmonary disease (COPD) prevalence estimation rates from 17 countries were surveyed. Prevalence ranged from 0.23% to 18.3%. In Europe and North America, rates were between 4% and 10% (
9). COPD is the second most common noninfectious disease in the world, causing 2.75 million deaths annually with global mortality predicted to double by 2030. It is the fourth largest cause of major activity limitation (
10). Thirty percent of COPD patients with forced expiratory volume in 1 second (FEV
1) less than 750 milliliters (mL) and 35% following an acute exacerbation die within 1 year (
11) and 50% within 3 years (
12).
Patient Evaluation
In addition to the elements of the patient evaluation noted in
Table 42-1, any medical, physical, financial, or psychological factors that might interfere with a rehabilitation program need to be addressed (
12). Commonly overlooked is the fact that 13% of COPD patients are anemic. This may indicate presence of erythropoietin resistance and be associated with increased serum inflammatory proteins (
13).
Various dyspnea assessment surveys can be used to objectify the extent of dyspnea and the effects of rehabilitation (
14,
15,
16,
17). In addition, the presence of any dyspnea, coughing, wheezing, chest pains, neurologic or psychological disturbances, allergies, previous communicable diseases, injuries, and nutritional imbalance is explored.
Poor nutrition can be characterized by low protein values. Other tests that assess nutritional status include total iron binding capacity, cholesterol, and serum vitamin levels, especially of vitamins A, C, and E. This is especially important because COPD and neuromuscular disease (NMD) patients have a high incidence of vitamin deficiencies. Delayed cutaneous hypersensitivity is a function of cell-mediated immunity and is the immune response most sensitive to nutritional deprivation. Hypophosphatemia, hypomagnesemia, hypocalcemia, and hypokalemia may also cause respiratory muscle weakness, which is reversible following replacement (
18). Social, educational, and vocational histories and any relevant environmental factors are explored.
The pulmonary function studies of COPD patients demonstrate air trapping, low-maximum midexpiratory flow rates and increased midexpiratory times, normal or increased lung compliance, and increased flow work. Residual volume and total lung capacity are generally increased. Exertional dyspnea tends to occur when the forced expiratory volume in 1 second (FEV
1) is less than 1,500 mL. FEV
1 decreases by 45 to 75 mL/yr for COPD patients (
19), a rate up to three times normal. Arterial oxygen tensions may be posturally related, significantly decreased with the patient supine (
20), and desaturation may be episodically severe during sleep (
21).
Since pulmonary function impairment does not predict the overall functional impairment, clinical exercise testing is done. This measures the functional reserve of all mechanisms taking part in oxygen and carbon dioxide transport and yields information regarding the capacity to perform exercise, the factors that limit exercise, the reasons for exercise-related symptoms, and the diagnosis (
22). It permits the clinician to determine whether the primary disability is pulmonary, cardiac, or related to exercise-induced bronchospasm (
23). The latter two diagnoses and even the presence of purely restrictive pulmonary syndromes are commonly mistaken for COPD and, therefore, may be mismanaged. Clinical exercise testing can also be useful for documenting patient progress with rehabilitation.
Clinical exercise testing, whether by using a treadmill, stationary bicycle, or upper-extremity ergometer, includes monitoring of: vital signs, electrocardiography, oxygen consumption, carbon dioxide production, the respiratory quotient, the ventilatory equivalent, minute ventilation, and metabolic rate. The respiratory quotient is the ratio of the carbon dioxide produced divided by the oxygen consumed. The ventilatory equivalent is equal to the volume of air breathed for 1 L of oxygen consumed. A metabolic equivalent (MET) is the resting metabolic rate per kilogram of body weight (i.e., 1 MET = 3.5 mL O
2/kg/min). Other useful measures for noninvasively assessing cardiac function include the oxygen pulse, a measure of the mL of oxygen consumed per heart beat (
23). A clinical exercise test should advance until oxygen consumption fails to increase, maximum allowable heart rate for age is reached (usually 220—age in years), or electrocardiographic changes, chest pain, severe dyspnea, or intolerable fatigue occurs. A minute ventilation 37.5 times the patient’s FEV
1 can be the goal (
24). Arterial blood gases may be normal at rest but are often abnormal during exercise. Oximetry is performed to determine need for supplemental oxygen therapy to maintain SpO
2 greater than 90% during reconditioning exercise or greater than 60 mm Hg long term (
25). It has been suggested that supplemental oxygen benefits patients with COPD with moderate-to-severe airflow obstruction and mild hypoxemia at rest by improving exercise tolerance and reducing pulmonary hypertension during exercise (
26).
