17 Rehabilitation
Improving Outcomes for Patients Following Fractures of the Proximal Femur
Fracture of the proximal femur is a common and catastrophic event that frequently occurs in older people. For those who previously functioned independently, a proximal femur fracture may mean a loss of independence, and for frail elderly patients, the fracture may result in the permanent loss of their ability to live in their own home.1–3 Proximal femur fractures are the most common type of injury requiring hospitalization among persons 65 years old and older. There is an associated high in-hospital mortality rate, and the mortality rate remains consistently high at 1 year after fracture.4,5 Despite improvements in surgical procedures and rehabilitation interventions, a proximal femur fracture remains uniquely challenging for patients and families, for the many health care professionals who provide care, and for the already overburdened health care system.3,6–10 For patients, these unique challenges include learning how to navigate the continuum of care and understanding what to expect in terms of treatments and discharge plans. For health care providers, the challenges revolve around optimizing communication and easing transitions for patients across various health care settings.
Successes through collaborative efforts include the development of proximal femur fracture clinical guidelines and integrated models of care based on best clinical practice. These approaches address both the physical needs and the cognitive needs of patients, and they combine orthopaedic and geriatric care principles to provide structured rehabilitation approaches across the health care continuum.3,10,11 These innovative systems approaches are reframing rehabilitation by establishing principles of care that improve access and patient flow across the health care continuum, set expectation for optimal clinical care through a coordinated orthopaedic and geriatric approach, ensure the consideration of patients’ needs for secondary prevention, and facilitate and measure health care system improvements by using a structured performance measurement system.3,10–12
Issues in Rehabilitation Care for Patients with a Fracture of the Proximal Femur
Rehabilitation care for patients following a proximal femur fracture care is challenging as patients engage in a complex journey influenced by several issues. These issues include the patients’ characteristics, the coordination of the health care services across hospitals and the community, and the significant health care system costs related to the patient’s rehabilitation needs.3,10,12
Patient Characteristics
Patients experiencing fractures of the proximal femur tend to be older, and thus their care frequently includes the management of a range of complex geriatric issues. Patient characteristics are known to affect functional and cognitive gains significantly and are primary indicators of rehabilitation outcomes after proximal femur fracture.12 Specific characteristics known to influence outcomes include: age, specifically for those who are 80 years old and older and are frail7; comorbid conditions13; poor nutritional status9; social support14; prefracture cognitive function8; depression15,16; and postoperative delirium.17 In addition, although it is not a predictor of rehabilitation outcomes, osteoporosis is a significant and common condition of the bone that contributes to bone fragility. Osteoporosis is often left untreated, a situation that contributes to increased numbers of proximal femur fractures and the occurrence of future fractures.10,18
Cognitive impairment may be exhibited as delirium, it may reflect preexisting dementia, or it may be complicated by depression. Cognitive impairment occurs in approximately 17% of patients with proximal femur fracture. Further unknown numbers of patients with cognitive deficit are identified at the time of admission to the hospital.1,17,19 Delirium, dementia, and depression significantly influence rehabilitation gains and are known to affect the hospital length of stay (LOS).19–21 Moreover, delirium, dementia, and depression15 are shown to influence discharge disposition and to affect issues related to a patient’s previous living situation (i.e., living alone or with others)22 and the presence of social support.14
Health Care Services Issues
Health care services for people with a fracture of the proximal femur are traditionally fragmented and limited.3,11,23 Patients undergo a complex journey through the health care system that may include the emergency department, the surgery department, the acute orthopaedic unit, and then, depending on the patient’s circumstances and the services available, discharge home, transfer to an inpatient rehabilitation option, or, often, direct placement in a long-term care facility without the opportunity for rehabilitation.3,23
Inpatient rehabilitation options for patients are variable and are found in several settings, including acute care hospitals, rehabilitation hospitals, specialized geriatric units, subacute longer-term units, and convalescent units in long-term care facilities.11,24 A Cochrane review25 meta-analysis considered four models for proximal femur fracture rehabilitation and compared usual orthopaedic care with several approaches combining orthopaedics, geriatric, and interprofessional care. Results indicated that although evidence was limited with respect to the effectiveness of specific individual inpatient rehabilitation programs, evidence was sufficient to determine that older people with proximal femur fractures had better recovery when they were cared for in an interprofessional team environment that included specialist geriatric support.