When energy cost studies are not available, maximum exercise tolerance may be estimated from pulmonary function data (
27). A 3-, 6-, or 12-minute walk test can also provide useful information. The patient is instructed to gradually increase walking speed and duration on subsequent walking tests. The test is simple and may be performed daily in the hospital or at home (
28).
Any motivated COPD patient who has respiratory symptoms that limit activities of daily living (ADL) and who has adequate medical, neuromusculoskeletal, financial, and psychosocial status to permit active participation is a candidate for rehabilitation. Active patients who are still able to walk several blocks but who have noted yearly decreases in exercise tolerance or who have recently begun to require ongoing medical attention for pulmonary symptoms or complications are ideal candidates.
Therapeutic Interventions
Medications
The patient’s medical regimen is optimized prior to reconditioning exercise. Bronchodilators are delivered as aerosolized solutions but are not effective if the patient deposits the medications uselessly on the tongue. COPD patients require training in the use of “spacers” and nebulizers (
35). Orally administered β agonists are used when aerosolized medications are ineffective or when metered-dose inhaler cannot be
efficiently used. One half to two thirds of 33 double-blind, randomized, placebo-controlled studies showed significant positive effects of anticholinergics and short-acting β-2 mimetics (especially salbutamol), respectively, on exercise capacity.
Early medical attention is important during intercurrent respiratory tract infections (
36). Antibiotics, glucocorticoids, and adjustment of bronchodilators and mucolytic agents may be indicated.
N-acetylcysteine at 1,200 mg/d was demonstrated in a randomized, double-blind, placebo-controlled study to normalize C-reactive protein levels, lung function, and symptoms during acute exacerbations and possibly in preventing the exacerbation (
37).
Counseling and General Medical Care
Dyspnea often causes fear and panic. This may worsen tachypnea while increasing dead-space ventilation, the work of breathing, hyperinflation, and air trapping. Relaxation exercises, such as Jacobson exercises and biofeedback (
38,
39), yoga, and diaphragmatic and pursed-lip breathing, can be used to decrease tension and anxiety.
COPD patients perceive impairment in quality of life. Depression has been reported in 50% of patients, and there is often severe reduction in social interaction (
40). Integrating psychosocial support with multimodal pulmonary rehabilitation optimizes intervention (
41). Loss of employment and physical independence may also need to be addressed.
COPD patients tend to overuse medications during periods of respiratory distress and underuse them otherwise. They are counseled on adhering to their medication regimens (
42), and on avoiding atmospheric or vocational pollutants and other aggravating factors, such as pollen, aerosols, excessive humidity, stress, and respiratory tract pathogens. Yearly flu vaccinations are recommended; and pneumococcal vaccines are used one time or every 5 to 10 years for high-risk cases.
High-altitude travel may require an additional 0.5 L/min of supplemental oxygen administration for those already requiring supplemental oxygen; otherwise, oxygen therapy generally need not be used for short flights (
43). Good hydration should be maintained with ample fluid intake.
Nutrition
Significant weight loss occurs in 19% to 71% of COPD patients (
18). In a study of 255 stable COPD pulmonary rehabilitation patients, depletion of body weight, fat-free mass, and muscle mass was noted in 40% to 50% of patients with chronic hypoxemia and in normoxemic patients with FEV
1 < 35% (
44). In one study, 30 of 50 consecutive COPD patients presenting with ARF were significantly undernourished, and impaired nutritional status was more prevalent in those patients requiring mechanical ventilation (74% vs. 43%) (
45).
Undernutrition has been associated with an increased susceptibility to infection that is due in part to impaired cell-mediated immunity, reduced secretory immunoglobulin A, depressed pulmonary alveolar macrophage function, and increased colonization and adherence of bacteria in the upper and lower airways. Patients with significant nutritional impairment are more frequently colonized by
Pseudomonas species (
46,
47). In addition, malnutrition can adversely affect lung repair, surfactant synthesis, control of ventilation and response to hypoxia, respiratory muscle function and lung mechanics (
48), and water homeostasis. It can lead to respiratory muscle atrophy and decreased exercise capacity, cor pulmonale, increased rate of hospitalization for pulmonary-related problems, hypercapnic respiratory failure, and difficulty in weaning from mechanical ventilation (
45,
49,
50). Likewise, inappropriate nutrition, such as increasing carbohydrate intake, can exacerbate hypercapnia.
Short-term refeeding of malnourished patients can improve respiratory muscle endurance and increase respiratory muscle strength in the absence of demonstrable changes in skeletal muscle function (
51). Because of bloating due to a low diaphragm, patients are advised to take small mouthfuls of food, eat slowly, and take smaller and more frequent meals. SpO
2 can be evaluated while eating. If desaturation occurs, supplemental oxygen is used or increased. For those with hypercapnia, a dietary regimen high in calories derived from fat can decrease hypercapnia. Although short-term refeeding can be beneficial, refeeding programs lasting more than 2 weeks have not consistently resulted in increases in body weight. Growth hormone has not been shown to be useful. Possible beneficial effects of anabolic steroids as adjuncts to nutritional support and exercise have been reported to increase lean body mass and promote weight gain (
52,
53,
54).
Breathing Retraining
Shallow, rapid breathing is commonly seen in anxious, dyspneic patients. This increases dead-space ventilation and airflow through narrowed airways, increasing the flow work of breathing. Patients with chronic airflow obstruction also have an altered pattern of ventilatory muscle recruitment in which the most effective ventilatory pressure is generated by the rib-cage inspiratory muscles rather than by the diaphragm, with significant contribution by primarily expiratory muscles (
55). Diaphragmatic breathing and pursed-lip exhalation can help to reverse these tendencies. These techniques are usually initiated in the supine or 15% to 25% head-down position. Diaphragmatic breathing is guided by having the patient place one hand over the abdomen and the other on the thorax just below the clavicle. Breathing deeply through the nose, the abdomen is distended forward as appreciated by movement of the hand on the abdomen. Movement of the rib cage and, thus, the hand on the thorax should be kept to a minimum. Small weights can be placed on the abdomen to provide some resistance training and enhance the patient’s focus. During exhalation, the abdominal muscles and the hand on the abdomen compress the abdominal contents, and exhalation is via pursed lips (
56). Classically, a lighted candle is put several feet in front of the patient, and the patient flickers the flame while exhaling. This equalizes pleural and bronchial pressures, preventing collapse of smaller bronchi and decreasing air trapping. Diaphragmatic and pursed-lip breathing decreases the respiratory rate, coordinates the breathing pattern, and can improve blood gases (
57). It is used during routine ADL and exercise. It can improve exercise performance by relaxing accessory muscles and improving breathing efficiency.
Air-shifting techniques may be useful to decrease microatelectasis. Air shifting involves taking a deep inspiration that is held with the glottis closed for 5 seconds, during which time the air shifts to lesser-ventilated areas of the lung. Expiration is via pursed lips. This technique may be most beneficial when performed several times per hour.
Airway Secretion Elimination
Airway secretion clearance is crucial because exacerbations of COPD are caused by trapping of airway secretions in the peripheral airways. The patient’s cough may be weak or ineffective as a result of increased airway collapse in more central airways, and frequent bouts of coughing are fatiguing. The high expulsive pressures generated during coughing can exacerbate both air trapping and secretion retention. “Huffing,” or frequent short expulsive bursts following a deep breath, is often an effective and more comfortable alternative to coughing. Chest percussion and postural drainage can be useful for patients with chronic bronchitis or others with greater than 30 mL of sputum production per day (
58), although caution must be taken to increase oxygen delivery as necessary during treatment. Autogenic drainage involves breathing with low tidal volumes between the functional residual capacity and the residual volume to mobilize secretions in small airways. This is followed by taking increasingly larger tidal volumes and forced expirations to transport mucus to the mouth (
59).
Application of positive expiratory pressure (PEP) breathing is based on the theory that mucus in small airways is more effectively mobilized by coughing or forced expirations
if alveolar pressure and volume behind mucous plugs are increased. PEP is applied by breathing through a face mask or a mouthpiece with an inspiratory tube containing a one-way valve and an expiratory tube having variable expiratory resistance. Expiratory pressures of 10 to 20 cm H
2O are maintained throughout expiration. PEP increases functional residual capacity, reducing resistance to airflow in collateral and small airways (
60,
61). Studies on the clinical benefits of PEP breathing have been inconclusive for both cystic fibrosis (CF) and COPD (
62,
63,
64,
65,
66,
67,
68,
69,
70).
Flutter breathing is a combination of PEP and oscillation applied at the mouth. The patient expires through a small pipe. A small stainless steel ball rests on the expiratory end of the pipe; it is pushed upward during expiration, producing PEP, and falls downward again, interrupting flow. The mucus-mobilizing effect is thought to be due to widening of the airways because of the increased expiratory pressure and airflow oscillations due to the oscillating ball (
71). For this too, however, the results of clinical trials have been conflicting (
72,
73,
74,
75,
76).
With currently available technology, mechanical vibration or oscillation can be mechanically applied to the thorax or directly to the airway to facilitate airway secretion elimination. Vibration is possible at frequencies up to 170 Hz applied under a soft plastic shell to the thorax and abdomen (the Hayek Oscillator, Breasy Medical Equipment Inc., Stamford, CT). Another device delivers rapid burst airflows at up to 25 Hz under a vest covering the chest and upper abdomen (THAIRapy System, American Biosystems, Inc., St. Paul, MN). The effects of mechanical chest percussion and vibration appear to be frequency dependent (
77,
78,
79). In most animal studies, frequencies between 10 and 15 Hz appear to best facilitate mucous transport (
77,
79,
80), especially the transport of a thicker mucous layer (
81). Warwick and Hansen found long-term increases in forced vital capacity (FVC) and forced expiratory flows for CF patients treated with high-frequency chest-wall compression as compared with manual chest percussion alone (
82). Others have reported improvement in pulmonary function and in gas exchange during high-frequency oscillation (
83,
84,
85,
86,
87), and Sibuya et al. found that chest-wall vibration decreased dyspnea (
86). Most studies on COPD and CF patients, however, have failed to demonstrate objective clinical benefits from percussion or vibration on mucous transport (
87,
88,
89,
90). Side effects of percussion and vibration can include increasing obstruction to airflow (
91,
92). In an animal model, the application of vibration and percussion was also associated with the development of atelectasis (
93). Despite conflicting studies, the THAIRapy Vest has become popular for CF and familial dysautonomia patients, and studies have claimed decreases in hospitalization rates with its daily use (
77). Patients with daily airways secretion encumbrance usually feel that its use is beneficial.
The Percussionator (Percussionaire Corp., Sandpoint, ID) can deliver aerosolized medications while providing high-flow percussive minibursts of air directly to the airways at rates of 2.5 to 5 Hz. This intrapulmonary percussive ventilation has been reported to be more effective than chest percussion and postural drainage in the treatment of postoperative atelectasis and secretion mobilization in COPD patients (
94,
95). The majority of such patients feel that it is helpful (
96,
97).
Patterson et al. found in a 10-year study that good CF patient compliance with airway secretion mobilization methods was associated with a slower rate of loss of pulmonary function (
98). Patient compliance is usually poor, however (
99,
100,
101). There is greater patient compliance for simple methods that can be used independently. Little has been documented concerning long-term safety and efficacy of any of these methods. Because expensive methods have not been shown to be more effective than simple handheld percussors costing about $400 (Jeannie Rub Percussor, Morfan Inc., Mishawaka, IN [
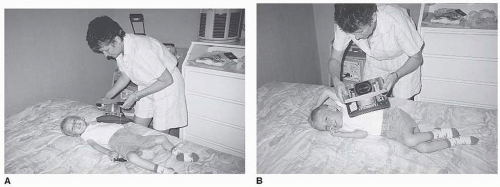
Fig. 42-1] or NeoCussor General Physical Therapy, St. Louis, MO), the latter should be favored for routine clinical use.
Inspiratory Resistive Exercises
Inspiratory resistive exercises, including maximum sustained ventilation, inspiratory resistive loading, and inspiratory threshold loading, can improve the endurance of respiratory muscles (
102,
103,
104). Typically, patients breathe through these devices for a total of 30 minutes daily for 8 to 10 weeks. The settings of the devices are adjusted to increase difficulty as patients improve and the program advances.
Levine et al. conducted an evaluation of the isocapnic hyperpnea method and determined that no more benefits could be derived from it than could be achieved using periodic intermittent positive pressure breathing treatments, a regimen that was considered equivalent to placebo (
105). However, Ries and Moser randomly assigned 18 patients to either a home isocapnic hyperventilation training program or a walking program and found that the former led to improvements in ventilatory muscle endurance and exercise performance and significant improvements in the maximum rate of oxygen consumption (VO
2max), whereas walking exercises improved lower limb exercise endurance but not ventilatory muscle endurance (
106).
Twenty-one controlled studies of inspiratory resistive loading involving 259 COPD patients reported improvements in inspiratory muscle strength and endurance (
107). The mean increase in maximum inspiratory pressure was 19%. However, the subjects using inspiratory resistance training reduce their inspiratory flow rates and lengthened their inspiratory time to reduce the severity of the imposed loads. Thus, “targeted” or threshold inspiratory muscle training is recommended over flow-resistive training to assure adequate intensity of inspiratory muscle activity.
With targeted training, the subject is provided feedback regarding the inspiratory flow rates through the resistor or the inspiratory pressure generated by flow through the resistor; with threshold training, the subject is unable to generate flow through the device until a predetermined pressure is achieved. Six of the nine controlled studies of the use of targeted or threshold resistor devices in COPD reported significantly greater improvements in inspiratory muscle function in the subjects than in the controls (
107). In three of the six studies in which it was assessed, exercise tolerance was greater for trained subjects than for controls. In one controlled study comparing exercise reconditioning plus threshold inspiratory muscle training with exercise reconditioning alone, the former resulted in significantly greater increases in inspiratory muscle strength and endurance and in exercise tolerance (
108). Exercise tolerance seemed to be improved particularly for those with electromyographic changes indicating inspiratory muscle fatigue with exercise (
109). One controlled, well-designed, but small study of threshold inspiratory exercise for CF patients demonstrated significant improvements in inspiratory muscle strength, FVC, total lung capacity, and exercise tolerance in the experimental group (
110). In another controlled study of patients taking corticosteroids, inspiratory muscle training appeared to prevent the weakness that would have otherwise resulted from the steroid use (
111). The combination of inspiratory muscle training along with bronchodilator therapy and reconditioning exercise was demonstrated to very significantly reduce dyspnea by comparison to the use of bronchodilators and general exercise without inspiratory muscle training (
112). A recent study showed benefit incorporating inspiratory muscle training into a pulmonary rehabilitation program (
113). In general, improvements in inspiratory muscle function and in exercise tolerance were greater for the targeted and threshold studies than for the flow-resistor studies (
114).
Respiratory Muscle Rest
Relatively minor changes in the pattern of breathing or respiratory muscle loading can trigger acute respiratory muscle fatigue and failure. Interspersing periods of exercise and muscle rest is a basic principle of rehabilitation. Hypercapnia is an indication of limited reserve before the appearance of overt fatigue and may indicate the need for periods of respiratory muscle assistance or rest before considering strengthening exercises (
115). Diaphragm rest can be achieved by assisted ventilation using either body ventilators, mouth piece, or nasal noninvasive positive pressure ventilation (NIV).
Despite high ventilation rates in COPD, ventilatory response to both hypercapnia and hypoxia may be reduced. This is often exacerbated during sleep. The increase in pulmonary vascular resistance that occurs in the presence of pulmonary tissue hypoxia is exacerbated by acidosis. When this situation becomes severe, it may lead to right ventricular failure. The use of oxygen therapy alone may exacerbate CO2 retention and acidosis.
Two groups of patients may be suited to ventilatory assistance at home. The first and smaller group includes those who use ventilatory assistance around the clock, usually by tracheostomy, but who are medically and psychologically stable. These patients tend to require frequent hospital readmission, have a poorer prognosis than ventilator-assisted individuals with NMD, and can be candidates for decannulation to NIV. The second group may benefit from nocturnal assistance alone.
While both nocturnal negative pressure body ventilator (NPBV) use and NIV can normalize arterial blood gases, and have been reported to increase quality of life, 12-minute walking distance, respiratory muscle endurance, and decrease dyspnea (
116), the former methods cause obstructive apneas during sleep (
117,
118). The NIV methods, provided by portable ventilators and bilevel positive airway pressure (BiPAP) machines, can rest inspiratory muscles, assist ventilation, and splint open the airway to prevent sleep apneas and airway collapse (
119).
Belman et al. reported greater diaphragm relaxation by nasal ventilation than by use of NPBVs (
120). Marino demonstrated reversal of nocturnal ventilatory insufficiency for COPD patients using nasal ventilation (
121), and others have used assisted ventilation via oral-nasal interfaces as an alternative to intubation and tracheostomy for COPD patients in acute exacerbation (
122). Nasal BiPAP has the additional benefit of the expiratory positive airway pressure countering auto—positive end-expiratory pressure (PEEP) in these patients
who trap air. This decreases their work of breathing. A number of studies have reported long-term improvements in daytime blood gases with the use of nocturnal nasal ventilation for hypercapnic COPD patients (
116,
123,
124), and it has been suggested that nocturnal ventilator use can also decrease dyspnea, improve quality of life (
125), and improve survival (
123). Nocturnal nasal BiPAP was also reported to improve sleep efficiency and total sleep time in hypercapnic COPD patients (
126). In another study of 49 hypercapnic patients with COPD, while hospitalization rates were decreased by both long-term oxygen therapy (LTOT) and by LTOT with nocturnal nasal ventilation by BiPAP, only the latter group had a significant decrease in intensive-care admissions and a significant improvement in 6-minute walk distance (
127). However, a systematic review (
76) of nocturnal noninvasive positive pressure ventilation of at least 3 months duration in stable hypercapnic COPD patients did not find a consistent clinically or statistically significant effect on lung function, gas exchange, respiratory muscle strength, sleep efficiency, or exercise tolerance. However, these conclusions are limited by the small size of the underlying studies. Although it is widely considered appropriate to offer nocturnal BiPAP for hypercapnic COPD patients, little or no benefit has been reported with nocturnal use for nonhypercapnic patients for whom its role remains controversial (
128). Use of proportional assist ventilation and pressure support during exercise has been reported to facilitate high-intensity exercise training in severe COPD (
129,
130,
131). Patients benefiting from proportional assist ventilation were reported to achieve 15% higher exercise levels at 6 weeks than those exercising without it. Users had a significant reduction in plasma lactate concentration at equivalent workloads after training.
Supplemental Oxygen Therapy
Supplemental oxygen therapy is indicated for patients with pO
2 continuously less than 55 to 60 mm Hg (
132). Home oxygen therapy can decrease pulmonary hypertension, polycythemia, and perception of effort during exercise, and it can prolong life (
132,
133). Patients with COPD have also been shown to have increased sympathetic modulation and reduced baroreflex sensitivity. Supplemental oxygen has been shown to significantly and favorably alter autonomic modulation and decrease blood pressure and pulse (
134). In addition, cognitive function can be improved, or at least, better maintained, and hospital needs reduced.