Access to inpatient rehabilitation settings is variable and often limited. Patients with proximal femur fracture are usually older and have frailties, comorbidities, and cognitive issues of delirium, dementia, and depression. Cognitive issues become critical barriers when rehabilitation settings select higher-functioning patients.21,23 There is a misconception that older patients are unable to benefit from rehabilitation approaches, and these patients are therefore denied access to rehabilitation. This misconception occurs despite strong evidence that patients with proximal femur fracture benefit most from targeted structured rehabilitation opportunities focused on improving self-care and motor function.1,23,24,26–28
Access to rehabilitation settings is also influenced by weight-bearing status and by the ability to engage in early mobilization. In the past, common surgical procedures demanded long periods of non–weight bearing postoperatively for older persons, a situation that seriously limited a patient’s engagement in rehabilitation activities. Advances in surgical procedures support immediate weight bearing and thus facilitate earlier mobility and rehabilitation.29 Access to rehabilitation is essential for older persons following a proximal femur fracture. Without rehabilitation, many patients who were previously managing the activities of daily living independently do not return home, and instead needlessly experience direct, permanent, and costly admissions to long-term care facilities.23,22,30
Cost of Care
Care for patients following a fracture of the proximal femur is costly. The main determinants of hospital costs are expenses related to the surgical procedures and the hospital LOS. However, other costs such as the community supports needed on discharge, as well as long-term care for those requiring permanent placement, also need to be considered.3,21 In Canada, the annual economic burden of proximal femur fracture was estimated to be $650 million in 1996/97. With an aging population, this economic burden is expected to rise to 2.4 billion by 2041. In Canada, direct health care system costs are approximately $27,000 for each patient. These costs may be as low as $21,000 for patients discharged home and as high as $47,000 when a patient requires long-term care placement.21 With population projections indicating that more people will survive to an age at which proximal femur fractures are common, the disease burden and health care resources required for necessary community care and long-term care will be enormous.31,32 There are clear health system cost benefits in achieving system efficiencies through a coordinated systems approach to care that includes reductions in LOS, appropriate rehabilitation, and the supports necessary for patients to return home successfully.
Reframing Rehabilitation Across the Health Care Continuum
Advances in the care of proximal femur fractures are emerging through collaborative efforts to develop clinical guidelines and integrated models of care.3,10,12 These approaches are systematically developed to reframe rehabilitation care across the health care continuum by using evidence-based practices for optimal clinical care combining orthopaedic and geriatric principles, interprofessional management, and efficient patient flow. These approaches are integrated and work to improve both the quality and cost-effectiveness of care.3,10,11 Several specific approaches are described in the following subsections.
SIGN Guidelines for the Prevention and Management of Hip Fracture in Older Persons
The Scottish Intercollegiate Guidelines Network (SIGN)3 has a strong record of developing evidence-based guidelines including the SIGN Guidelines Number 56, Prevention and Management of Hip Fractures in Older Persons. This guideline details the “journey of care” for patients with a proximal femur fracture and uses evidence at each stage. A summary of key recommendations for improved patient care and flow across the system include the following: (1) early formal assessment within 2 hours of transfer to the inpatient unit; (2) early access to surgery within 24 hours of admission; (3) interprofessional team collaboration to facilitate early rehabilitation; (4) transfer to a geriatric orthopaedic rehabilitation unit for those patients with comorbidities, poor functional ability, and cognitive issues; (5) early supported discharge; and (6), overall median reduction in the hospital LOS.3 Specific clinical practices are also highlighted. For example, femoral traction should not be used, and preoperative antibiotic prophylaxis should be administered routinely.3 Finally, a national hip fracture audit system is strongly supported. This system monitors progress with established indicators that allow for comparisons between “what is happening” and “what ought to happen” and supports continued improvement in the quality of care.3,33
“Blue Book” for the Care of Patients with Fragility Fractures
The British Orthopaedic Association10 and the British Geriatric Society collaborated to develop the “Blue Book” for the care of patients with fragility fractures to summarize current best practices in the care and secondary prevention of fragility or proximal femur fractures.10 The key elements featured were (1) prompt admission to orthopaedic care, (2) rapid comprehensive assessment, (3) minimal delay to surgery, (4) accurate and well- performed surgical repair, (5) prompt mobilization, (6) early interprofessional rehabilitation, and (7) early supported discharge and ongoing community rehabilitation. In addition, osteoporosis management and secondary prevention of fragility fractures were strongly supported in these guidelines, and recommendations included active assessment and management of bone protection and falls prevention. Prominently featured is an audit system that uses the National Hip Fracture Database, a Web-based system to monitor and promote best practices in the care and secondary prevention of fractures.10
Total Joint Network Integrated Model of Care
The Total Joint Network,11 through a partnership of 35 organizations (acute and rehabilitation hospitals and other partners including the local programs for geriatrics, osteoporosis, arthritis, and the rehabilitation network) across the Greater Toronto Area, came together from December 2005 to April 2008 to develop an integrated model of care for patients following a hip fracture.11,34 The model of care design featured improved postoperative management of patients by coordinating acute care, inpatient rehabilitation, and community care across the health care continuum to enable patients to succeed in their return to their prefracture situation. A key objective of the model was to ensure that patients were able to return home. The model is summarized as providing the following: (1) optimized acute care through a clinical pathway; (2) new access to intensive inpatient rehabilitation by postoperative day 5 for all patients coming from the community regardless of cognitive issues; (3) rapid assessment through a rehabilitation clinical pathway (initial 7- to 10-day period) using assessment, patient-centered goals, treatment, evaluation, and discharge (ACTED) approaches that highlight geriatric management principles; (4) ongoing intensive rehabilitation; and (5) standardized discharge planning focused on returning patients to their homes.11,12
Implementation of the model at all 35 health care sites occurred over an 18-month period and included development of hospital and community partnerships, targeted education on delirium and dementia, and feedback using performance indicators. Findings over 1 year indicated system efficiencies that included reductions in LOS for acute care, new and timely access for patients into inpatient rehabilitation, and for most patients (>80%) new opportunities to return home rather than being streamed into long-term care.12
Model of Care for Patients with a Hip Fracture
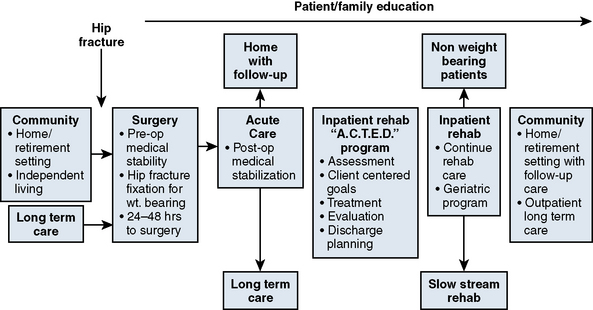
Building on the successes of these international collaborative efforts, the Orthopaedic Expert Panel for Ontario, Canada, developed a provincial model of care for patients with a hip fracture. This integrated model of care promotes optimal rehabilitation care and efficient flow of patients across the health care continuum. The primary outcome is to return a patient to his or her prefracture setting (for most patients this is home) or to ensure a smooth transition into the most appropriate care setting. Key elements include the following: (1) timely surgery within 48 hours of admission to hospital; (2) surgical repair that optimizes functional recovery that allows weight-bearing and early mobilization; (3) an optimized acute care clinical pathway that transitions medically stable patients, not yet ready to return home, to inpatient rehabilitation on postoperative day 5; (4) acceptance of medically stable patients with proximal femur fracture into inpatient rehabilitation programs, regardless of cognitive issues or complex social situations; (5) an optimized rehabilitation clinical pathway for rapid assessment and treatment during the initial 7- to 10-day period using the ACTED model of care; (6) ongoing intensive optimized rehabilitation care; (7) transition to other slow-stream rehabilitation options for patients who may require longer stays; (8) standardized discharge planning that focuses on returning home with community supports; (9) best practices in management of secondary prevention issues of osteoporosis and falls management; and (10) facilitation of system data tracking to measure patient access and flow across the system by using predefined targets.35 Figure 17-1 provides a visual overview of the model and the flow for patients across the health care continuum.