An international consensus on the current status and indications for LTOT suggested that the prescription be based on (
135):
An appropriately documented diagnosis
Concurrent optimal use of other rehabilitative approaches, such as pharmacotherapy, smoking abstinence, and exercise training
Properly documented chronic hypoxemia
Oxygen therapy should be given with caution to hypercapnic patients whether or not they are using NIV (
136).
There can also be need for supplemental oxygen during exercise. Many patients exhibit exercise hypoxemia. Decreases in SpO2 are noted at physical activity levels comparable to those necessary to perform ADL. Often, the decrease in SpO2 occurs within the first minute, after which SpO2 stabilizes; but occasionally there is a progressive decline in SpO2 with exercise.
In a study of 38 subjects in whom the mean resting SpO
2 was 93 ± 3%, a decrease in SpO
2 of 4.7 ± 3.6% (range: 1% to 18%) was observed during submaximal exercise (
137).
In a crossover study of 12 subjects with severe COPD (
138), four patients more than doubled their duration of exercise while receiving 40% oxygen, but in only two of these was desaturation observed in the absence of oxygen. Bradley et al. reported that in subjects with mild hypoxemia and exercise desaturation, supplemental oxygen by nasal prongs did not influence maximum work rate but did influence endurance (
139). Davidson et al. noted that oxygen increased mean walking endurance time by 59% and 6-minute walking distance by 17%. Moreover, submaximal cycle time at a constant workload was increased by 51% at a flow rate of 2 L/m and by 88% at 4 L/m, suggesting a dose-response curve (
140). The exercise response to oxygen could not be predicted from the degree of desaturation, resting pulmonary function tests, echocardiographic measurements of right ventricular systolic pressure, or other clinical parameters (
138). In fact, in nonhypoxemic COPD patients performing moderate exercise, oxygen supplementation decreases ventilatory requirement by its direct effect on chemoreceptor inhibition (
141). Thus, exercise tolerance can be increased by oxygen therapy without improving oxygen consumption or utilization. A recent study found that supplemental oxygen during exercise prevented exercise induced oxidative stress (
142). Marcus et al. also reported significantly greater exercise tolerance in CF patients receiving oxygen (
143). A recent study found improved exercise tolerance in CF patients in the Dead Sea basin compared with at sea level (
144). This was thought to be due to the increased oxygen tension below sea level.
The most widely accepted guideline for prescribing oxygen use during exercise is that of exercise-induced SpO
2 below 90%. However, it seems reasonable to recommend that measurements of dyspnea and exercise tolerance be undertaken with and without supplemental oxygen to determine which individuals are less short of breath or walk further (have greater exercise tolerance) when given supplemental oxygen (
145). Certainly, exercise-induced decreases in SpO
2 below 90% when combined with increased exercise tolerance with oxygen therapy warrant the prescription of oxygen therapy during exercise.
Patients with mild-to-moderate daytime hypoxemia often have marked nocturnal desaturation. Home overnight oximetry can be used to diagnose nocturnal oxyhemoglobin desaturation and assist in oxygen prescription although guidelines for sleep supplemental oxygen have not been established (
146).
Inspiratory phase or pulsed oxygen therapy, especially when delivered transtracheal, avoids waste and decreases discomfort and drying of mucous membranes. Oxygen flow
delivery is 0.25 to 0.4 L/min compared to 2 to 4 L/min when delivered via nasal cannula or face mask (
147,
148). Oxygen therapy should be used in combination with mechanical ventilation for patients with concomitant carbon dioxide retention.
Reconditioning Exercise
COPD patients are markedly inactive during and after hospitalizations for acute exacerbations. Those with low activity levels 1 month postdischarge were significantly more likely to be hospitalized during the next year. Patients who had hospitalizations for exacerbations in the previous year were even more deconditioned than patients with recent hospitalizations. Thus, efforts to enhance physical activity and exercise tolerance are especially important for patients experiencing acute exacerbations (
149).