Principles of Optimized Rehabilitation Care
Access and Patient Flow Across the Health Care Continuum
Timely Surgery
Access to timely surgery is crucial for patients following a proximal femur fracture. Limited access is frequently linked to significantly higher rates of mortality and also contributes to increased morbidity and subsequently reduced success in rehabilitation.4,5,17,36 Studies have suggested that for each day surgery is delayed, the risks that the patient will die in hospital increase, and operative delays beyond 48 hours approximately double the risk that the patient will die before the end of the first postoperative year.4,37
Surgery is delayed in these patients for many reasons. Frequently, patients have preexisting medical conditions that first need to be stabilized. However, many underlying and often correctable process issues exist and contribute to surgical delays, including wait times for consultations, lack of available surgical time, waits for bed availability, and inadequate access to the necessary resources for surgery.3
Transition Between Services
Transitions between services in patients with proximal femur fracture may occur at multiple points along the health care continuum. Although these transitions occur frequently within the same health care organization, in many instances patients also move between organizations. The most common transitions are transfers from the initial referring hospital to the regional orthopaedic center, from acute care to rehabilitation services, and from the hospital to the community. Delays in transitions are stressful for patients and their families and contribute to poor rehabilitation outcomes.12,17 Specific processes need to be designed to support successful and seamless transitions that contribute to care and maximize efficiencies.10,11
At the time of transfer, the patient’s medical status must be clearly represented and meet the criteria for admission to the subsequent service and will avoid the return of the patient back to the previous service for stabilization.11,23 Medical stability during rehabilitation is well defined for patients with proximal femur fracture and includes stable vital signs; an intact surgical incision with no drainage; no signs or symptoms of infection; no evidence of anemia; and a patient who is voiding, tolerating the diet well, and receiving and responding well to medications.11,23
Effective and positive communication needs to occur at several levels to facilitate effective patient transitions between services. At the senior management level, formal relationships through memorandums of agreement or more informal repatriation principles have been demonstrated to facilitate smooth transitions and support the development of a regional systems approach to patient flow between organizations and services.11 Similarly, at the clinical level there needs to be effective communication and sharing of relevant patient information between the transferring and receiving services. Unfortunately, strong evidence suggests that this is information that is not consistently provided, therfore standardized transfer forms are recommended and have been demonstrated to be useful tools.11,23,38 Furthermore, well-developed clinician relationships are helpful to create a comfort level to “pick up the phone” to obtain information, solve problems, and clarify patient issues.11
Discharge Planning
Discharge planning is the responsibility of all the team members in an interprofessional team including physical therapists, occupational therapists, social workers, nurses, and physicians. Discharge planning starts with the initial assessment on the patient’s arrival in the emergency department. Social, physical and cognitive assessments must also be completed to identify the patient’s prefracture abilities. In addition, information is collected about a patient’s home environment and any preexisting support services provided by caregivers or family members before the patient’s fracture.3 By gathering information on a patient’s previous level of function, including cognitive status, and social involvement, the health care team will be able to establish the most appropriate goals for successful discharge. Throughout the initial assessments, the patient and family should be informed of the care plan following a proximal femur fracture, including the targeted LOS,11 so that patients have the opportunity to discuss potential discharge issues with the team. Identifying this plan early in the care process will facilitate planning3 for the rehabilitation team and will allow maximum time to make preparations for a home-supported discharge. For the few patients identified as unable to return to their prefracture setting, there will be the opportunity to make an alternate arrangement for placement.11
For patients who sustain a proximal femur fracture and are cognitively alert and medically well, rehabilitation needs to be planned for a short LOS and discharge from the acute care unit. These patients often do well postoperatively. They increase their mobility and functional tolerances quickly and achieve early discharge with the social services provided through the community.3
Patients whose conditions are more complex and who present with cognitive issues or limited mobility or low tolerance require a more comprehensive rehabilitation program and will require a longer LOS with a more intensive rehabilitation plan. To facilitate future discharge planning, patients and families need to be made aware of the program care path that the patient will follow. For example, in the Ontario model, patients and families are informed that all patients with proximal femur fracture are admitted to acute care hospitals and that they (1) will receive surgical care within 48 hours, (2) will be transferred to a rehabilitation unit when they are medically stable (on postoperative day 5), and (3) will be discharged home with home care services when they are functionally able (with an average 24-day LOS).11 This approach facilitates confidence in patients and families and allows them the opportunity to plan.
Before a patient’s discharge from hospital, services need to be coordinated in the community, and sufficient notice must be given to allow the patient and caregivers time to make arrangements and to set up the care for the patient’s return home. Educational information on medication, mobility, expected progress, and pain control should be given to the patient, caregiver, and families. A schedule of appointments, as well as relevant contact information, must also be provided to ensure that the patient and caregivers are able to access the necessary ongoing care.3
If any question exists about the patient’s safety and ability to function at home, related either to the home environment or to the functional recovery of the patient, a home visit can be completed by a rehabilitation staff member such as an occupational therapist or a physical therapist. For patients who present with cognitive issues, this assessment can be very insightful because the patient’s functional level may well improve once the patient returns to the more familiar home environment.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree